HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Early Bird Registration Discount Expires July 11 for HMA Conference on The Future of Publicly Sponsored Healthcare, October 10-11 in Chicago

- California Extends Medicaid Coverage to Undocumented Residents

- Colorado Receives Federal Approval to Establish Standardized Exchange Plan Option

- Hawaii to Restore Medicaid Dental Benefits to Adults in 2023

- Indiana Awards MMIS Maintenance, Operations Contract to Gainwell Technologies

- Louisiana Enacts Bill Prohibiting Medicaid Plans from Conducting Provider Prepayment Reviews

- Massachusetts Is Granted Temporary Extension of Existing 1115 Medicaid Waiver

- Nebraska is Seeking Not-for-profit Organizations to Provide Housing Stability Services

- North Carolina Legislative Budget Agreement Does Not Contain Provisions for Medicaid Expansion

- Oregon Low-Income, Undocumented Residents To Gain Health Insurance July 1

- Pennsylvania Governor Proposes Fiscal 2023 Nursing Home Rate Increase

- Vermont is Granted 1115 Waiver Extension Through 2027

- Virginia Enacts 30 Percent Increase in Medicaid Dental Reimbursement Rates

- HHS Releases RFI to Strengthen Primary Care System

- CMS to Launch New Risk-Based Payment Model for Medicare Cancer Care

- Evolent Health to Acquire IPG from TPG Growth

In Focus
Early Bird Registration Discount Expires July 11 for HMA Conference on The Future of Publicly Sponsored Healthcare, October 10-11 in Chicago
Be sure to register for HMA’s 2022 Conference by Monday, July 11, to get the special early bird rate of $1,695 per person. After July 11, the rate is $1,895.
Nearly 40 industry speakers, including health plan executives, state Medicaid directors, and providers, are confirmed for HMA’s The New Normal: How Medicaid, Medicare, and Other Publicly Sponsored Programs Are Shaping the Future of Healthcare in a Time of Crisis conference, October 10-11, at the Fairmont Chicago, Millennium Park.
In addition to keynote sessions featuring some of the nation’s top Medicaid and Medicaid executives, attendees can choose from multiple breakout and plenary sessions on behavioral health, dual eligibles, healthcare investing, technology-enabled integrated care, social determinants of health, eligibility redeterminations, staffing, senior care, and more.
There will also be a Pre-Conference Workshop on The Future of Payment Reform: Delivering Value, Managing Risk in Medicare and Medicaid, on Sunday, October 9.
Visit our website for complete details: https://conference.healthmanagement.com/ or contact Carl Mercurio at [email protected]. Group rates and sponsorships are available. The last HMA conference attracted 500 attendees.
State Medicaid Speakers to Date (In alphabetical order)
- Cristen Bates, Interim Medicaid Director, CO Department of Healthcare Policy & Financing
- Jacey Cooper, Medicaid Director, Chief Deputy Director, California Department of Health Care Services
- Kody Kinsley, Secretary, North Carolina Department of Health and Human Services
- Allison Matters Taylor, Medicaid Director, Indiana
- Dave Richard, Deputy Secretary, North Carolina Medicaid
- Debra Sanchez-Torres, Senior Advisor, Centers for Disease Control and Prevention
- Jami Snyder, Director, Arizona Health Care Cost Containment System
- Amanda Van Vleet, Associate Director, Innovation, NC Medicaid Strategy Office, North Carolina Department of Health & Human Services
Medicaid Managed Care Speakers to Date (In alphabetical order)
- John Barger, National VP, Dual Eligible and Medicaid Programs, Humana, Inc.
- Michael Brodsky, MD, Medical Director, Behavioral Health and Social Services, L.A. Care Health Plan
- Aimee Dailey, President, Medicaid, Anthem, Inc.
- Rebecca Engelman, EVP, Medicaid Markets, AmeriHealth Caritas
- Brent Layton, President, COO, Centene Corporation
- Andrew Martin, National Director of Business Development (Housing+Health), UnitedHealth Group
- Kelly Munson, President, Aetna Medicaid
- Thomas Rim, VP, Product Development, AmeriHealth Caritas
- Timothy Spilker, CEO, UnitedHealthcare Community & State
- Courtnay Thompson, Market President, Select Health of SC, an AmeriHealth Caritas Company
- Ghita Worcester, SVP, Public Affairs & Chief Marketing Officer, UCare
- Mary Zavala, Director, Enhanced Care Management, L.A. Care Health Plan
Provider Speakers to Date (In alphabetical order)
- Daniel Elliott, MD, Medical Director, Christiana Care Quality Partners, eBrightHealth ACO, ChristianaCare Health System
- Taylor Nichols, Director of Social Services, Los Angeles Christian Health Centers
- Abby Riddle, President, Florida Complete Care; SVP, Medicare Operations, Independent Living Systems
- David Rogers, President, Independent Living Systems
- Mark Sasvary, Chief Clinical Officer, CBHS, IPA, LLC
- Jim Sinkoff, Deputy Executive Officer, CFO, SunRiver Health
- Tim Skeen, Senior Corporate VP, CIO, Sentara Healthcare
- Efrain Talamantes, SVP & COO, Health Services, AltaMed Health Services Corporation
Featured Speakers to Date (In alphabetical order)
- Drew Altman, President and CEO, Kaiser Family Foundation
- Cindy Cota, Director of Managed Medicaid Growth and Innovation, Volunteers of America
- Jesse Hunter, Operating Partner, Welsh, Carson, Anderson & Stowe
- Bryant Hutson, VP, Business Development, MedArrive
- Martin Lupinetti, President, CEO, HealthShare Exchange (HSX)
- Todd Rogow, President, CEO, Healthix
- Joshua Traylor, Senior Director, Health Care Transformation Task Force
- James Whittenburg, CEO, TenderHeart Health Outcomes
- Shannon Wilson, VP, Population Health & Health Equity, Priority Health; Executive Director, Total Health Care Foundation
HMA Roundup
California
California Extends Medicaid Coverage to Undocumented Residents. Bloomberg Law reported on June 27, 2022, that California Governor Gavin Newsom signed a fiscal 2023 budget that provides $628 million to extend Medi-Cal eligibility to an estimated 698,000 undocumented residents, regardless of age, effective January 1, 2024. The budget also establishes an Office of Health Care Affordability. Read More
Colorado
Colorado Receives Federal Approval to Establish Standardized Exchange Plan Option. Colorado Newsline reported on June 23, 2022, that Colorado has received federal approval for a Section 1332 waiver amendment establishing the Colorado Option, a standardized Exchange plan that insurers will be required to offer to individuals and to employers with less than 100 employees. Insurers must lower premiums on the option by 15 percent over the next three years. Read More
Hawaii
Hawaii to Restore Medicaid Dental Benefits to Adults in 2023. State of Reform reported on June 23, 2022, that Hawaii Med-QUEST will restore Medicaid full dental benefits for adults over age 21 in January 2023, pending federal approval. Dental benefits for adults were removed from Medicaid in 2009. Read More
Indiana
Indiana Awards MMIS Maintenance, Operations Contract to Gainwell Technologies. The Indiana Department of Administration announced on June 15, 2022, its intent to award Gainwell Technologies with the contract for Medicaid Management Information System (MMIS) Maintenance and Operations and Medicaid Business Operations for the Indiana Family and Social Services Administration. Gainwell was the only vendor to submit a proposal. The contract is worth over $2.9 million and will run for five years, including a one-year implementation period, plus two one-year renewal options.
Louisiana
Louisiana Enacts Bill Prohibiting Medicaid Plans from Conducting Provider Prepayment Reviews. The Louisiana State Legislature announced on June 17, 2022, that Governor John Bel Edwards signed Senate Bill 59, which prevents Medicaid managed care organizations from subjecting network providers to prepayment reviews of submitted claims, unless required by the Louisiana Department of Health. The bill is effective August 1, 2022. Read More
Massachusetts
Massachusetts Is Granted Temporary Extension of Existing 1115 Medicaid Waiver. The Massachusetts Executive Office of Health and Human Services announced on June 27, 2022, that federal regulators approved a temporary extension of the state’s existing MassHealth Section 1115 waiver, pending approval of a new five-year agreement submitted late last year. The temporary extension will expire on September 30, 2022. Read More
Nebraska
Nebraska is Seeking Not-for-profit Organizations to Provide Housing Stability Services. The Nebraska Department of Health and Human Services announced on June 29, 2022, it is seeking to award approximately $15 million in federal funds to not-for-profit organizations to provide housing stability services as part of the federal Emergency Rental Assistance program. Awards are expected to be between $100,000 and $2 million, and contracts will run for one year or until August 15, 2023. Read More
North Carolina
Legislative Budget Agreement Does Not Contain Provisions for Medicaid Expansion. North Carolina Public Radio/The Associated Press reported on June 29, 2022, that North Carolina lawmakers in the state House and Senate unveiled a budget agreement for fiscal 2023 that does not include provisions for Medicaid expansion. The Senate passed a Medicaid expansion bill earlier this month, while the House recently proposed its own Medicaid expansion legislation. Read More
House Committee Leaders Introduce Another Medicaid Expansion Bill. FOX8 WGHP reported on June 28, 2022, that the debate over Medicaid expansion in North Carolina will continue, with Republican leadership in the state House Rules Committee introducing a Medicaid expansion bill that would replace one already passed in the Senate. The bill would create a new process for drafting expansion legislation, including working with federal regulators and requiring approval by a Joint Legislative Committee on Medicaid Rate Modernization and Savings in December. In addition to expansion, the plan would invest in substance abuse treatment and mental health, and increase access to health care in rural areas. Read More
North Carolina House Signals That Debate Is Not Over on Medicaid Expansion Proposal. Spectrum News/The Associated Press reported on June 23, 2022, the North Carolina House Health Committee debated a bill (SB 408) directing the state to develop a Medicaid Modernization Plan, including recommendations on how to implement Medicaid expansion. The plan could only be implemented after a formal legislative vote. The state Senate already passed a Medicaid expansion bill (HB 149), which the House is not expected to vote on this session. Read More
Oregon
Oregon Low-Income, Undocumented Residents To Gain Health Insurance July 1. The Oregon Capital Chronicle reported on June 23, 2022, that the Oregon Health Authority will implement a state-funded program offering health insurance to 12,000 low-income, undocumented residents aged 19 to 25 and 55 and up, effective July 1. The program, which is expected to cost $100 million in fiscal 2023, is distinct from Medicaid. Previously, low-income, undocumented individuals in the state received emergency care coverage only. Read More
Pennsylvania
Pennsylvania Health Plan, Hospital System Launch Social Care Network. Highmark Health and Allegheny Health Network announced on June 2, 2022, the launch of a multi-year effort to establish a social care network that will compensate 20 not-for-profit organizations addressing social determinants of health, such as food insecurity and housing for patients referred by the healthcare system. Part of the funding for the program comes from a $5 million grant Highmark received from the Richard King Mellon Foundation. Read More
Governor Proposes Fiscal 2023 Nursing Home Rate Increase. Spotlight PA reported on June 24, 2022, that Pennsylvania Governor Tom Wolf proposed allocating $91.25 million to increase nursing home reimbursement rates to an average of $210 per resident in fiscal 2023. The increase would be aimed at offsetting the cost of a plan to require nursing homes to raise levels of care. Read More
Pennsylvania HealthChoices Plan Selection Period Begins for Beneficiaries. The Pennsylvania Department of Human Services announced on June 22, 2022, the start of the plan selection period for beneficiaries enrolling in Medicaid Physical HealthChoices managed care plans. The selection period runs through August 16, with new HealthChoices contracts to be implemented on September 1. Read More
Rhode Island
Rhode Island to Establish Child Mental Health Task Force. The Providence Journal reported on June 25, 2022, that the Rhode Island legislature passed legislation to form a task force aimed at improving the delivery of mental health care services covered by Medicaid for children under the age of six. Less than eight percent of covered children received mental health services in 2018. Read More
Vermont
Vermont is Granted 1115 Waiver Extension Through 2027. Healthcare Innovation reported on June 28, 2022, that the Vermont Agency of Human Services received federal approval to extend the state’s Global Commitment to Health Section 1115 Medicaid waiver through 2027. The approval allows the state to continue existing programs and implement new initiatives for housing assistance, health information technology, maternal health, and substance use disorder. Read More
Virginia
Virginia Enacts 30 Percent Increase in Medicaid Dental Reimbursement Rates. CBS 19 News reported on June 22, 2022, that Virginia Governor Glenn Youngkin signed a 2022-24 budget that includes a 30 percent increase in Medicaid reimbursement rates for dental services. The increase goes into effect on July 1. Read More
Washington
Washington Releases Rebased Medicaid Hospital Payment Rates. The Washington Health Care Authority (HCA) released on June 22, 2022, updated Medicaid inpatient and outpatient hospital payment rates, effective July 1, 2022. HCA rebased prospective payment methodologies to better reflect cost differences for providing services. Read More
West Virginia
West Virginia Seeks 10 Percent Increase in Medicaid Ambulance Service Reimbursement Rate. West Virginia Public Broadcasting reported on June 22, 2022, that the West Virginia Department of Health and Human Resources is seeking a 10 percent reimbursement rate increase for ambulance service providers in response to rising fuel costs. The proposed rate increase would go into effect on July 1. Read More
National
HHS Releases RFI to Strengthen Primary Care System. Fierce Healthcare reported on June 28, 2022, that the U.S. Department of Health and Human Services (HHS) issued a request for information (RFI) on how to establish a federal infrastructure for improving primary care in the U.S., with an initial goal of releasing an action plan by the end of the year. HHS is seeking comments on primary care payments, delivery models, service integration, access, workforce education, training, digital health, care measurement, research, and barriers to implementing innovations. Responses are due on August 1. Read More
Information Gaps Remain in Federal Oversight of Medicaid Directed Payments, GAO Study Says. The U.S. Government Accountability Office (GAO) released a study on June 28, 2022, which found that information gaps remain in federal efforts to oversee of Medicaid directed payments by states, raising concerns over the potential for inappropriate payments. The study also noted that the effectiveness of recent efforts by the Centers for Medicare & Medicaid Services to enhance oversight of directed payments remains unknown. Thirty-six states received CMS approval for one or more directed payment initiative in 2021. Read More
Removing Prior Authorizations for OUD Treatments Has Mixed Effect on Medicaid Beneficiary Access to Care, Study Finds. Health Payer Intelligence reported on June 27, 2022, that removing prior authorizations for opioid use disorder (OUD) treatments like buprenorphine had a mixed effect on Medicaid beneficiary access to care, according to a JAMA Health Study. The study found that removing prior authorizations on buprenorphine led to a statistically significant decrease in buprenorphine prescriptions in California and a statistically significant increase in Illinois. The study used Medicaid State Drug Utilization Data for California and Illinois from 2013 to 2020 and compared it to eight control states. Read More
MACPAC Comments on Medicare Proposed Rule Impacting Immunosuppressive Drug Benefit, Enrollment. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on June 27, 2022, support for the Centers for Medicare & Medicaid Services (CMS) proposed rule to extend the Medicare Savings Program coverage for individuals enrolled in the Medicare Part B immunosuppressive drug benefit, according to comments submitted to the agency. MACPAC also outlined support for CMS’ efforts to create streamlined eligibility and enrollment processes across Medicare and Medicaid, including a new Medicare special enrollment period for individuals who lose Medicaid eligibility after the public health emergency ends. Read More
CMS Urges Congress to Pass Legislation Extending Enhanced Exchange Subsidies. Fierce Healthcare reported on June 22, 2022, that the Centers for Medicare & Medicaid Services (CMS) is urging Congress to pass legislation extending enhanced Affordable Care Act (ACA) subsidies beyond 2022. Open enrollment for 2023 begins in November, and health plans are already developing 2023 rates. The enhanced subsidies led to a record 14.5 million individuals enrolling in Exchange plans for 2022. The Build Back Better Act would have extended the subsidies through 2025, but it stalled in the Senate. Read More
HUD Announces Grants, Voucher Funding to Address Homelessness. The Centers for Medicare & Medicaid Services announced on June 22, 2022, the availability of $365 million in grants and voucher funding to address unsheltered homelessness and homeless encampments. The funding, which is available through the U.S. Department of Housing and Urban Development (HUD), includes $54.5 million for permanent housing in rural communities and $43 million for roughly 4,000 incremental housing choice vouchers for vulnerable families. Read More
CMS Considers Mandating NCQA Health Equity Accreditation for Medicaid, Exchange Plans. Modern Healthcare reported on June 21, 2022, that the Centers for Medicare & Medicaid Services (CMS) is considering making National Committee for Quality Assurance’s (NCQA) Health Equity Accreditation mandatory for Medicaid and Exchange plans in an effort to address health disparities. The change would require that Medicaid and Exchange plans comply with new standards aimed at addressing disparities. NCQA launched the Health Equity Accreditation program in November 2021. Read More
Dual Eligibles Utilize Home Health Care at Twice the Rate of Medicare-Only Beneficiaries. Home Health Care News reported on June 27, 2022, that Medicaid and Medicare dual eligibiles utilize home health care at twice the rate of individuals who are only covered by Medicare, according to a report from ATI Advisory, with support from Arnold Ventures. The report also found that dual eligibles prefer Medicare Advantage plans, which offer supplemental benefits, more than Medicare-only beneficiaries. About 12 million of the 63.1 million Medicare beneficiaries are dually eligible. Read More
CMS to Launch New Risk-Based Payment Model for Medicare Cancer Care. Modern Healthcare reported on June 27, 2022, that the Centers for Medicare & Medicaid Services (CMS) announced the Enhancing Oncology Model, a new risk-based Medicare payment model aimed at improving cancer care. Under the new model, which will be effective July 1, 2023, and run for five years, providers will have upside and downside risk for patient quality and expenditures over a six-month episode of care. Providers can bill an additional monthly capitated rate of $70 for extra services and receive $30 per member per month extra for dual eligibles. The new model builds off of the Oncology Care Model, which will end on June 30 after six years. Read More
U.S. Supreme Court Upholds 2005 Federal DSH Payment Rule. Modern Healthcare reported on June 24, 2022, that the U.S. Department of Health and Human Services (HHS) acted appropriately when it changed the formula for how Medicare Disproportionate Share Hospital (DSH) payments are calculated in a 2005 rule, according to the U.S. Supreme Court. The rule includes patient days of individuals enrolled in Medicare Part A regardless of whether services were provided. Hospitals were expecting to receive additional funds if they won the case. The high court ruling reverses a decision by the U.S. Court of Appeals. Read More
CMS Proposes 4.2 Percent Decrease in Fiscal 2023 Medicare Home Health Provider Payments. Home Health Care News reported on June 23, 2022, that the Centers for Medicare & Medicaid Services (CMS) proposed a 4.2 percent decrease in aggregate fiscal 2023 Medicare home health provider payments. Under the proposal, home health providers would receive $801 million less compared to fiscal 2022. Read More
Industry News
Evolent Health to Acquire IPG from TPG Growth. Evolent Health announced on June 29, 2022, a definitive agreement to acquire musculoskeletal surgery cost management company IPG from TPG Growth for $375 million, plus up to $87 million in performance incentives. IPG will become part of Evolent’s New Century Health operation. Read More
South Shore Peer Recovery Announces Formal Affiliation With Aspire Health Alliance. South Shore Peer Recovery (SSPR) announced on June 27, 2022, a formal affiliation with Aspire Health Alliance, a community-based mental health center in Boston. SSPR provides services for individuals in recovery from substance use disorder. Read More
Pinnacle Treatment Centers Acquires Stepping Stone of North Carolina. Pinnacle Treatment Centers announced on June 22, 2022, the acquisition of Stepping Stone of North Carolina, an outpatient opioid addiction treatment program offering medication-assisted treatment. Pinnacle, a provider of community-based drug and alcohol addiction treatment, now operates in nine states. Read More
Sonrava Health Completes Acquisition of Mid-Atlantic Dental Partners. Sonrava Health announced on June 22, 2022, that it has completed the acquisition of Mid-Atlantic Dental Partners. Sonrava Health now has 215 offices in 17 states. Read More
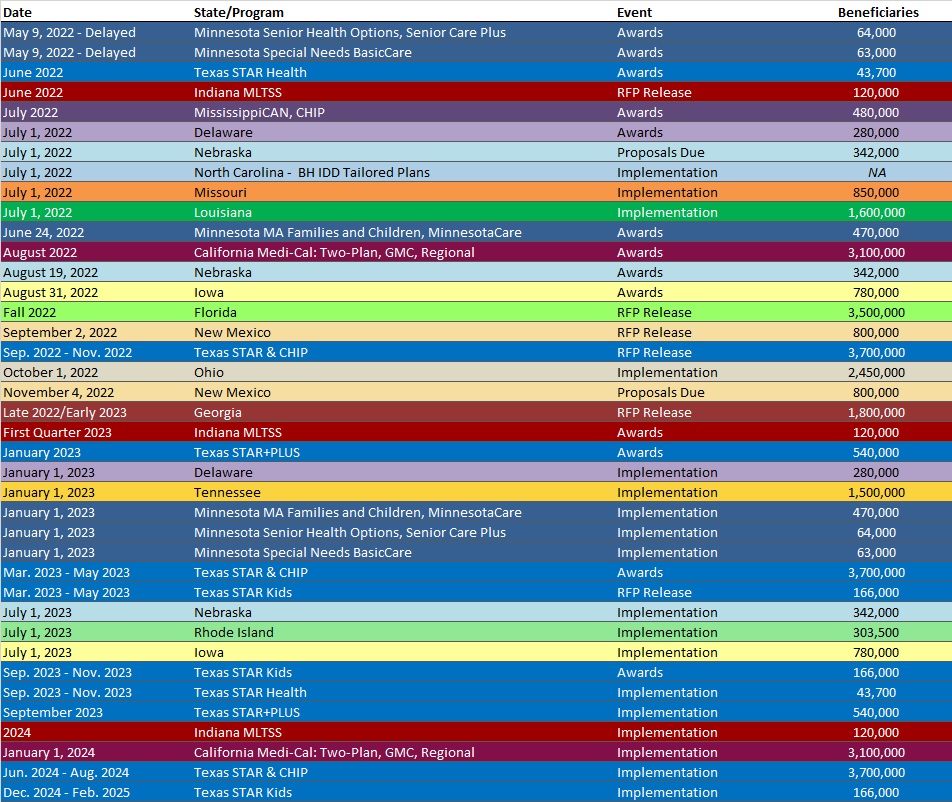
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
- Colorado RAE Enrollment is Up 2.2%, Mar-22 Data
- Delaware SNP Membership at 12,219, Mar-22 Data
- Hawaii SNP Membership at 29,520, Mar-22 Data
- Kansas Medicaid Managed Care Enrollment is Up 10.8%, 2021 Data
- Kansas Medicaid Managed Care Enrollment is Up 1.8%, Mar-22 Data
- Michigan Dual Demo Enrollment is Down 5.7%, Feb-22 Data
- Michigan Medicaid Managed Care Enrollment is Flat, Feb-22 Data
- Nevada Medicaid Managed Care Enrollment is Up 12.6%, 2021 Data
- Nevada Medicaid Managed Care Enrollment is Up 2.5%, Apr-22 Data
- New Mexico Medicaid Managed Care Enrollment is Up 6.5%, 2021 Data
- North Carolina Medicaid Managed Care Enrollment is 1.7 Million, 2021 Data
- North Dakota Medicaid Expansion Enrollment is Up 27%, 2021 Data
- South Carolina Dual Demo Enrollment is Down 5.2%, 2021 Data
- South Carolina Medicaid Managed Care Enrollment is Up 10.1%, 2021 Data
- Wisconsin SNP Membership at 71,718, Mar-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Indiana MMIS M&O and Medicaid Business Operations RFP, Proposal, Award, and Related Documents, 2022
- Michigan Medicaid Actuarial Services RFP, Jun-22
- New Hampshire Medicaid Managed Care Contracts and Amendments, 2019-22
- Tennessee Pharmacy Reimbursement Services RFP, Jun-22
Medicaid Program Reports, Data and Updates:
- New Hampshire Medicaid Enrollment Demographic Trends and Geography, May-22
- North Carolina Medicaid Annual Reports, SFY 2015-21
- North Dakota Medicaid Expansion Quality Strategy Plans, 2018-22
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, June-22
- Rhode Island 2020 EQR Annual Technical Reports, Apr-22
- Rhode Island Long Term Care Service and Finance Performance Report, Apr-22
- Rhode Island Medicaid Expenditure Report SFY 2020, Apr-22
- Vermont ACO Quality Measures, 2018-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
