HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: State Teams Convene to Strengthen Collaboration across Child Welfare, Behavioral Health, and Medicaid

- HMA Offers a New Way to Approach Grant Funding for Behavioral Health Providers

- California Names Tyler Sadwith Medicaid Director

- Colorado Plans to Submit 1115 Waiver Expanding SMI Inpatient Mental Health Services

- Georgia Senate Advances Bill to Relax Certificate-of-need Regulations, Form Health Commission

- Georgia Medicaid Work Requirements Program Faces Low Enrollment, Higher than Projected Admin Costs

- Kansas House, Senate Committees to Hold Hearings on Medicaid Expansion

- Kentucky Supreme Court Rules Medicaid Managed Care Contracts to Remain in Place

- Mississippi Senate Medicaid Expansion Bill Dies; Focus Shifts to House Bill

- New York Releases Self-directed Care Initiative RFI

- Ohio to Release RFA for FIDE SNPs in Coming Months

- HHS Announces New Model to Improve Primary Care Access for Medicare Beneficiaries

- U.S. Senators Introduce Bill to Streamline Care Coordination for Dual Eligibles

- CMS to Hasten Medicaid Reimbursements for Providers Affected by Cyberattack

- States Consider Medicaid Rate Hikes in Fiscal 2025

- MedPAC and MACPAC Release Respective March 2024 Reports to Congress

- Medicare Billed $101.4 Million for Remote Monitoring Services in 2021, KFF Finds

- Elevance to Acquire Kroger’s Specialty Pharmacy Business

- UnitedHealth Group Pays $2 Billion to Providers Affected by Cyberattack

In Focus
State Teams Convene to Strengthen Collaboration across Child Welfare, Behavioral Health, and Medicaid
This week, our In Focus section highlights the Children’s Behavioral Health (CBH) State Policy Lab, held February 7−9, in Baltimore, MD. Health Management Associates, Inc., (HMA), in partnership with national philanthropies and associations, hosted the Policy Lab, which provided an unprecedented opportunity for state cross-systems teams to conduct in-depth work toward creating an equitable behavioral health system of care for children and youth.
Background
The lack of collaboration and misaligned strategies and policies across state child welfare, behavioral health, and Medicaid has contributed to unsatisfactory outcomes for children and youth in our communities. The COVID-19 public health emergency exacerbated these issues, as the rate of mental health and substance use disorders (SUD) increased and many families experienced traumatic events during this time. Increasingly, states and local jurisdictions are exposed to threats or actual class action lawsuits based on the inadequate care of children and youth involved in the child welfare settings.
Fortunately, federal and state efforts and investments to address the youth systems of care—including schools, community, delivery systems, and community-based child placing agencies—are in motion. Though the diversity of efforts being implemented across local and state agencies are critical, these complex issues require collaboration across multiple systems, including Child Welfare, Behavioral Health authorities, Medicaid, and K-12 Education. A cross-sector strategic approach will enable comprehensive identification of gaps, policy solutions, and best practices, as well as highlight opportunities for cross-sector braided or blended funding to build a system of care that supports the needs of multi-system children, youth, and their families.
Child Behavioral Policy Lab
The current behavioral health crisis presents an opportunity to address long-term challenges and divisions and to build a truly comprehensive approach. This is why HMA sponsored the Children’s Behavioral Health State Policy Lab which convened key partners within a state and across states. The Annie E. Casey Foundation, Casey Family Programs, National Association of State Mental Health Program Directors (NASMHPD), the Child Welfare League of America (CWLA), the American Public Human Services Association (APHSA), National Association of Medicaid Directors (NAMD) and MITRE, a Children’s Behavioral Health (CBH) State Policy Lab, joined HMA in funding, organizing and providing consultation support for the meeting.
The nine participating states—Georgia, Kansas, Kentucky, Maryland, Missouri, Pennsylvania, Texas, Utah, and Wisconsin—were selected through a competitive process based on the goals and commitment of the state and the thorough analysis of gaps and opportunities, demonstration of collaborative state interagency partnerships, and engagement of youth and adults.
The participating states committed their leadership teams to join the Policy Lab in laying the foundational work of development of statewide plans that would advance their collective goal of creating a more united system of care. Participants learned about intergenerational trauma and resilience. The sessions also provided participants with data that helped provide context to the problems we are trying to solve. Presenters included Aliyah Zeien, a national child welfare policy advocate and youth ambassador, with lived experience who highlighted that 25 percent of foster youth will spend time in prison or other enforcement systems within two years of leaving the child welfare system. Her experience and reflections served as call for action to actively engage families and youth in all system planning, advocacy, and policy work.
Key areas of focus
Following these brief educational sessions, each state had substantial “team time” to develop a road map and set of next steps for continuing their work after the Policy Lab. Expert facilitators guided state teams through discussions on three key issues:
- Service array. State teams were challenged to define their array of services and develop collective agreements on how to develop enhanced treatment options for children and their families. With an emphasis on building a full continuum of care with community-based supports and fewer children in residential facilities, each team considered challenges such as eligibility, access, and workforce. Prevention, diversion, and engagement of people with lived experience to help with system development were common commitments in state action teams.
- Financing. The teams considered their statutory authority, funding streams, funding partners, contract vehicles, and financing mechanisms. They also worked on ideas for blending and braiding funding, with a focus on Medicaid and leveraging collective opportunities to develop staff and contractual resources.
- Governance. State teams worked through difficult conversations, including how to measure success, how to manage accountability and monitoring, how to collaboratively design services and case practice, while meaningfully sharing data and creating interoperability within their systems while respecting confidentiality and privacy concerns.
What’s Next
Since the Policy Lab program, most participating states have embarked on next steps identified during the workshop, such as vetting their plans with state leadership, creating an ongoing team for implementation, and identifying community partners. HMA and HMA Companies, including Leavitt Partners, are collaborating with our Policy Lab partners and the state agencies to further develop these plans and prepare for implementations that rethink our approach to services for youth and their families.
For more information about the Policy Lab and follow-on work, please contact Uma Ahluwalia ([email protected]), Christina Altmayer ([email protected]), Jon Rubin ([email protected]), and Sarah Scholle ([email protected]).
HMA Offers a New Way to Approach Grant Funding for Behavioral Health Providers
Grants from both government and foundations can be an essential component of a community behavioral health provider’s growth strategy. Every year billions of dollars are distributed to support program growth, quality improvement, training, and other essential needs. Finding the right opportunities and applying for grants that are aligned with your organization’s strategic growth interests can be an essential catalyst for organizational development, service continuum growth, and quality improvements.
Behavioral health providers often struggle with identifying and applying for the right grant opportunities. It is time consuming and takes resources away from your mission to serve your communities. The deluge of notices of funding opportunities, requests for proposals, requests for applications, and requests for expressions of interest can overwhelm even the most sophisticated and well-resourced provider. Few organizations have the internal capacity to devote to wading through the hundreds of opportunities that are published each week.
That is why we created HMA Grant Prospector. HMA will do the work, so you don’t have to.
The HMA Grant Prospector is a tool that combines HMA’s deep subject matter expertise in community behavioral health care with understanding of the process of grant procurement. We have embedded this expertise in proprietary software that can sift through grant opportunities and pick out the gold nuggets from the mountain of information.
When your organization subscribes to Grant Prospector, we interview you to find out what services you have, the communities you serve, and what gaps in your care continuum you seek funding to fill. We collect information on grant opportunities as they are released, and the Grant Prospector matches your organization’s criteria with funding opportunities. We’ll send you only those opportunities for which your organization is eligible, that are aligned with your strategy and organizational objectives, and targeted to your population. You can rely on HMA to do the legwork so you can focus your efforts on improving lives in your community.
HMA Roundup
Arizona
Arizona House Considers Bill to Reduce Medicaid Fraud Targeting Rehabilitation Facilities. ABC News reported on March 15, 2024, that the Arizona House Health and Human Services Committee is considering a Senate-passed bill, sponsored by Senator Theresa Hatathlie (D-Coal Mine Canyon), that would strengthen regulations for rehab facilities in response to fraudulent Medicaid billing and scams targeting Native Americans receiving care in the facilities. Specifically, the bill would increase the civil penalty per incidence of noncompliance at facilities from up to $500 to at least $1,500 daily, require patients’ family members to be notified when they arrive at a facility, and ensure that employees undergo fingerprint and background checks. Governor Katie Hobbs and Attorney General Kris Mayes previously indicated plans to investigate fraudulent Medicaid charges, most of which had been submitted through the American Indian Health Program, a health plan, and have resulted in 72 indictments thus far.
Arizona Medicaid Provider Fraud Extends into Managed Care Organizations, Senate Passes Bill Increasing Provider Oversight. The Arizona Daily Star reported on March 15, 2024, that the Arizona Health Care Cost Containment System acknowledged fraud in the Medicaid managed care program, not just in traditional fee-for-service, within Medicaid behavioral health residential and outpatient treatment service providers. Fraud has cost the state $2 billion and harmed more than 7,000 individuals. Separately, the state Senate has advanced a bill that strengthens oversight and regulations required by behavioral health entities and sober living homes and increases penalties for violations. Read More
California
California Names Tyler Sadwith Medicaid Director. Becker’s Payer Issues reported on March 14, 2024, that Tyler Sadwith has been named Medicaid director of the California Department of Health Care Services (DHCS). Sadwith was previously deputy director of behavioral health at DHCS. Read More
Colorado
Colorado Plans to Submit 1115 Waiver Expanding SMI Inpatient Mental Health Services. The Colorado Sun reported on March 18, 2024, that legislators are requesting $7.2 million be allocated to the Colorado Medicaid department to reimburse psychiatric hospitals, crisis stabilization units, and other centers that care for people with serious mental illness (SMI) who need care for up to 30 days, as recommended by the Joint Budget Committee. The state plans to submit by April 1 a Section 1115 demonstration proposal for federal approval to implement the new policy. Read More
Colorado Launches Medicaid eConsult Platform. Safety Net Connect announced on March 19, 2024, that the Colorado Department of Health Care Policy & Financing has launched the Colorado Medicaid eConsult platform, aimed at facilitating electronic communication between Medicaid primary care providers and specialists. Primary care providers gained access to the platform effective February 1. Read More
Delaware
Delaware Senator Proposes Bill to Implement Provider Tax to Support Medicaid. Delaware Public Media reported on March 18, 2024, that Delaware Senator Sarah McBride (D-Bellefonte) has introduced legislation that would require hospitals and behavioral facilities to pay a 3.58 percent provider tax. The new hospital tax would generate federal matching funds used to support investments in Medicaid including increasing reimbursement rates for providers, expanding coverage, or building out innovative policies. The bill has been assigned to the Senate Health and Social Services Committee. Delaware is only one of six states that does not have a health care facility assessment for its hospitals. Read More
Georgia
Georgia Medicaid Work Requirements Program Faces Criticism of Low Enrollment, High Admin. Costs. KFF Health News reported on March 20, 2024, that Georgia’s Pathways to Coverage program, which offers Medicaid to people earning up to the federal poverty level if they meet defined work requirements, has cost a minimum of $26 million thus far, with additional costs expected when the state begins collecting premiums and verifying compliance with work requirements. Although the state projected that more than 25,000 individuals would enroll in the first year and 52,000 after five years, about 3,500 individuals have enrolled since the program began in July. Approximately 45 percent of applications for the Pathways programs are currently waiting to be processed. Read More
Georgia Senate Advances Bill to Relax Certificate-of-need Regulations, Form Health Commission. The Georgia Recorder reported on March 15, 2024, that the Georgia Senate has advanced a bill that would scale back certificate-of-need regulations, form a comprehensive health coverage commission, and make it easier to open psychiatric and substance abuse inpatient facilities and rural hospitals. Senate Democrats are expected to withhold support for the legislation next time unless the bill includes full Medicaid expansion. The bill will now go back to the House for further consideration. Read More
Idaho
Idaho Proposed Fiscal 2025 Medicaid Budget Includes Funding for Provider Rate Increases. The Idaho Capital Sun reported on March 18, 2024, that the Idaho Joint Finance-Appropriations Committee has drafted the state’s fiscal 2025 Medicaid budget and included spending requests that are intended to increase funding for new staff and pay for current medical providers. Approved requests included approximately $66 million in provider rate increases, $58 million in non-discretionary adjustments, and $362,000 for regular employee pay raises. The budget totals $4.7 billion, which is about $27.7 million more than last year’s budget. Read More
Indiana
Indiana Hospitals Experience Delayed Payments, Financial Losses Following Cyberattack at Change Healthcare. WFYI Indianapolis reported on March 18, 2024, that the cyberattack on Change Healthcare continues to impact hospitals in Indiana, according to a recent survey from the Indiana Hospital Association (IHA). One-third of IHA’s members responded to the survey, with 60 percent of them reporting that the cyberattack has had a direct impact on patient care and nearly all have had financial losses. IHA indicated that there could be a delay in processing of about $50 to $60 million in payments. According to the IHA survey, most hospitals had identified temporary solutions for processing payments. Read More
Iowa
Iowa Medicaid Fraud Control Units Receive Less Funding, Possess Fewer Staff, Survey Finds. Iowa Capital Dispatch reported on March 19, 2024, that Iowa’s Medicaid Fraud Control Unit (MFCU), responsible for investigating abuse and neglect of Medicaid beneficiaries as well as provider fraud, received less funding and possessed fewer staff than other states in 2022, according to a recent survey conducted by the National Association of Medicaid Fraud Control Units. For example, Indiana Medicaid spent less than half of what Iowa’s program spent in 2022, yet Indiana allocated $8.4 million for its MFCU while Iowa allocated $1.3 million. There were four other states in the country that had fewer total staff members than Iowa. In 2022, the Office of Inspector General previously noted the Iowa MFCU’s low staffing levels and stated that hiring additional staff would enhance the program’s operations, though the state disagreed with the assessment. Read More
Kansas
Kansas House, Senate Committees to Hold Hearings on Medicaid Expansion. The Topeka Capital-Journal reported on March 13, 2024, that the Kansas House and Senate will both hold hearings on Medicaid expansion for the first time since 2020. The Senate Public Health and Welfare Committee is scheduled to have a joint meeting with the Senate Ways and Means Committee on March 20. The House Health and Human Services Committee will hold a hearing regarding expansion House Bill 2556 on the same day. Read More
Kentucky
Kentucky Supreme Court Rules Medicaid Managed Care Contracts to Remain in Place. Kentucky Lantern reported on March 14, 2024, that the Kentucky state Supreme Court will uphold a 2022 state Court of Appeals ruling that Elevance Health was rightfully excluded from receiving a contract in the state’s 2020 Medicaid managed care procurement. The successful bidders, CVS/Aetna, Humana, Molina, UnitedHealthcare, and Centene/WellCare will retain their contracts. Read More
Maine
Maine Incumbents Appeal NEMT Contract Awarded to Modivcare. The Bangor Daily News reported on March 18, 2024, that current incumbents Penquis Community Action Agency and Waldo Community Action Partners (CAP) are appealing Maine’s decision to award Modivcare Solutions a statewide contract for non-emergency medical transportation (NEMT) services, citing unfair scoring of proposals. Penquis bid to cover four regions of the state, and Waldo CAP bid for one. Modivcare’s anticipated contract, estimated to be worth $750 million, will run for an initial two-years beginning July 1, with renewals for up to 10 years. Read More
Mississippi
Mississippi Senate Medicaid Expansion Bill Dies; Focus Shifts to House Bill. WAPT reported on March 14, 2024, that the Mississippi Senate has allowed its Medicaid expansion bill to die. The Senate now plans to amend the House bill version and include work requirements. Read More
Nebraska
Nebraska Legislators Consider Provider Tax Bill to Increase Medicaid Funding for Nursing Homes. The Grand Island Independent reported on March 18, 2024, that Nebraska legislators are considering an amendment to a bill, sponsored by Senator Myron Dorn (R-Adams), that would increase payment rates for nursing homes serving Medicaid beneficiaries. The measure would boost nursing home provider taxes from $3.50 per day per resident to $9 per day per resident, which would yield approximately $23 million in additional Medicaid funding. The bill requires further review before it heads to the floor of the legislature. Lawmakers are also considering a new provider tax applied to hospitals. Read More
Nevada
Nevada Judge Blocks State from Limiting Medicaid Coverage for Abortions. ABC News reported on March 19, 2024, that Nevada District Judge Erika Ballou struck down the state’s limitations on Medicaid coverage for abortion services on the basis that the restrictions violate equal rights protections. Judge Ballou also indicated plans to issue an order directing the state to grant Medicaid coverage for all abortions, though she noted that the actions may be appealed. Nevada currently only provides Medicaid coverage for abortions in the case of a life-threatening pregnancy, rape, or incest.
New York
New York Senate, Assembly Fiscal 2025 Budget Proposes 3 Percent Medicaid Rate Increases. Politico Pro reported on March 14, 2024, that the New York Senate and Assembly have each proposed three percent Medicaid rate increases in their respective budget bills for fiscal 2025. Additionally, the Assembly called for a supplementary 7.5 percent increase for hospitals, nursing homes, and assisted living facilities, while the Senate proposed a seven percent increase for hospitals and a 6.5 percent increase for nursing homes, assisted living facilities, and hospice services. The proposals challenged Governor Kathy Hochul’s proposed budget, which called for a reduction in Medicaid spending to reduce the program’s rising costs. Read More
New York Releases Self-directed Care Initiative RFI. The New York State Office of Mental Health released on March 13, 2024, a request for information (RFI) seeking interest from vendors to operate a Self-directed Care program providing support broker and fiscal intermediary services to Health and Recovery Plan (HARP) enrollees and HARP-eligible HIV Special Needs Plan enrollees. Interested vendors would be required to recruit HARP members to participate in a pilot program, hire and train support brokers, support program participants in reaching their recovery goals, designate a fiscal intermediary to manage funds, and provide self-directed care to a minimum of 100 individuals in the specified geographic region. Responses are due April 3, 2024.
Ohio
Ohio to Release RFA for FIDE SNPs in Coming Months. The Ohio Department of Medicaid announced on March 5, 2024, that it will release a request for applications for MyCare Ohio, the state’s managed care program serving individuals dually eligible for Medicaid and Medicare, in the coming months. The state will transition to a Fully Integrated Dual-Eligible Special Needs Plan (FIDE SNP) model from the Financial Alignment Initiative dual demonstration that is being sunset by the Centers for Medicare & Medicaid Services (CMS). Contract awardees will be required to notify CMS of intent to establish a FIDE SNP in Ohio by Fall 2024. Selected FIDE SNPs will begin to serve eligible individuals in the 29 demonstration counties beginning January 2026.
Pennsylvania
Pennsylvania Improperly Claimed $551 Million in Medicaid Funds, OIG Audit Finds. Scripps News reported on March 13, 2024, that Pennsylvania improperly received $551 million in Medicaid funds to go toward its school-based services, according to an audit from the U.S. Office of the Inspector General (OIG). The report found improper claims totaling $182.5 million from July 2015 through June 2019. The state additionally claimed $368.9 million via unsupported ratios when allocating costs to Medicaid. OIG recommended that Pennsylvania refund $182.5 million and provide evidence justifying the $368.9 million, though the state maintains that it is not required to release supporting documentation. Read More
Virginia
Virginia Budget Amendment to Contract with Single PBM Dies. The Virginia Mercury reported on March 14, 2024, that a pair of Virginia budget amendments, introduced by Delegate Mark Sickles (D-Fairfax) and Senator Travis Hackworth (R-Tazwell), that would have required the Virginia Department of Medical Assistance Services to contract with a single prescription benefits manager (PBM) died in conference. Some pharmacists estimated that the proposed transition to a single PBM would have saved more than $30 million in the state budget and improved drug transparency and affordability. Governor Glenn Youngkin may determine whether to include the amendments in the state budget when the General Assembly reconvenes on April 17. Read More
National
PBM Legislation Dropped from Upcoming Spending Bill Package. Modern Healthcare reported on March 19, 2024, that a healthcare package that included legislation pushing for stronger regulations on pharmacy benefit managers (PBMs) and enhanced community health center funding will not be included in the second set of fiscal 2024 spending bills that must reach President Biden by March 22 to avoid a government shutdown. Lawmakers could not reach agreement on whether new regulations on PBMs should apply only to Medicare and Medicaid or be expanded to the private insurance market. The policies generally have broad bipartisan support, and lawmakers may decide to revisit the issues during the lame duck Congress after the November election. Read More
HHS Announces New Model to Improve Primary Care Access for Medicare Beneficiaries. The U.S. Department of Health and Human Services (HHS) announced on March 19, 2024, a new voluntary model, titled the Accountable Care Organization Primary Care Flex Model (ACO PC Flex Model), which will provide a one-time advanced shared savings payment and monthly prospective primary care payments to ACOs to encourage person-centered primary care and to promote competition in healthcare. The Centers for Medicare & Medicaid Services (CMS) Innovation Center will test the model within the Medicare Shared Savings Program and invest in low revenue ACOs to strengthen care access and quality for their respective Medicare beneficiaries. CMS expects to select approximately 130 ACOs to participate in the model, which will last for five years beginning on January 1, 2025. Interested applicants must first apply to the Shared Savings Program between May 20 and June 17. A Request for Applications is anticipated to be released in the second quarter of 2024. Read More
Senators Introduce Bill to Streamline Care Coordination for Dual Eligibles. The Office of Senator Bill Cassidy (R-Louisiana) announced on March 14, 2024, that Cassidy and other members of the Senate Duals Working Group introduced a bill, titled “Delivering Unified Access to Lifesaving Services (DUALS) Act of 2024,” which would require states to develop integrated health plans for individuals dually eligible for Medicare and Medicaid. The bill aims to further streamline care for dual eligibles by reducing plans that do not provide care coordination and expanding the Program of All-Inclusive Care for the Elderly. Read More
President Biden Signs Executive Order Expanding Women’s Health Initiatives. The New York Times reported on March 18, 2024, that President Joe Biden signed an executive order aimed at strengthening research and data standards on women’s health and directed federal agencies to use federal funds to research health conditions and diseases that disproportionately affect women. Health conditions like heart disease, Alzheimer’s, menopause, and fibroids would be a focus of the expanded research effort. Under the executive order, agencies will be will required to annually report their investments in women’s health research and to study ways that artificial intelligence can be used to advance such research. Read More
CMS to Hasten Medicaid Reimbursements for Providers Affected by Cyberattack. Modern Healthcare reported on March 15, 2024, that the Centers for Medicare & Medicaid Services (CMS) will allow states to submit Medicaid state plan amendments in order to make interim payments to providers affected by disabled payment systems due the cyberattack on Change Healthcare. States will be able to use Federal Financial Participation funds and the payments can be retroactive to February 21. States are encouraged to submit required documentation by March 31. Read More
States Consider Medicaid Rate Hikes in Fiscal 2025. Modern Healthcare reported on March 15, 2024, that some states are planning to increase Medicaid managed care capitation rates for fiscal 2025 while others plan to reduce payments and benefits such as long-term services and supports, in-home care, and mobile crisis units. Arizona, California, Missouri, and Washington are among the states that aim to raise capitation rates. New York aims to eliminate a quality bonus program and a one percent pay increase to cut costs. Legislators in Indiana, Kentucky, and other states have proposed reducing benefits. Read More
MedPAC Releases March 2024 Report to Congress. The Medicare Payment Advisory Commission (MedPAC) released on March 15, 2024, its annual report to Congress recommending lower payments for hospice providers and post-acute care sectors, including skilled nursing facilities, home health, and inpatient rehabilitation facilities for 2025. MedPAC found that the government will spend an estimated $83 billion more on the cost of care for enrollees in Medicare Advantage plans this year than if the same beneficiaries were enrolled in the traditional fee-for-service program. Read More
CMS Releases Guidance on Medicaid Health Home Core Sets. The Centers for Medicare & Medicaid Services (CMS) released on March 15, 2024, a state health official letter which details the state requirements that begin in federal fiscal year 2024 for Core Sets of Health Home Quality Measures for Medicaid (Health Home Core Sets). The letter also provides updates to the 2025 Health Home Core Sets. Revisions include the ambulatory care emergency department visits measure and retires the chronic conditions composite measure. Read More
CMS Releases Guidelines Regarding Permissible Practices During Medicaid, CHIP Eligibility Renewals. The Centers for Medicare & Medicaid Services (CMS) released on March 15, 2024, an informational bulletin and slide deck to clarify the permissibility of certain practices during Medicaid and the Children’s Health Insurance Program (CHIP) renewals. Specifically, the bulletin reiterates the circumstances in which states are not allowed to terminate beneficiaries, exclude individuals from ex parte renewal, or transition individuals to the Marketplace or a different eligibility category. The information is intended to address questions that CMS has received from states, stakeholders, and external partners. Read More
Several Providers Cease Participation in Medicare ACO REACH in 2024. Modern Healthcare reported on March 19, 2024, that 10 accountable care organization (ACOs) have left the Centers for Medicare & Medicaid Services (CMS) ACO Realizing Equity, Access, and Community Health (ACO REACH) program, with Alignment Health, Centene, and NeueHealth scaling back participation. CMS has reported a year-over-year decline in the total number of ACOs in program in 2024, although the number of providers and traditional Medicare enrollees in ACO REACH grew by 30 percent. CMS plans to get all fee-for-service Medicare enrollees under an ACO by 2030. Read More
Medicaid Managed Care Appeals Rates Varied Among States in 2022, GAO Finds. The U.S. Government Accountability Office (GAO) released on March 14, 2024, a report that found that rates of Medicaid managed care appeals and grievances varied widely across states in 2022, with appeals rates ranging from 1.4 to 79.9 appeals per 1,000 enrollees in the 27 states examined. The report attributed variance to differences in states’ appeals processes, including communication about the appeals process, the supports available for enrollees to navigate the process, and whether a state offers external medical review as part of the process. Approximately 20.9 percent of appeals taken to the state for a fair hearing resulted in a favorable outcome for the enrollee, 25 percent of cases were retracted, and 53.7 percent of cases resulted in a decision adverse for the enrollee. GAO recommended that the Centers for Medicare & Medicaid Services require states to report on the outcomes of Medicaid managed care appeals and the number of denials and implement strategies to improve oversight and transparency. Read More
MACPAC Releases March 2024 Report to Congress. The Medicaid and CHIP Payment and Access Commission (MACPAC) released its March 2024 Report to Congress on Medicaid and CHIP. The report focused on three issues of interest to Congress: how state Medicaid agencies can improve beneficiary engagement on Medical Care Advisory Committees; increasing the transparency of the denials and appeals process in Medicaid managed care; and the Commission’s work on Medicaid disproportionate share hospital allotments to states. Read More
Senators Push to Include PBM Legislation in Upcoming Spending Bill Package. Modern Healthcare reported on March 14, 2024, that Senate Finance Committee Chair Ron Wyden (D-Oregon) and ranking member Mike Crapo (R-Idaho) are pushing to include legislation that would impose stronger regulations on pharmacy benefit managers (PBMs) in the second set of spending bills that must reach President Biden by March 22 to avoid a government shutdown. The legislation includes two Finance Committee bills that would implement new transparency rules for PBMs, ban spread pricing, and impose restrictions to PBMs in the private health insurance market. Legislators previously abandoned the legislation following disagreements over details. Read More
State Medicaid Fraud Units Recovered $1.2 Billion in 2023, OIG Report Finds. The U.S. Department of Health and Human Services Office of Inspector General released on March 14, 2024, a report showing that state Medicaid Fraud Control Units recovered $1.2 billion in civil actions and criminal convictions for fraud and patient abuse in 2023. Recoveries increased by $100 million, up from $1.1 billion in 2022. Read More
Medicare Billed $101.4 Million for Remote Monitoring Services in 2021, KFF Finds. KFF Health News reported on March 18, 2024, that since Medicare began allowing physicians to get paid for remote monitoring services in 2019, services billed to Medicare grew from fewer than 134,000 to 2.4 million in 2021. Total Medicare payments for the four most common billing codes for remote monitoring increased from $5.5 million in 2019 to $101.4 million in 2021. Federal law enforcement officials are conducting investigations after a surge in complaints about some remote patient monitoring companies. Read More
6.4 Million Individuals Were Uninsured and Eligible for Medicaid in 2022, KFF Finds. KFF released on March 15, 2024, an issue brief that examines the characteristics of nonelderly uninsured individuals eligible for Medicaid and the Children’s Health Insurance Program (CHIP), using national survey data from 2022, and eligibility levels for Medicaid from 2023. Among the 6.4 million nonelderly people who are uninsured and eligible for Medicaid or CHIP, 4.2 million are adults and 2.2 million are children. Additionally, over three-quarters of the 6.4 million people who are uninsured and Medicaid eligible reside in expansion states, which have higher Medicaid income eligibility for adults than non-expansion states. Read More
Industry News
Change Healthcare’s Competitors Waystar, Availty Offer Services Following Cyberattack. Modern Healthcare reported on March 19, 2024, that companies such as Waystar and Availty have stepped in to provide solutions to payers and providers following the cyberattack at Change Healthcare. Waystar is currently offering a temporary program for providers affected by the cyberattack, which reportedly allowed one health system to process nearly 120,000 claims transactions. Availty has reported a 40 percent increase in daily claims volume after assisting 300,000 providers and 50 health plans move approximately $9 billion in pending claims. Read More
Elevance to Acquire Kroger’s Specialty Pharmacy Business. The Kroger Company announced on March 18, 2024, that it has entered a definitive agreement to sell its specialty pharmacy business to Elevance subsidiary CarelonRx. Kroger’s specialty pharmacy provides services such as education, counseling, side effect management, financial assistance, and personalized care to individuals with chronic illness that require complex care. The transaction is subject to regulatory approval and is expected to close in the second half of 2024. Read More
UnitedHealth Group Pays $2 Billion to Providers Affected by Cyberattack. CNBC reported on March 18, 2024, that UnitedHealth Group has paid out more than $2 billion to healthcare providers who have been affected by Change Healthcare’s cyberattack and is releasing medical claims preparation software. UnitedHealth is not expecting repayments until claims flows return to normal. Results from an American Hospital Association survey found that 94 percent of surveyed hospitals have experienced financial disruptions from the Change Healthcare attack and more than 60 percent of the 1,000 hospitals estimated the revenue loss to be around $1 million per day. Read More
UnitedHealth Group’s Pharmacy Network Resumes Operations. Health Payer Specialist reported on March 14, 2024, that UnitedHealth Group indicated that the pharmacy network at its subsidiary Change Healthcare is back online after the company experienced a cyberattack in February. Change Healthcare is still in the process of bringing some pharmacies online, however. UnitedHealth Group has identified the route utilized by hackers to conduct the cyberattack and has launched a full forensic analysis. Read More
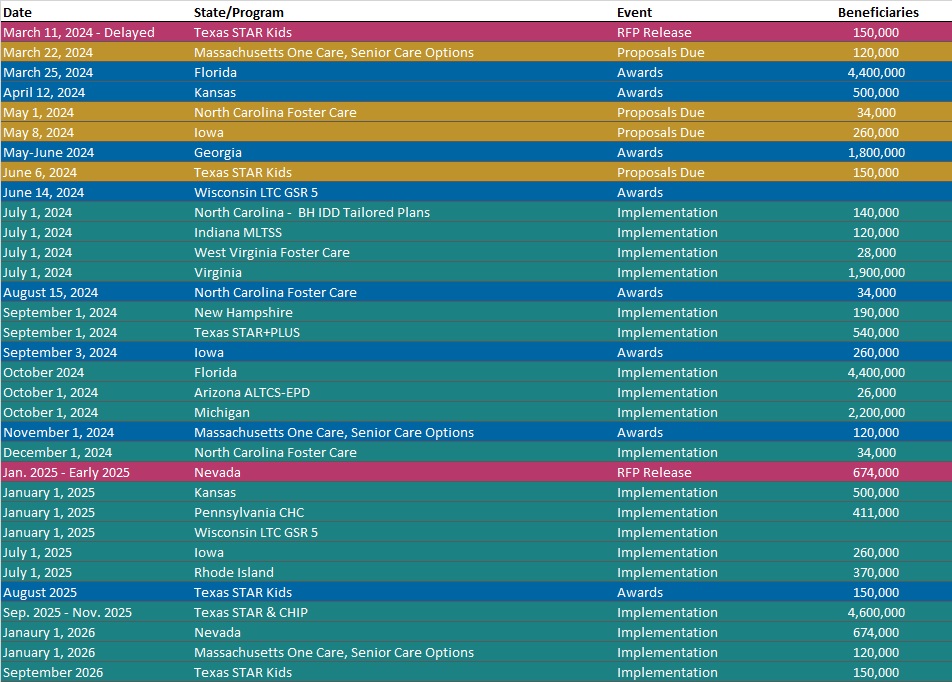
RFP Calendar
HMA News & Events
Leavitt Partners, an HMA Company, Report:
Delivering on the Promise of a Patient First Health Care System: A Compromise Approach to Site-Neutral Payments. Leavitt Partners released a new policy framework that proposes a compromise path forward on implementing site-neutral payments. Medicare is an incredibly important program, providing more than 65 million Americans with access to robust health care benefits. As the program has grown, mounting concerns have been raised about its affordability for Medicare beneficiaries and the sustainability of its spending and financing structure. As hospitals play an irreplaceable role in their communities, providing lifesaving services to every person, regardless of their background or insurance situation, it is important to fully support them in their efforts to fulfill their mission. At the same time, however, it is critical that policymakers address payment distortions that are driving up costs to Medicare beneficiaries and the Medicare program, including the lack of site-neutral payments. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Colorado RAE Enrollment is Down 4.1%, Jan-24 Data
- Louisiana Medicaid Managed Care Enrollment is Down 1.1%, Jan-24 Data
- Minnesota Medicaid Managed Care Enrollment is Down 13.3%, Mar-24 Data
- Missouri Medicaid Managed Care Enrollment is Down 5.4%, Feb-24 Data
- Missouri Medicaid Managed Care Enrollment is Down 5.1%, Mar-24 Data
- Montana SNP Membership at 5,590, Nov-23 Data
- Nevada SNP Membership at 35,629, Nov-23 Data
- Tennessee SNP Membership at 144,451, Nov-23 Data
- Virginia Medicaid Managed Care Enrollment is Down 0.9%, 2023 Data
- Virginia Medicaid MLTSS Enrollment is Flat, 2023 Data
- Washington SNP Membership at 122,893, Nov-23 Data
- West Virginia SNP Membership at 36,132, Nov-23 Data
- Wyoming SNP Membership at 2,195, Nov-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama Community Waiver Program Services RFP, Mar-24
- Alabama Medicaid Recovery Audit RFP, Mar-24
- Arizona AHCCCS Contract Amendments, 2023
- New York Self Directed Care Initiative RFI, Mar-24
- Utah Medicaid MAC Pharmacy Pricing RFP, Mar-24
Medicaid Program Reports, Data, and Updates:
- Alabama Medicaid Unwinding Report, Jan-24
- Colorado PHE Medicaid Redeterminations Monthly Report to CMS, Feb-24
- Florida PHE Medicaid Redeterminations Monthly Report to CMS, Jan-24
- Kentucky PHE Medicaid Redeterminations Monthly Report to CMS, Jan-24
- Maine PHE Medicaid Redeterminations Monthly Report to CMS, Jan-24
- North Carolina Medicaid Annual Reports, SFY 2015-23
- South Carolina PHE Medicaid Redeterminations Monthly Reports to CMS, Feb-24
State Overviews:
- Updated: Nebraska Managed Medicaid Opportunity Assessment and State Medicaid Landscape
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
