HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Medicaid Unwinding Check-in: Data Informed Observations to Guide Future Action

- Alabama Legislators Hear from Arkansas, North Carolina Officials on Medicaid Expansion

- Arkansas Cancels Medicaid Dental Services Procurement; Fails to Reach Agreement with Bidders

- California to Adopt Health Care Spending Limit Beginning 2025

- Colorado Extends Medicaid Eligibility for Beneficiaries Living with Disabilities

- Connecticut House Passes Bill Aimed at Improving Elder Health Care System

- Illinois CBOs to Receive More than $5 Million in Funding for Maternal, Infant Healthcare

- Kansas to Implement Supplemental Waiver to Shorten IDD, Physical Disability Waiver Waitlists

- Mississippi Medicaid Expansion Bill Heads to House, Senate for Vote

- Oregon Medicaid Program Offers Equipment to Protect Beneficiaries Against Climate Change

- CMS, NCQA Grant Two Week Extension for Insurers to Submit Star Quality Data

- FTC Finalizes Rule to Prevent Digital Health Apps from Releasing Sensitive Medical Data

- CVS to Acquire Medicare Advantage Broker Hella Health

- More News Here

In Focus
Medicaid Unwinding Check-in: Data Informed Observations to Guide Future Action
In this week’s In Focus section, Health Management Associates (HMA) Managing Director Matt Powers and Associate Principal Lora Saunders discuss observations and perspectives as we approach completion of the Medicaid unwinding.
Overview
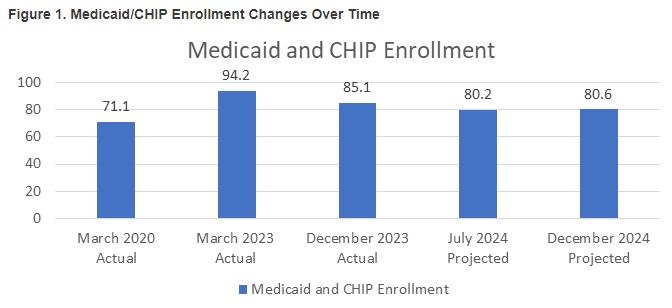
In response to the COVID-19 pandemic, CMS offered states an enhanced federal match in exchange for states pausing Medicaid disenrollments. As a result, Medicaid enrollment increased from around 71 million at the start of the pandemic to more than 92 million in December 2022, when Congress passed a bill to end the “continuous eligibility” provision. States began to resume normal (pre-pandemic) redetermination activities in early 2023—a massive undertaking of attempting to reach and verify eligibility for the then 94 million Medicaid enrollees known as “unwinding.”
More than 70 percent of the efforts that will precipitate the largest one-year drop in enrollments since the program’s inception in 1965 have been completed. The enrollment reductions to date have been virtually identical to HMA’s aggregate projections, and overall enrollment remains well above pre-pandemic levels. Perhaps most importantly, the Medicaid unwinding has put policymakers in a position to better evaluate how to improve enrollment and redetermination processes going forward.
Figure 1 summarizes pre-pandemic enrollments, unwinding enrollments, and the projected end of 2024 enrollment. If the current trend holds, national Medicaid enrollment will be approximately 80 million enrollees—down from the 94 million pre-unwinding enrollment peak and nearly 10 million greater than the 71 million pre-pandemic enrollment.
Our team’s assessment of the status of and data related to the Medicaid unwinding has led us to the following observations:
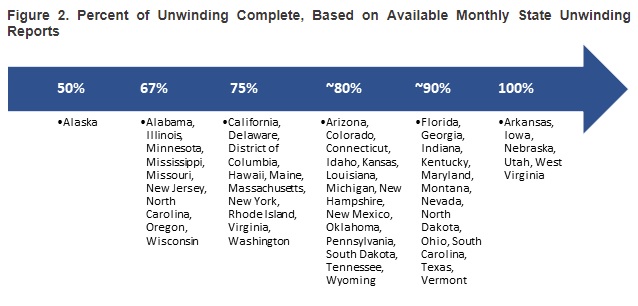
- Arkansas, Iowa, Nebraska, Utah, and West Virginia have completed the redetermination process. More than half of the states are within two months of finishing the process.
- The states that saw Medicaid enrollment grow the most under the continuous coverage policy are generally the same ones that are experiencing the greatest enrollment declines during the Medicaid unwinding.
- Some larger states—including California, New York, and Texas—have sizeable outstanding redeterminations.
- Nationally, more than 70 percent of all Medicaid enrollees have completed the redetermination process. Figure 2 points out how far along states are with the redetermination process as of late April 2024.
Medicaid Unwinding: The Road Ahead
As the Medicaid unwinding process enters its final phase in most states, we are looking back at the experiences and lessons that can be applied to make impactful changes to Medicaid eligibility policies, systems, and procedures.
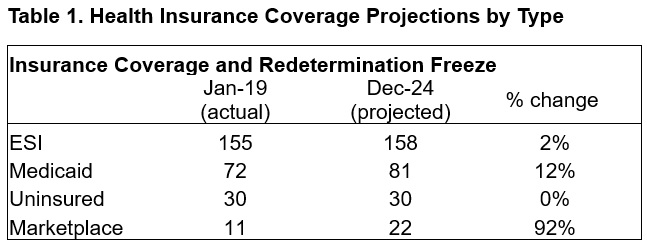
Despite the challenges that the pandemic presented, the safety net was tested and responded well. In early 2020, the number of employed Americans decreased from 158 million to 133 million, and unemployment levels quickly reached 15 percent. Many new healthcare policies targeted direct access issues (e.g., financial supports to providers and telehealth regulatory relaxations), whereas the Medicaid continuous coverage requirement was intended to mitigate the effects of the abrupt spike in unemployment and potential effects on healthcare insurance. Table 1 shows how HMA projects national coverage patterns to change by type of coverage from before the pandemic through the end of the Medicaid unwinding. While the number of people with employer-sponsored insurance (ESI) or uninsured remains essentially flat, Medicaid enrollment grows significantly, and marketplace enrollment nearly doubles. Myriad federal and state policy changes contributed to a remarkably stable uninsurance rate during one of the most volatile economic periods in the past century.
A next question for policymakers is whether, or to what extent, the rate of uninsured people can be sustained or reduced. The broad state adoption of policies to expand postpartum coverage to 12 months from two months and the nationwide January 2024 requirement for states to offer 12 months of continuous Medicaid coverage for children provide a coverage and continuity boost, especially given that nearly 40 million children will benefit from the new law. Other policy levers have the potential to be widely accepted and provide a further incentive to move people who are uninsured toward coverage, more stable insurance products, and more predictable outcomes and costs relative to the inefficiencies and ineffectiveness of non-coverage.
Pivoting to best practices and making policy changes permanent. Just as the relaxation of relatively rigid telehealth policies has become more accepted, post-Medicaid unwinding will provide a natural opportunity to assess best practices and consider permanent policy changes.
- Making Ex Parte Durable Policy. Evidence suggests that ex parte policies effectively reduce churn. Further refinement of longstanding ex parte policies is within reach. Ensuring ex parte appropriately manages both the complexities of household versus individual eligibility issues and addresses the weaknesses of unreliable member contact information can improve the likelihood that ex parte can effectively serve as durable policy.
- Pivoting from Paper to Electronic Communications. The Medicaid unwinding has seen more partnerships and innovation with state and federal workers, providers, managed care organizations, and consumer advocates, and allowed the increased use of mobile devices for outreach and engagement. Making more deliberate strides to simplify eligibility and move the eligibility platform, patient engagement, and member outreach to more reliable communication methods (e.g., email, text, and member portals rather than paper communication) while adhering to privacy and security requirements is a logical next step.
- Continuing to Measure Better. Call abandonment rates, call center wait times, and application processing times—metrics that focused on some of the key challenges to a successful redetermination and timely access to care—received greater attention during the unwinding but were frequently overshadowed by other primary metrics like “disenrollments” and “procedural terminations.” Though disenrollment data and procedural terminations could be used to identify potential areas of concern, their emergence as primary metrics often diverted energy from innovative engagement and redetermination efforts. A focus on contextualized metrics that provide actionable information will support effective oversight and monitoring.
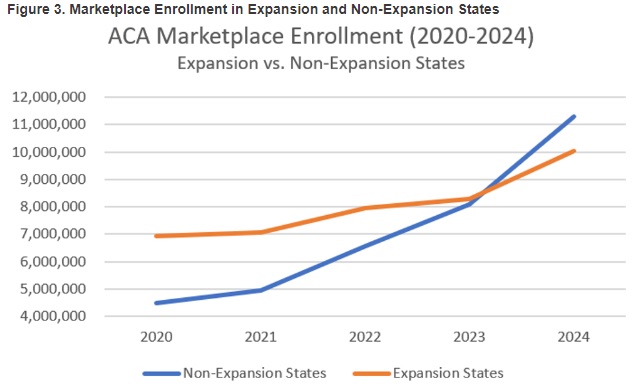
Marketplace growth may be the real story. Throughout the pandemic, marketplace enrollment has steadily increased, jumping nearly 90 percent from 2020 to 2024 and 30 percent from 2023 to 2024, to reach more than 21 million enrollees. Driving the growth in marketplace enrollment are temporarily increased marketplace subsidies and Medicaid unwinding public awareness campaigns.
- The marketplaces are proving to be a reliable source of coverage for consumers without health insurance access through ESI or other public programs, particularly in times of significant change such as the Medicaid unwind. With more marketplace enrollees and, therefore, broader risk pools, more health insurers are considering offering marketplace plans and are assessing competitive advantages like lower costs, broader provider networks, and more robust drug formularies.
- Figure 3 shows that marketplace growth in non-expansion states is far outpacing marketplace growth in Medicaid expansion states, suggesting that the key elements of the Affordable Care Act have developed deep roots.
HMA’s experts continue to monitor Medicaid unwinding developments. We are taking a comprehensive approach to assessing lessons learned and opportunities to improve Medicaid as state and stakeholder experiences and data continue to become available over the next two quarters.
For more information or questions about Medicaid unwinding developments, contact Matt Powers ([email protected]) and Lora Saunders ([email protected]).
HMA Roundup
Alabama
Alabama Legislators Hear from AR, NC Officials on Medicaid Expansion. The Alabama Reflector reported on April 25, 2024, that the Alabama House and Senate committees on health held a joint session in which state officials from Arkansas and North Carolina discussed the benefits, challenges, and strategies associated with implementing Medicaid expansion. North Carolina Representative Donny Lambeth (R-Forsyth) noted that Medicaid expansion has been cost-effective. Former secretary of the Arkansas Department of Human Services Cindy Gillespie described Arkansas’s established premium assistance program. Medicaid expansion would offer coverage to an additional 100,000 individuals in Alabama; however, some legislators remain opposed to the initiative. Read More
Arizona
Arizona Disenrolls 611,144 Medicaid Beneficiaries Since Redeterminations Began. Arizona Public Media reported on April 27, 2024, that Arizona has disenrolled 611,144 Medicaid beneficiaries and renewed coverage for 1,953,301 beneficiaries since redeterminations began in April 2023. More than 2.2 million Arizonans have full or partial Medicaid coverage, which is approximately 300,000 more than before the pandemic. The state has 1,892 pending eligibility cases to review. Read More
Arkansas
Arkansas Cancels Medicaid Dental Services Procurement; Fails to Reach Agreement with Bidders. The Arkansas Democrat Gazette reported on April 30, 2024, that Arkansas has cancelled its Medicaid dental managed care services procurement due to a stalemate in negotiations with vendors who bid on the contract. The state is reviewing options to either rebid the procurement or to move services back to fee-for-service. Read More
California
California Releases Medicaid Fiscal Intermediary Maintenance, Operations RFI. The California Department of Healthcare Services released on April 29, 2024, a request for information (RFI) regarding an upcoming procurement for a Fiscal Intermediary Maintenance and Operations contractor to support the California Medicaid Management Information System. Responses are due June 3, 2024. Read More
California to Adopt Health Care Spending Limit Beginning 2025. Politico Pro reported on April 24, 2024, that California’s Health Care Affordability Board voted to enact a new health care spending limit that will prevent total state health care expenditures from growing by more than three percent. The limit will be phased in over the next five years, beginning at 3.5 percent in 2025 and 2026, 3.2 percent in 2027 and 2028, and three percent in 2029. The spending cap will apply to the state’s health insurance plans, physician groups, hospitals, and other health entities. Read More
InnovAge Launches New CA PACE Program Center. InnovAge announced on April 24, 2024, that it has launched a Program of All-inclusive Care for the Elderly (PACE) program center in Los Angeles, California. The center will provide integrated healthcare and support services to seniors with Medicare and Medicaid coverage residing throughout West and South Los Angeles. InnovAge operates PACE centers in California, Colorado, New Mexico, Pennsylvania, Virginia, and Florida. Read More
Colorado
Colorado PDAB Review of Rare Disease Drug Costs Could Result in Capped Costs. The Colorado Sun reported on April 30, 2024, that the Colorado Prescription Drug Affordability Board (PDAB) is continuing to review prices for specific prescription drugs, which could eventually result in the Board capping how much patients and insurers must pay for prescription drugs, specifically for patients with rare diseases. Some patients and consumer advocacy groups are concerned about the unintended consequences of capping drug prices, including pharmaceutical companies potentially pulling their drugs from Colorado or pharmacists no longer stocking them. Read More
Colorado Extends Medicaid Eligibility for Beneficiaries Living with Disabilities. CBS News Colorado reported on April 25, 2024, that the Colorado Department of Health Care Policy and Financing will grant a 12-month extension for individuals with long-term disabilities to submit paperwork for Medicaid renewals due to technology issues within the state’s new case management system, known as CCM. State records show that CCM did not allow beneficiaries’ information from the old system to move to the new system, making it more difficult to process claims. Read More
Connecticut
Connecticut House Passes Bill Aimed at Improving Elder Health Care System. The Connecticut Mirror reported on April 29, 2024, that the Connecticut House passed a bill, sponsored by the Aging Committee, that would overhaul the state’s current elder care system by requiring additional oversight of home care workers, streamlining Medicaid access, incentivizing high quality care, and launching an online registry to make it easier for beneficiaries to locate caregivers. The bill would also create a presumptive eligibility program in which case managers and social workers could utilize screening tools to quickly determine Medicaid eligibility. The bill next heads to the Senate for review. Read More
Illinois
Illinois to Address Homelessness Services in Section 1115 Demonstration. Health News Illinois reported on April 26, 2024, that Illinois Governor JB Pritzker’s fiscal 2025 budget proposal includes $250 million to address homelessness, with $13 million aimed at reducing racial disparities. The state intends to offer homelessness services in its Section 1115 demonstration. A University of Illinois Chicago report found that Black individuals are eight times more likely to be unhoused than white individuals in Illinois. The report suggests that the state use additional funding to address disparities in homelessness and healthcare access. Read More
Community-based Organizations to Receive More than $5 Million in Funding for Maternal, Infant Healthcare. Health News Illinois reported on April 30, 2024, that five Illinois organizations will receive more than $5 million in federal funding to improve maternal and infant healthcare. The following organizations will each receive approximately $1 million from the U.S. Department of Health and Human Services (HHS): Access Community Health Network in Chicago, Cook County, SGA Youth & Family Services in Chicago, the University of Illinois, and Southern Illinois Healthcare Foundation in Sauget. The funds are part of $105 million in funding from HHS to support more than 100 community-based organizations providing maternal and infant healthcare. Read More
Illinois Safety Net Hospital Can Proceed With Lawsuit Over Medicaid Plan Payment Disputes, Court Rules. Cook County Record reported on April 25, 2024, that the Seventh U.S. Circuit Court of Appeals has ruled that Chicago-based safety net provider St. Anthony Hospital can sue Illinois over inadequate state regulatory oversight of Medicaid Managed Care Organizations (MCOs). The lawsuit claims certain Medicaid MCOs contracted by the state have repeatedly violated federal Medicaid rules, which require 90 percent of Medicaid claims to be paid within 30 days and 99 percent within 90 days. Read More
Iowa
Iowa Releases Medicaid Pharmacy Benefit Administration RFP. The Iowa Department of Health and Human Services released on April 24, 2024, a request for proposals seeking a contractor to provide Medicaid pharmacy benefit administration (PBA) services for claims processing and pharmacy clinical services. PBA services include point-of-sale claims adjudication, automated and manual prior authorization, provider and member communications, drug reporting and analytics for the fee-for-service population, and Medicaid managed care program oversight. Proposals are due June 12, 2024, with a notice of intent to award scheduled for July 3, 2024. The contract would have an initial two-year design, development, and implementation phase beginning October 1, 2024, and a five-year base operational term with three additional one-year renewal options. Read More
Kansas
Kansas Senate Fails to Move Medicaid Expansion Bill to Floor Debate. 13WIBW reported on April 29, 2024, that the Kansas Senate failed to secure enough votes to compel the full chamber to debate a Medicaid expansion bill pending in committee. Read More
Kansas to Implement Supplemental Waiver to Shorten IDD, Physical Disability Waiver Waitlists. The Topeka Capital Journal reported on April 26, 2024, that Kansas is developing a community support waiver option that would allow a limited set of services for Medicaid eligible individuals on the Intellectually and Developmentally Disabled (IDD) and Physically Disabled (PD) waitlists who do not need a comprehensive waiver slot. The waiver, which would not be implemented until 2026, includes supported employment and respite care services with a maximum service payment cap. Read More
Louisiana
Louisiana Plan Humana Healthy Horizons Invests in Health-related Social Needs. Humana Healthy Horizons announced on April 25, 2024, that it has invested $500,000 to support 24 nonprofit community organizations throughout Louisiana. The investments, ranging from $5,000 to $50,000 per organization, are aimed at addressing health-related social needs, with particular focus on maternal health. Read More
Maine
Maine Upholds Decision to Award Modivcare Statewide NEMT Contract. Maine Public reported on April 26, 2024, that the Maine Bureau of General Services has upheld the decision to award Colorado-based Modivcare Solutions a statewide contract for non-emergency medical transportation (NEMT) services. Incumbents Penquis Community Action Agency and Waldo Community Action Partners previously appealed the decision citing unfair scoring of proposals. Modivcare’s contract, estimated to be worth $750 million, will run for an initial two-years beginning July 1, with renewals for up to 10 years. Read More
Maryland
Maryland Health Department to Conduct Studies on Dental Coverage, Obesity Treatment. Maryland Matters reported on April 29, 2024, that the Maryland Department of Health and related agencies indicated at the Maryland Medicaid Advisory Committee meeting that they will conduct 13 new reports and studies required by bills approved during the 2024 legislative session. One bill, sponsored by Delegate Heather Bagnall (D-Anne Arundel), calls for a study to examine the feasibility of reimbursing providers for full or partial denture work. Other bills require an investigation into weight-loss medications and the potential fiscal and operational impact of implementing an Employed Individuals with Disabilities program covering those aged 65 or older. The studies must be completed and presented to lawmakers before December 1. Read More
Mississippi
Mississippi Medicaid Expansion Bill Heads to House, Senate for Vote. The Clarion Ledger reported on April 30, 2024, that Mississippi legislators have reached a final compromise on a Medicaid expansion bill that will now head to the Senate and House for a vote. The bill would expand Medicaid for individuals aged 19 to 64 working 100 hours per month earning up to 99 percent of the federal poverty level (FPL). Those making between 100 and 138 percent of the FPL would be covered through the federally administered Marketplace program. Full time students, individuals in workforce training programs, parents and caregivers, as well as individuals with disabilities are exempt from the work requirement. Gov. Tate Reeves has stated he would veto any Medicaid expansion bill, and legislators would need to have a veto-proof majority to overcome his opposition. Read More
Missouri
Missouri House Approves Bill Restricts Medicaid Payment for Certain Organizations. St. Louis Post-Dispatch reported on April 24, 2024, that the Missouri House has advanced a bill which would prohibit Medicaid from paying for health care services from any organization that affiliates with abortion providers, including Planned Parenthood. The bill now moves to Governor Mike Parson for signature. Read More
Montana
Montana Medicaid Director Resigns. The Montana Free Press reported on April 25, 2024, that Montana Medicaid Director Mike Randol has resigned after accepting a job in the private sector. Randol’s last day will be May 10. Rebecca de Camara, the current administrator of the Behavioral Health and Developmental Disabilities Division, was appointed as acting Medicaid director beginning May 13. Read More
New York
New York City’s Fiscal 2025 Executive Budget Sparks Concern Over Mental Health Services Funding. Crain’s New York reported on April 25, 2024, that New York City Mayor Eric Adams released an executive budget for fiscal 2025 with more than $5 billion allotted for healthcare initiatives, up $172 million from the preliminary budget. The New York City Council’s Committee on Health has expressed concern about a lack of additional funding to support preventive mental healthcare. The council and the mayor must reach a final budget by July. Read More
North Carolina
North Carolina Governor’s Budget Proposes More Medicaid Funding for IDD, Elderly Population. North Carolina Health News reported on April 25, 2024, that North Carolina Governor Roy Cooper’s $34.5 billion fiscal 2025 budget seeks to improve care for people with disabilities, increase Medicaid payment rates for providers, and support elderly beneficiaries. Specifically, Cooper suggests setting aside funds to establish a Medicaid program that would offer additional home-based care options for individuals with disabilities as well as $445 million to increase pay rates for direct support caregivers. The budget also allots $17.5 million to add 1,000 slots for the Innovations Waiver program, which offers additional home and community-based services for individuals with disabilities and currently has a waitlist of 16,000 individuals. The proposal calls for $265 million to increase Medicaid reimbursement for physicians, dentists and specialists as well as $10.5 million to prevent the institutionalization of elderly residents. Read More
Oregon
Oregon Plans to Implement New CCO Contracts in 2027; Eliminate Health Disparities by 2030. The Oregon Capital Chronicle reported on April 24, 2024, that a state forum was held to address eliminating health inequities in Oregon, including through upcoming coordinated care organization (CCO) contracts that will be implemented in 2027. New contract modifications will include changes to how providers and insurers invest in the regions they serve and how individuals will be administered other services that improve their overall health, including housing assistance. The Oregon Health Authority has set a goal to eliminate health inequities by 2030, and will release a strategic plan in June mapping a plan of how federal and state Medicaid dollars will be used to support the initiative. Read More
Oregon Medicaid Program Offers Equipment to Protect Beneficiaries Against Climate Change. CBS News reported on April 29, 2024, that Oregon Medicaid is providing beneficiaries with equipment aimed at offering protection against climate-related events, such as air conditioners, air purifiers, power banks, and mini fridges. The state initially began sending equipment to Medicaid recipients in March and is the first in the country to utilize Medicaid funding to address climate change. The funding is part of Oregon’s five-year, $1.1 billion effort to address health-related social needs. Read More
National
Medicaid, Medicare Enrollment Tops 151 Million in January 2024, CMS Reports. The Centers for Medicare & Medicaid Services announced on May 1, 2024, that Medicaid and Children’s Health Insurance Program enrollment was approximately 84 million in January 2024, a 1.2 percent decrease from December 2023. Medicare enrollment was nearly 67 million, a 0.2 percent increase. More than 12 million individuals were eligible for both Medicare and Medicaid. Read More
FTC Finalizes Rule to Prevent Digital Health Apps from Releasing Sensitive Medical Data. Fierce Healthcare reported on April 26, 2024, that the Federal Trade Commission (FTC) finalized a rule aimed at preventing digital health apps from sharing consumers’ sensitive medical data with companies. The rule also requires vendors managing health records and health apps to notify individuals, the FTC, and potentially the media in the event of a breach of personally identifiable health data. The final rule will go into effect 60 days after its publication in the Federal Register. Read More
Federal Court Dismisses Medicare Home Health Payment Lawsuit. Modern Healthcare reported on April 29, 2024, that the U.S. District Court of Columbia dismissed a lawsuit filed by the National Association for Home Care and Hospice (NAHCH) against the U.S. Health and Human Services Department (HHS) and the Centers for Medicare & Medicaid Services (CMS) regarding Medicare home healthcare payment calculations. The Court ruled that NACHC had not fully exhausted the administrative options to address the association’s concerns prior to filing the lawsuit. NACHC plans to continue to challenge the payment methodology. Read More
CMS, NCQA Grant Two Week Extension for Insurers to Submit Star Quality Data. Modern Healthcare reported on April 29, 2024, that the Centers for Medicare & Medicaid Services (CMS) and the National Committee for Quality Assurance (NCQA) will provide insurers additional time to submit quality data due to the cyberattack on Change Healthcare. Health plans will now have until June 28 to submit data that will be used to calculate five-star ratings. CMS and NCQA did not indicate if the extension will also delay the release of the star quality ratings this year. Read More
Industry News
CVS to Acquire Medicare Advantage Broker Hella Health. Modern Healthcare reported on April 30, 2024, CVS Health has acquired New York-based Hella Health, a Medicare Advantage (MA) broker which offers plans from Aetna, Cigna, Humana, UnitedHealthcare and other major insurers. Financial terms were not disclosed. Read More
Your Behavioral Health Acquires Insight Treatment Programs. Comvest Partners announced on April 30, 2024, that its portfolio company, Your Behavioral Health, has acquired Insight Treatment Programs, a provider of teen mental health and addiction treatment programs. Your Behavioral Health now provides clinical inpatient and outpatient mental health care across more than 25 sites throughout Southern California. Read More
CareSource Names Fred A. Schulz Chief Operating Officer. CareSource announced on April 24, 2024, that it has named Fred A. Schultz as chief operating officer. Schultz will report to CareSource President and chief executive Erhardt Preitauer. Schultz has formerly worked at Accenture, Aetna, CatalystRx, UnitedHealth Group, and WellCare Health Plans. Read More
Centene Updates Prior Authorization System to Include Automating Source Data. Modern Healthcare reported on April 26, 2024, that Centene has updated its prior authorization system by automating real-time source data in an effort to streamline pre-approval decisions for patients and providers. The update follows a recent Centers for Medicare & Medicaid Services rule that requires Medicare, Medicaid, and Marketplace plan carriers to improve the efficiency and transparency of prior authorization decisions. Read More
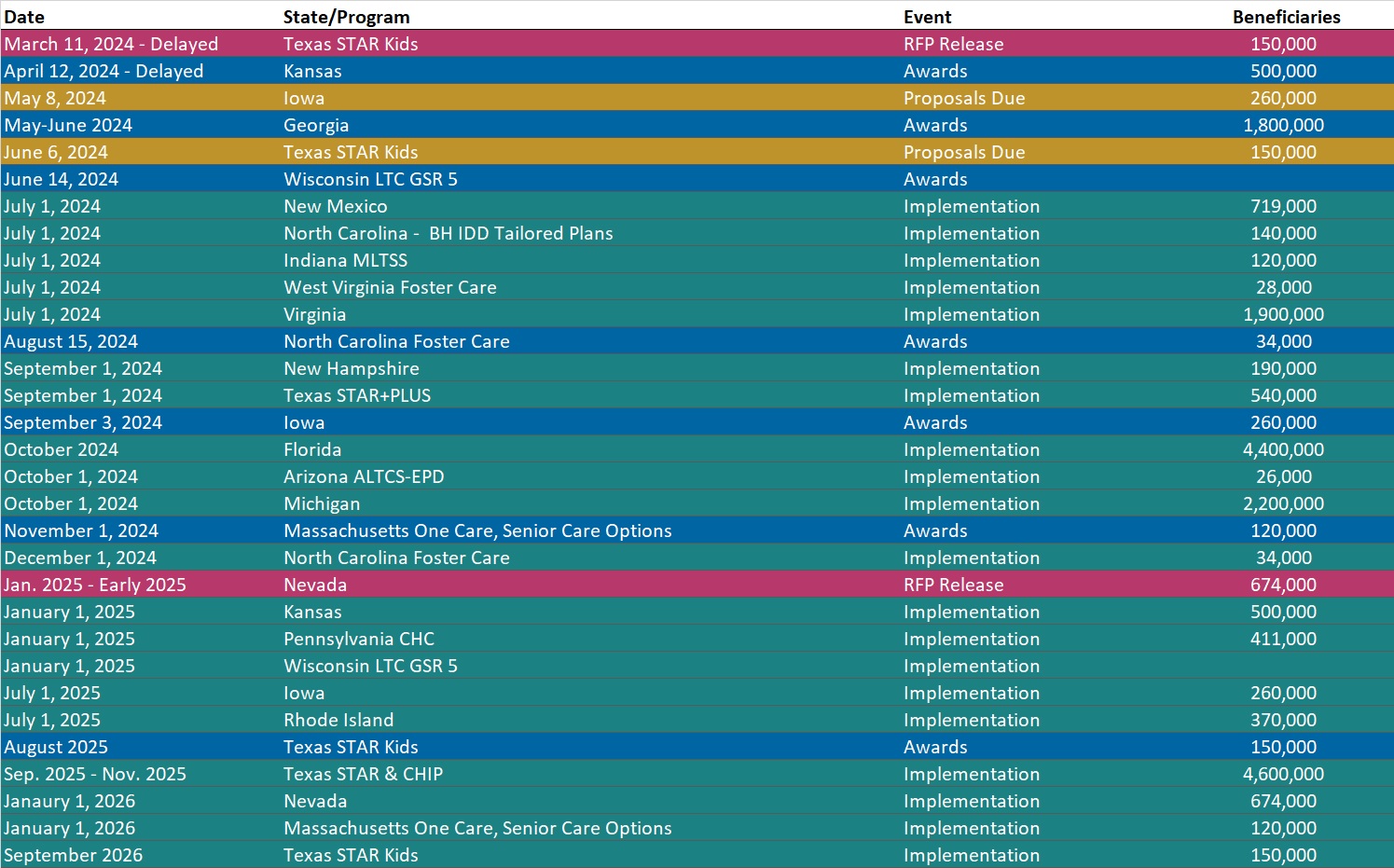
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Illinois Medicaid Managed Care Enrollment is Down 0.5%, Jan-24 Data
- Illinois Dual Demo Enrollment is Down 6.3%, Jan-24 Data
- Iowa Medicaid Managed Care Enrollment is Down 17%, 2023 Data
- South Dakota Medicaid Enrollment is Up 3.2%, FY 2023 Data
- Virginia Medicaid Managed Care Enrollment is Flat, Jan-24 Data
- Virginia Medicaid MLTSS Enrollment is Flat, Jan-24 Data
- West Virginia Medicaid Managed Care Enrollment is Down 6.4%, Apr-24 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Iowa Pharmacy Benefit Administration RFP, Apr-24
- Maryland Preferred Drug List and Supplemental Rebate For Medicaid FFS RFP, Apr-24
- Pennsylvania Community HealthChoices RFA Q&A, 2024
Medicaid Program Reports, Data, and Updates:
- Federal Regulatory Tracker
- Updated Georgia Overview
- Iowa PHE Medicaid Redeterminations Monthly Report to CMS, Mar-24
- Washington Medicaid Managed Care Service Area Matrices, 2020-24
- Washington Value-Based Payment Quality Report Cards, 2021-23
- West Virginia Children’s Health Insurance Program (CHIP) Annual Reports, 2018-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
