HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Federal Policymakers Consider Current and Future Spending Measures on Simultaneous Tracks

- Arizona Medicaid to Reimburse for Community Health Worker Organizations

- Arkansas Governor Approves Committee, Strategic Plan to Support Maternal Health

- Florida House Passes Bill to Establish Rural Emergency Hospitals

- Georgia Senate Committee Advances Bill to Relax Certificate-of-need Regulations

- Minnesota House Committee Holds Hearing on Bills to Support HRSNs Through Section 1115 Waiver

- Nevada Receives Federal Approval Allowing Medicaid Funds to Cover Housing, Supportive Services

- Oregon Awards $17 Million to CBOs Supporting Health Equity

- Texas Announces Awards for STAR, CHIP RFP

- Texas FQHCs Receive $19.3 Million to Expand Services to Underserved, Uninsured Populations in 2023

- Virginia Postpones Several Caregiver Policies

- Redetermination Updates: Montana, Texas

- States Pause Nursing Home Staffing Penalties Amid Review of CMS Rule

- CMS Permits States to Expand Medicaid Behavioral Health Professionals, Claim Federal Match Funding for Nurse Advice Lines

- HHS to Investigate Cyberattack at UnitedHealth Group’s Change Healthcare

- White House Pressures UnitedHealth Group to Increase Funding for Providers Affected by Cyberattack

In Focus
Federal Policymakers Consider Current and Future Spending Measures on Simultaneous Tracks
This week, our In Focus section covers Congress’s and the Administration’s parallel efforts to finalize fiscal year (FY) 2024 spending bills and begin the budget process for FY 2025.
Congress approved a bipartisan package for some of the FY 2024 spending bills, and on March 9, 2024, President Biden signed the Consolidated Appropriations Act of 2024 into law (PL 118-42). Programs funded through this measure include the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and other federal nutrition supports, rental assistance for safe and affordable housing, and veterans medical care and benefits.
Several mandatory funding extensions of public health programs and health-related policies also found their way into the 2024 consolidated appropriations package, including extending the Community Health Center Fund, delaying reductions in the disproportionate share hospital allotments, defining Certified Community Behavioral Health Centers (CCBHCs) as a Medicaid service, extending incentive payments for certain Medicare providers, and mitigating the impact of cuts to the Medicare physician fee schedule.
These policies, however, addressed a narrower set of issues than the expansive and bipartisan legislation that has been moving through both chambers of Congress. For example, House and Senate members have worked on respective bipartisan policies affecting price transparency, pharmacy benefit managers, and Medicare site-neutral policies, among others.
Meanwhile, President Biden released the FY 2025 Budget proposal March 11, 2024, kicking off the annual budget process. Like the administration’s FY 2024 budget proposal, the FY 2025 plan emphasizes deficit reduction and continues to make equity and Medicare solvency cornerstones of the budget. Health-related priorities include expanding access to affordable healthcare services, lowering drug costs, improving maternal health, addressing the mental health and substance use disorder crises, and enhancing biodefense and preparedness activities.
Check out the FY 2025 budget analysis from Leavitt Partners, a Health Management Associates, Inc. (HMA), company, here, and a deeper dive into the Consolidated Appropriations Act of 2024 here.
What We’re Watching
Congress is continuing negotiations on the outstanding spending bills, including the one that funds the Departments of Health and Human Services, Labor, and Education through September 2024. Lawmakers are working to reach an agreement before the next funding deadline of March 22.
The administration’s FY 2025 budget proposals are generally being characterized as a blueprint for President Biden’s re-election campaign and, if successful, a policy agenda for his second term. Though Congress has already begun holding hearings on the budget request, members on both sides of the aisle will likely focus on issues that resonate in an election year.
Regardless of the outcome of the November elections, Congress has an opportunity to address unfinished business during the lame duck session later this year.
HMA and Leavitt Partners collaborate to monitor legislative and regulatory developments in healthcare and adjacent spaces and to assess the impact of policy changes on the healthcare industry.
HMA Roundup
Arizona
Arizona Medicaid to Reimburse for Community Health Worker Organizations. The Arizona Health Care Cost Containment System (AHCCCS) announced on March 11, 2024, that organizations that employ Community Health Workers (CHWs) will be able to register as AHCCCS providers and receive reimbursement for Medicaid services. CHW organizations will be required to submit a list of all employed certified CHWs, adhere to AHCCCS policies when billing for CHW services, and be certified by the Arizona Department of Health Services. Read More
Arkansas
Arkansas Governor Approves Committee, Strategic Plan to Support Maternal Health. The Arkansas Advocate reported on March 6, 2024, that Arkansas Governor Sarah Huckabee Sanders signed an executive order to create a committee that will develop a comprehensive statewide strategic health plan aimed at improving maternal health. The strategic plan goals include connecting more pregnant and postpartum women with healthcare providers and advertising care and coverage options to pregnant Arkansans to improve the state’s collection of maternal health data. The committee is required to report its progress to Sanders in six months. Sanders has opposed extending Medicaid postpartum coverage to 12-months, saying that doing so would be duplicative of existing programs. Read More
Florida
Florida House Passes Bill to Establish Rural Emergency Hospitals. Health News Florida reported on February 29, 2024, that the Florida House passed a bill, sponsored by Senator Corey Simon (R-Tallahassee), that would establish a category of rural emergency hospitals in the state that could receive Medicare payments to provide emergency services, observation care, and outpatient services. The bill, intended to increase health access in rural areas, next heads to Governor Ron DeSantis for review. Read More
Georgia
Georgia Senate Committee Advances Bill to Relax Certificate-of-need Regulations. The Georgia Recorder reported on March 11, 2024, that the Georgia Senate Committee on Regulated Industries and Utilities has advanced a bill that would scale back certificate-of-need regulations and form a comprehensive health coverage commission. The Senate Committee also provided changes to the bill that would make it easier to open psychiatric and substance abuse inpatient facilities and rural hospitals. Under the revision, freestanding birth centers would be exempt from the certificate-of-need process. The bill now moves to the full Senate for further consideration. Read More
Illinois
Illinois Representative Introduces Legislation to Ban Medicaid Prior Authorization for Mental Health Drugs. WGEM reported on March 7, 2024, that Illinois Representative Lindsey LaPointe (D-Chicago) has introduced a bill which would allow Medicaid patients to obtain mental health medications without prior authorization. This comes after Illinois Governor JB Pritzker called on lawmakers for a complete prior authorization ban for mental health medications. Read More
Kentucky
Kentucky Supreme Court Holds Hearing on Elevance Medicaid Managed Care Contract Protest. The Kentucky Lantern reported on March 7, 2024, that the Kentucky state Supreme Court held a hearing on a dispute between Elevance Health, who failed to win a contract in 2020 for the state’s Medicaid managed care procurement, and contract winners, CVS/Aetna, Humana, Molina, UnitedHealthcare, and Centene/WellCare. Successful bidders are requesting that the Supreme Court uphold a 2022 state Court of Appeals ruling that Elevance was rightfully excluded from receiving a contract. Since 2020, Elevance has been allowed to retain a Medicaid managed care contract while legal disputes are pending. Current contracts run through December 31, 2024. Read More
Minnesota
Minnesota House Committee Holds Hearing on Bills to Support HRSNs Through Section 1115 Waiver. The Minnesota House of Representatives announced on March 7, 2024, that the House Human Services Finance Committee held a hearing on two bills, sponsored by Representative Mohamud Noor (DFL-Minneapolis), with both requiring the Department of Human Services to submit a Section 1115 Medicaid demonstration proposal to address health related social needs (HRSN). The first bill would require Medicaid to provide nutrition supports including medically tailored meals, and pantry items to children, pregnant women, and individuals exiting incarceration. The second bill would extend Medicaid coverage for care transition services to incarcerated individuals 30 days prior to their expected release. Read More
Mississippi
Mississippi to Allow 60-day Presumptive Medicaid Eligibility for Pregnant Woman. The Associated Press reported on March 13, 2024, that Mississippi lawmakers passed legislation allowing presumptive Medicaid eligibility for prenatal outpatient medical care for up to 60 days, beginning July 1. Medicaid would also be required to pay for services provided during the time of presumptive eligibility even if a woman’s application is ultimately rejected. It is estimated that the total cost to the Medicaid program will be just under $600,000 a year. Read More
Montana
Montana Disenrolls 127,214 Medicaid Beneficiaries During First 10 Months of Redeterminations. NBC Montana reported on March 12, 2024, that Montana has disenrolled 127,214 Medicaid beneficiaries during redeterminations from April 2023 through January 2024, including over 35,000 children. The state has renewed coverage for 105,495 beneficiaries. The state still has 45,081 pending eligibility cases from May through January. Read More
Nebraska
Nebraska Medicaid Procurement Lawsuit Reaches State Supreme Court. The York News Times reported on March 11, 2024, that Elevance/Healthy Blue’s lawsuit regarding Nebraska’s Medicaid managed care procurement has reached the state Supreme Court. Elevance initially filed the lawsuit in 2022, after it lost to bidders UnitedHealthcare, Centene/Nebraska Total Care, and Molina. Two of the bidders had failed to disclose hundreds of millions of dollars in payments to settle Medicaid-related investigations. Elevance maintains that taxpayer standing justifies its right to sue, given the relevance of expenditure of public funds to taxpayers. The state has refuted Elevance’s standing to sue. Read More
Nevada
Nevada Receives Federal Approval Allowing Medicaid Funds to Cover Housing, Supportive Services. The Nevada Current reported on March 13, 2024, that Nevada received federal approval for a pilot program which will use Medicaid funds to cover housing and supportive services through the state’s managed care plans: Anthem/Community Care Health Plan, Centene/SilverSummit Health Plan, UnitedHealthcare/Health Plan of Nevada, and Molina Healthcare. The four health plans will be required to submit plans to cover the services to the Centers for Medicare & Medicaid Services by the end of March. The state is also seeking approval of a Section 1115 demonstration proposal which would allow Medicaid to cover the cost of rent, temporary housing, and utilities for up to six months, and up to three meals per day for six months. Read More
New York
New York Legislators Reject Proposed Budget Amendment Altering Consumer Directed Personal Assistance Program. Crain’s New York reported on March 13, 2024, that New York legislators are pushing back against Governor Kathy Hochul’s proposed budget amendment which makes changes to the home care Consumer Directed Personal Assistance Program. Changes include limiting the number of financial intermediaries able to operate in the state, reducing wages for personal care aides, and expanding state oversight. A final spending plan is due April 1. Read More
New York Ambulette Companies Discontinue Operations in Parts of State. CBS News reported on March 8, 2024, that ten ambulette companies, which provide transportation for people with limited mobility including Medicaid enrollees, have discontinued service in New York’s Westchester County, citing that the state reimbursement is not adequate. The state Department of Health has previously estimated that the average ambulette trip costs $70; companies are being reimbursed about $53. Since 2019, at least 35 ambulette companies across the New York metro area have shut down. Read More
Oregon
Oregon Awards $17 Million to CBOs Supporting Health Equity. Oregon Health Authority’s (OHA) Public Health Division announced on March 6, 2024, that it has awarded $16.95 million to 44 new community-based organizations (CBOs) to support public health equity-based work. The funding will also support training and technical assistance. This second cohort of public health equity grants targeted rural communities, urban communities with service gaps, organizations that address the public health concerns and priorities of people who live with disabilities, and organizations serving communities at the intersection of multiple priority populations. Read More
Texas
Texas STAR, CHIP Managed Care Award Scoring Prompts Protest from Centene. Health Payer Specialist reported on March 13, 2024, that Centene plans to protest the Texas Health and Human Services Commission (HHSC)’s scoring of subsidiary Superior HealthPlan’s proposal for the state’s STAR & CHIP Managed Care Services procurement. HHSC issued a notice of intent to award on March 7 to Molina Healthcare, Blue Cross and Blue Shield, Aetna, UnitedHealthcare, Amerigroup, Dell Children’s Health Plan, Superior HealthPlan, Humana, El Paso First Health Plans, Community Health Choice, Scott and White Health Plan, and Parkland Community Health Plan. The protest period ends March 17. Centene previously reached a $165.6 million settlement with the state over allegations that it had breached Texas’s Medicaid fraud prevention law in September 2022. Read More
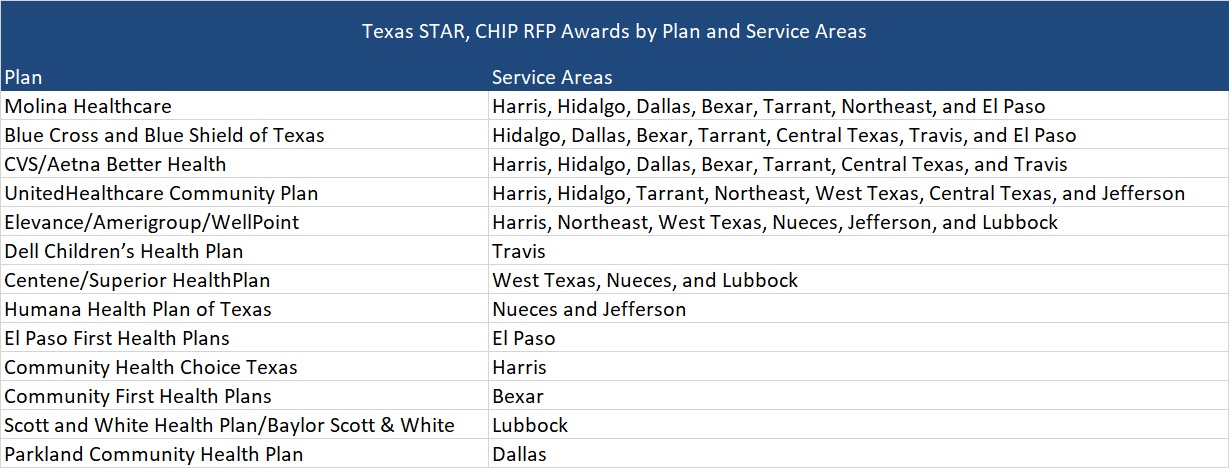
Texas Announces Awards for STAR, CHIP RFP. The Texas Health and Human Services Commission announced its intention to award State of Texas Access Reform (STAR) and Children’s Health Insurance Program (CHIP) Medicaid managed care program contracts to Molina Healthcare of Texas, Blue Cross and Blue Shield of Texas, CVS/Aetna, UnitedHealthcare Community Plan of Texas, Elevance/Amerigroup/Wellpoint, Dell Children’s Health Plan, Centene/Superior HealthPlan, Humana, El Paso First Health Plans, Community Health Choice Texas, Community First Health Plans, Scott and White Health Plan/Baylor Scott & White, and Parkland Community Health Plan. The state had previously announced that it would not award more than seven regions to any single managed care organization, which impacted three of the incumbents that were in more than seven regions. Molina won in seven regions (down from eight), Amerigroup was awarded in six regions (down from 11) and Superior won in three regions (down from 13). Three incumbents did not receive awards.
Implementation is expected between September and November 2025, and contracts will serve more than 4.6 million members. Contracts will run for six years, with three two-year renewal options, not to exceed a total contract term of 12 years. Read More
Texas FQHCs Receive $19.3 Million to Expand Services to Underserved, Uninsured Populations in 2023. The Texas Department of State Health Services (DSHS) announced on March 11, 2024, that several state health centers are now offering expanded services to underserved and uninsured populations after the DSHS Federally Qualified Health Center (FQHC) Incubator Program provided a total of $19.3 million in grant funding to FQHCs, FQHC look-alikes, and non-profit health centers in 2023. DSHS awarded grants ranging from $500,000 to $1 million to 35 entities in order to build new clinics, renovate existing facilities, purchase equipment and mobile health units, and hire additional staff and providers. The state legislature appropriated an additional $40 million in funding for the program in 2024. Read More
Texas Disenrolls 2,082,090 Medicaid Beneficiaries During First 10 Months of Redeterminations. The Texas Department of Health and Human Services announced that it has disenrolled 2,082,090 Medicaid beneficiaries based on eligibility redeterminations conducted from April 1, 2023, through February 20, 2024. Of those disenrolled, 1,380,152 lost coverage due to procedural reasons. Children made up about 1.3 million of those disenrolled. The state renewed coverage for 1,903,431 beneficiaries, and 701,938 individuals have been referred to the Marketplace. The state has 237,963 pending eligibility cases. Read More
Utah
Utah Receives Approval for Genetic Testing, Housing-Related Program, and Other Changes to State’s 1115 Demonstration Program. The Centers for Medicare & Medicaid Services announced on March 8, 2024, that it has approved Utah’s Medicaid Reform 1115 Demonstration amendments, effective through June 30, 2027. Under the waiver amendment, the state may provide coverage for in vitro fertilization and genetic testing services for eligible individuals ages 18 through 35 and for fertility preservation treatment for eligible individuals diagnosed with cancer. The state also received approval to increase the premium subsidy amount for the Children’s Health Insurance Program. Lastly, the amendment adds four risk factors to the state’s Housing Related Services and Supports demonstration program to align program eligibility with eligibility for the Targeted Adult Group. Read More
Utah Extends Postpartum Medicaid Coverage to 12 Months. The Centers for Medicare & Medicaid Services announced on March 8, 2024, that Utah is extending postpartum Medicaid coverage from 60 days to 12 months. An additional 4,000 individuals will now be eligible for Medicaid and Children’s Health Insurance Program coverage for one year following pregnancy. Read More
Virginia
Virginia Postpones Several Caregiver Policies. 3WTKR reported on March 13, 2024, that Virginia has received federal approval to halt select policies from going into effect regarding Legally Responsible Individuals (LRIs), which are paid caretakers for a child with severe developmental disabilities. Two new policies did become effective as of March 1, which now limit family caregivers to 40 hours of paid personal care each week and families with a paid family caregiver are not eligible for respite services. The General Assembly will need to take action on a set of three bills which would eliminate requirements that parents prove no one else can care for their child and remove limits on who the employer of record could be. If no action is taken, remaining policies are scheduled to become effective in summer or fall of 2024. Read More
Washington
Washington Elevance/Wellpoint Appoints Lisa Bogard as President. Health Payer Specialist reported on March 8, 2024, that Wellpoint Washington, a subsidiary of Elevance, has appointed Lisa Bogard as the company’s president. Bogard most recently served as president and chief executive of Medicaid at Anthem Blue Cross and Blue Shield in Nevada. Read More
National
House Energy, Commerce Health Subcommittee Advances 19 Health Bills. CQ reported on March 12, 2024, that the House Energy and Commerce Health Subcommittee advanced 19 health bills to the full committee, including those regarding programs preventing burnout in healthcare professionals and providing grants to help hospitals treat emergencies in children. A bill sponsored by Representative Earl Carter (R-Georgia), that would delay a Medicare plan moving payments for oral phosphate binders into a payment model for end stage renal disease to 2033, advanced despite opposition from the majority of the committee’s Democrats. Representative Diana Harshbarger (R-Tennessee) sponsored a bill that would make permanent a COVID-19 era waiver allowing independent physicians with onsite pharmacies to mail medications directly to their patients. Other bills that advanced aim to improve research regarding Alzheimer’s disease and stillbirths, efforts to improve training for rural emergency medical services, and the provision of respite care for family caregivers. Read More
CMS Website Newly Provides Support to Improve Medicaid Care for Sickle Cell Disease. The Centers for Medicare & Medicaid Services (CMS) released on March 11, 2024, a new website and informational resources on Medicaid and Children’s Health Insurance Program (CHIP) coverage for sickle cell disease (SCD) treatments. These developments complement CMS’ Cell and Gene Therapy Access Model, announced earlier this year. The website includes information related to demographics, health, and healthcare of individuals with SCD, and quality improvement tools that states can use to improve care for individuals with SCD. The agency also posted resources addressing access to out-of-state Medicaid providers, Medicaid-optional benefits for SCD, and potential value-based purchasing agreements between states and manufactures for certain drugs. Read More
President Signs $460 Billion Federal Spending Bill that Includes Healthcare Policies. Fierce Healthcare reported on March 10, 2024, that Congress passed and President Biden signed into law a $460 billion spending package, preventing a partial government shutdown through September. The spending package includes six out of the 12 annual federal appropriation bills. The compromise bill also delays an $8 billion reduction in Medicaid disproportionate share hospital payments for one year, provides some relief from Medicare’s pay cut for physicians, and increases funding for federally qualified health centers. Congress must pass the second set of six spending bills by March 22. Read More
States Pause Nursing Home Staffing Penalties Amid Review of CMS Rule. Modern Healthcare reported on March 12, 2024, that Illinois, Rhode Island, and New York have all paused penalties for nursing homes that violate staffing mandates in order to prevent limited access to care and facility closures. Opponents and advocates of nursing home staffing minimums have noted that states’ suspension of staffing rules may indicate the infeasibility of the Centers for Medicare & Medicaid’s nursing home minimum staffing standards final rule, particularly amid current staffing shortages. The White House Office of Management and Budget began reviewing the final rule March 1. Read More
President Biden Releases FY 2025 Budget Proposal. ABC News reported on March 11, 2024, that President Joe Biden released his fiscal year (FY) 2025 budget proposal, which includes efforts to build on the Medicare drug negotiations under the Inflation Reduction Act. Specifically, the proposal would hasten the pace of negotiations, increase the number of negotiable drugs, and extend the $2,000 out-of-pocket prescription drug cost cap to the commercial market. The budget plan also requests Congress provide $150 billion over 10 years to strengthen Medicaid home and community-based services. The Administration included a proposal for states to extend the existing 12-month continuous eligibility for all children to 36 months, and allows states to provide continuous eligibility for children from birth until they reach six years old. In addition, the President is asking Congress to agree to offer universal prekindergarten education, provide 12 weeks of paid family and medical leave, and expand anti-poverty tax credits among other proposals. Read More
Congress Considers Bill to Permanently include Certified Community Behavioral Health Centers in Medicaid. Behavioral Health Business reported on March 8, 2024, that Congress is currently considering a bill, sponsored by Representatives Doris Matsui (D-California) and Larry Buschon (R-Indiana), that would allow state Medicaid programs to make community behavioral health centers (CCBHCs) a permanent service option. CCBHCs, which provide outpatient mental health and addiction treatment as well as social and support services, are currently only offered through a temporary waiver demonstration program. (Editor’s note: Similar legislative language was included in the Consolidated Appropriations Act, 2024 signed into law by President Biden on March 10, 2024). Read More
Biden Administration to Push for Medicaid Expansion, Mental Health Parity, Continuous Medicaid Coverage for Kids in State of the Union. The White House announced on March 7, 2024, that during the State of the Union address, President Joe Biden will call on Congress to provide Medicaid-like coverage in the 10 states that have not adopted Medicaid expansion, push for continuous Medicaid coverage for children until they turn 6, improve access to mental health services and extend mental health parity protections to Medicare beneficiaries, and strengthen rules for nursing home staffing. Biden will focus on expanding Medicare’s authority negotiate prices for at least 50 prescription drugs each year, cap Medicare copayments at $2 for common generic drugs, and extend the $2,000 cap on out-of-pocket drug costs beyond Medicare to all private plans. Read More
CMS Permits States to Expand Medicaid Behavioral Health Professionals, Claim Federal Match Funding for Nurse Advice Lines. The Centers for Medicare & Medicaid Services (CMS) issued on February 26, 2024, a letter to state Medicaid Directors that permits states to expand the pool of skilled professional medical personnel (SPMP) to include additional behavioral health professionals, such as those with master’s-level education that are licensed as independent practitioners. Medicaid agencies utilize SPMPs to ensure that program administration aligns with clinical best practices, and expansion will authorize states to claim higher administrative federal match for their work. The letter also allows states to claim administrative federal match dollars for nurse advice lines. Read More
Less Than a Third of Primary Care Physicians Participated in Both Medicaid, Marketplace Plans in 2020, Study Finds. Health Payer Intelligence reported on March 7, 2024, that fewer than three in 10 primary care physicians participating in Medicaid also participated in an average Marketplace network, according to a study published in JAMA. The study utilized 2020 physician directory data to examine Medicaid-Marketplace overlap in 15 states. Percentage of overlap varied from 8.5 percent in South Carolina to 59.6 percent in Iowa, while the mean overlap was 28.8 percent. Read More
Industry News
HHS to Investigate Cyberattack at UnitedHealth Group’s Change Healthcare. Health Payer Specialist reported on March 13, 2024, that the U.S. Department of Health and Human Services (HHS) Office for Civil Rights released a letter indicating that it will investigate UnitedHealth Group’s compliance with the Health Insurance Portability and Accountability Act following the February cyberattack on subsidiary Change Healthcare. UnitedHealth Group may incur a fine as a result and has stated that it will comply with HHS’s probe. The Department of Justice previously launched an antitrust probe into the company in 2023, and the Federal Trade Commission is currently investigating its pharmacy benefit manager, Optum Rx. Read More
White House Pressures UnitedHealth Group to Increase Funding for Providers Affected by Cyberattack. Health Payer Specialist reported on March 12, 2024, that White House officials have called on UnitedHealth Group to take additional steps to ensure emergency funding is available for providers affected by disabled payment systems due to the cyberattack on Change Healthcare which began in February. UnitedHealth is expected to reinstate Change Healthcare’s electronic payments and claims processing platform during the week of March 18. Read More
CMS Announces Availability of Payments to Providers, Suppliers Following Cyberattacks at UnitedHealth Group’s Change Healthcare. The Centers for Medicare & Medicaid Services (CMS) announced on March 9, 2024, that it will provide accelerated payments to Part A providers and advance payments to Part B suppliers facing claims disruptions as a result of the cyberattack at UnitedHealth Group’s subsidiary Change Healthcare. The payments will be granted in amounts representing thirty days of claims payment, with the average value based on total claims paid between August 1, 2023, and October 31, 2023, divided by three. Payments will be repaid automatically from Medicare claims for a 90-day period. CMS has indicated that it will continue to monitor the incident and resulting disruptions. Read More
UnitedHealth Group to Restore Change Healthcare Systems Following Cyberattacks. Modern Healthcare reported on March 7, 2024, that UnitedHealth Group has reopened Change Healthcare’s electronic prescribing platform and is expected to reinstate the electronic payments platform on March 15 and the medical claims network the week of March 18 after experiencing a cyberattack in February. UnitedHealth Group has indicated that pharmacy partners and associations will be reimbursed for pharmacy claims filled during the systems outage. Some providers will also have access to an interest-free loan program. Prior authorization requirements for most outpatient care and utilization review for Medicare Advantage inpatient care has been suspended until March 31. Read More
UnitedHealth Group Faces Lawsuits in TN, MN Over Cyberattack at Change Healthcare. Modern Healthcare reported on March 6, 2024, that UnitedHealth Group is facing at least five lawsuits filed in Tennessee and Minnesota federal courts after a cyberattack at Change Healthcare disabled the payment processing systems. The lawsuits seek class action status and allege that the cybersecurity breach compromised personal information and could have been prevented with proper security measures. UnitedHealth Group is working to restore operations but has not provided comment on the lawsuits. Read More
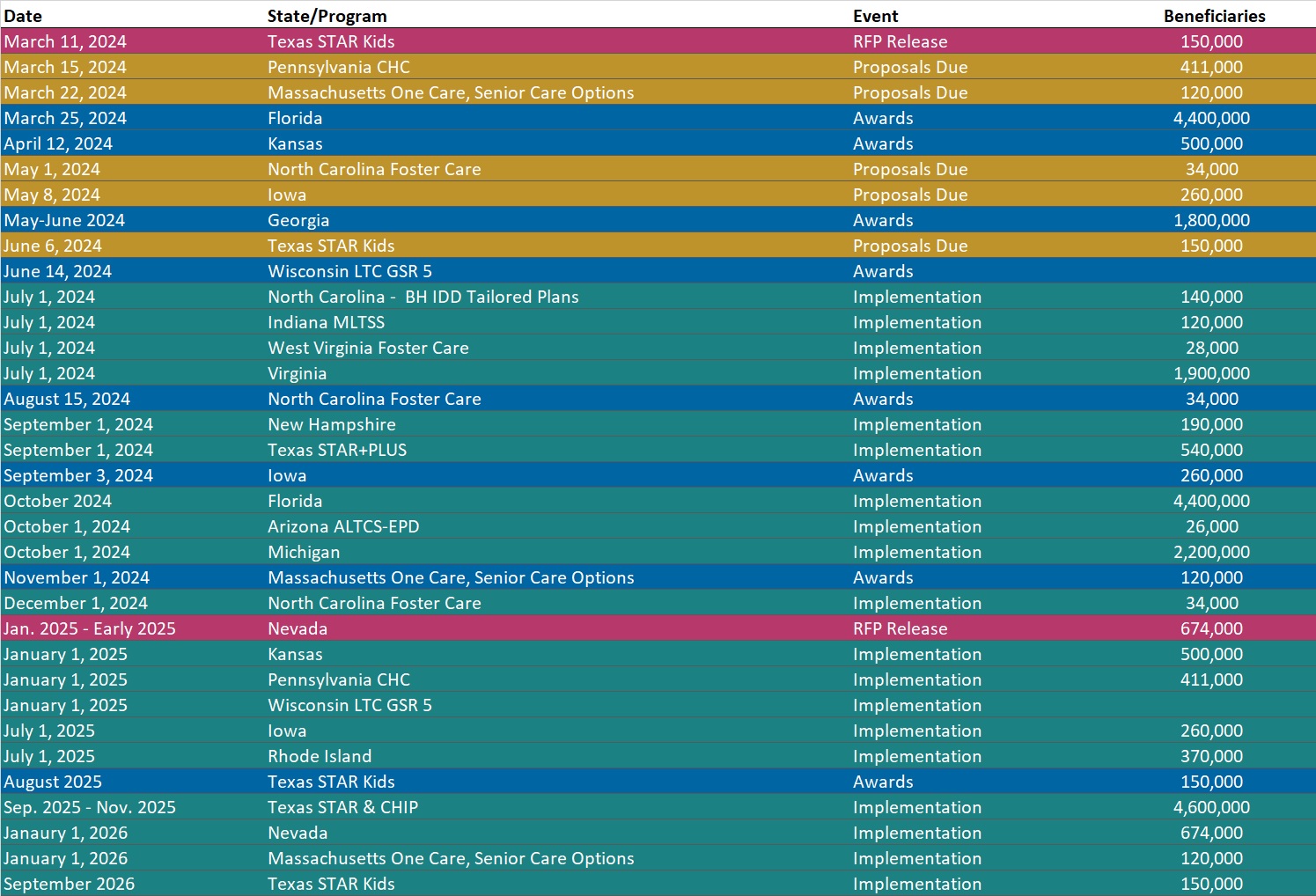
RFP Calendar
Company Announcements
MCG Press Release:
MCG Recognizes CareSource with 2023 Richard L. Doyle Award for Transforming Inpatient Authorization Workflows. MCG Health has named CareSource a recipient of its 2023 Richard L. Doyle Award for Innovation and Leadership in Healthcare. The nonprofit managed care organization (MCO) was recognized for successfully collaborating with hospitals to transform the inpatient authorization process. CareSource’s winning initiative involved partnering with Cleveland Clinic and University Hospitals to improve turnaround times for authorization responses and reduce administrative burden. Read More
HMA News & Events
HMA Webinars:
Substance Use Disorder (SUD) Ecosystem of Care: Pivoting to Save Lives Part 1–Overview, and The Role of Health Promotion and Harm Reduction Strategies. Thursday, March 14, 2024, 12 PM ET. Join us for part 1 of our 4-part webinar series, ‘Substance Use Disorder Ecosystem of Care: Pivoting to Save Lives”. In this session we will provide an overview of the series and take a look at the services and support that comprise a system of care for people who are not yet in treatment. Register Here
