This week's roundup:
- In Focus: CMS Seeks Input on the Future of Digital Health: What the Health Technology Ecosystem RFI Means for Stakeholders
- In Focus: CMS Announces New Innovation Agenda: Here’s What You Need to Know
- In Focus: Transforming Crisis Care Intervention: The Role of 988
- Indiana Extends Hoosier Care Connect Contracts Through June 2028
- Iowa Legislature Approves Medicaid Work Requirements Bill
- New York Submits Section 1115 Demonstration Amendment to Launch Medicaid Buy-In Program
- Oregon Releases PACE RFP
- House Budget Committee Advances Budget Bill with Changes
- HHS Implements AI Strategy to Improve Efficiency Across Health Programs
- Head of Aetna Medicaid Operations Steps Down
- Actuaries Corner: Stopping a ‘Moral Obscenity’: Senate Judiciary Committee Expresses Support for PBM Reform
In Focus
CMS Seeks Input on the Future of Digital Health: What the Health Technology Ecosystem RFI Means for Stakeholders
This week, in our In Focus section, health IT experts at Leavitt Partners, an HMA Company, review the recently released Request for Information (RFI) from the Centers for Medicare & Medicaid Services (CMS) and the Assistant Secretary for Technology Policy/Office of the National Coordinator for Health (ASTP/ONC), titled Health Technology Ecosystem (CMS-0042-NC). The RFI, published May 16, 2025, signals a renewed federal focus on advancing digital health tools, improving data interoperability, and supporting patient-centered innovation.
Notably, this RFI aligns with the vision laid out in Leavitt Partners’ Kill the Clipboard policy blueprint, developed in collaboration with a broad coalition of healthcare stakeholders. The paper outlines a future in which patients and providers benefit from seamless digital experiences, real-time data exchange, and reduced administrative burden. The RFI reflects many of the same priorities—such as expanding FHIR® Application Programming Interfaces (APIs), improving provider directories, and promoting digital identity solutions—that were highlighted in the paper as essential to modernizing the healthcare system.
Why This RFI Matters
The RFI invites public input on how CMS and ASTP/ONC can strengthen the digital health ecosystem for Medicare beneficiaries. It builds on years of federal investment in interoperability. The agencies are now seeking feedback on how to reduce barriers to data access, promote innovation in digital health products, and align technology with value-based care goals.
This is a pivotal opportunity for stakeholders to shape the future of digital health policy—especially as CMS continues to explore how APIs, digital identity, and patient-facing tools can improve care delivery and outcomes.
Key Themes in the RFI
The RFI is broad in scope, but several themes stand out, including:
- Addressing Patient and Caregiver Needs: The RFI asks patients which digital tools would be most helpful to them and their caregivers in managing their health needs, navigating care, and accessing all relevant health information in one place. It asks what features are most needed, what is missing from current apps, and how CMS can support adoption, especially for Medicare beneficiaries with limited digital experience. CMS is exploring how to make more data—beyond claims and clinical data—available through APIs. It also explores the role that CMS should play in reviewing and measuring the real-world impact of these tools on outcomes and costs. They also are considering how to promote the use of secure, standardized digital identity credentials (e.g., Login.gov, ID.me) to streamline patient access. Feedback also is sought on how TEFCA, FHIR APIs, and health information exchanges (HIEs) can better support seamless data exchange.
- Provider Adoption of Digital Health Tools: CMS is exploring how to help providers, especially those in rural areas, adopt digital health tools by addressing barriers like workflow integration, data access, and interoperability. CMS is also looking to improve administrative functions like scheduling and intake through third-party apps. In addition, CMS is seeking to understand which FHIR APIs and capabilities are already being supported or utilized in provider systems. They are also interested in understanding how providers might accept standardized digital identity credentials from patients and any challenges that might inhibit its adoption. ASTP/ONC is also seeking information on revisions to the information blocking requirements.
- Engaging Payers: The RFI invites payers to share how they can support interoperability and digital innovation, including through the use of APIs, digital identity credentials, and real-time access to clinical quality data. CMS is also interested in how payers can reduce provider burden, support value-based care (VBC), and contribute to a more connected digital health infrastructure. Feedback is requested on TEFCA participation, payer-to-payer data exchange, and the potential for a nationwide provider directory.
- Advancing VBC Organizations: The RFI emphasizes the role of digital health in supporting alternative payment models (APMs) and accountable care organizations. CMS is seeking feedback on which digital capabilities are most essential for success in VBC—such as care coordination, quality measurement, and patient engagement—and how certification criteria and data standards can better align with these needs. The agencies are also exploring how to reduce complexity for APM participants while maintaining flexibility and data access.
- Enabling Technology Vendors, Data Providers, and Networks: The RFI requests feedback from developers, data aggregators, and HIEs on how to unlock innovation through better access to CMS data, improved API standards, and streamlined certification processes. The RFI asks which technical and policy changes would enable more effective digital health products, recommendations to improve interoperability across networks, and means of supporting the viability of data exchange infrastructure.
Implications for Stakeholders
This RFI is more than a technical exercise; it is a strategic signal. The Trump Administration is maintaining momentum behind VBC and digital transformation. Stakeholders should consider:
- Submitting comments to CMS by the June 16, 2025, deadline.
- Assessing internal readiness to adopt or develop digital tools that align with CMS’s vision.
- Engaging in policy discussions regarding digital identity, data standards, and patient access.
- Monitoring related RFIs, including the Food and Drug Administration RFI exploring the potential use of HL7 FHIR standards to support the submission of study data derived from real-world data sources—such as electronic health records, claims, and registries—for regulatory purposes.
Next Steps
Health Management Associates, Inc. (HMA), encourages healthcare organizations to review the RFI and consider how their experiences, innovations, and challenges can inform CMS’s next steps. This is a rare opportunity to influence the infrastructure that will shape digital healthcare for years to come.
For support in drafting comments or understanding how this RFI intersects with your organization’s strategy, contact our Leavitt Partners health IT experts, Ryan Howells ([email protected]) or David Lee ([email protected]).
CMS Announces New Innovation Agenda: Here’s What You Need to Know
On May 13, 2025, the Centers for Medicare & Medicaid Services (CMS) published its new strategic direction for the CMS Innovation Center. The strategy builds on the lessons of the first 15 years of the Innovation Center, while presenting a significant pivot in policy direction, which emphasizes evidence-based prevention, consumer engagement, and tech-enabled care, while prioritizing financial performance over broad participation.
The new strategy provides high-level direction on the Trump Administration’s vision for the next phase of value-based payment reform under the leadership of CMS Administrator Dr. Mehmet Oz and Innovation Center Director Abe Sutton. They intend to “double down on our commitment to value-based care and take the learnings from the[se] previous investments to build a health system that empowers people to drive and achieve their health goals and Make America Healthy Again.” Notably, the strategy also aligns with goals central to the Trump Administration’s Make America Healthy Again initiative.
This new direction affirms the administration’s commitment to continue advancing value-based care and opens additional opportunities for organizations seeking to enhance the delivery of services that drive positive outcomes. Health Management Associates (HMA), experts will be tracking the implementation of the Innovation Center’s new strategy, including expected forthcoming models, movement toward greater levels of downside risk, and changes to existing models to align with the administration’s priorities. In this article, our experts review the strategy and provide insights on key takeaways for stakeholders.
New Strategy Overview
CMS leaders view the Innovation Center agenda as a framework for accelerating healthy behaviors, leveraging the agency’s authority to test new approaches designed to incentivize and engage stakeholders. According to CMS officials, the Innovation Center “will work expeditiously toward the future of health—building a system in which people are empowered to achieve their health goals and providers are incentivized to compete to deliver high-quality, efficient care and improve the health outcomes of their patients.”
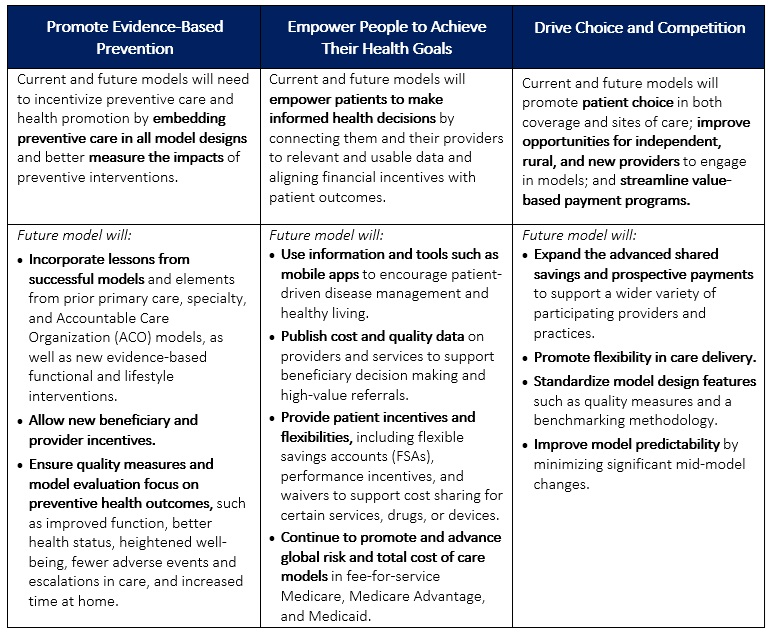
The strategy has three interrelated, foundational pillars:
- Promoting evidence-based prevention
- Empowering people to achieve their health goals
- Driving choice and competition.
Table 1 provides more detail on each pillar.
In addition to the new agenda, CMS released a request for information (RFI) seeking industry input on strategies that can better leverage data and technology to empower consumers. The focus of the RFI aligns with the Innovation Center’s strategic pillars to use tools, information, and processes that better connect people to their health data and allow them to make informed health decisions alongside their providers.
Table 1. CMMI’s Interrelated Strategic Pillars
Takeaways and Considerations
Critical to CMS’s approach is the belief that empowering individuals to make their health decisions—through incentives, better data access, and more flexible options—can lead to better health outcomes and lower overall costs. This shift reflects an evolution in healthcare policy that places greater emphasis on personal accountability and private sector collaboration—a key theme that is emerging across the administration’s policy initiatives.
Consumer Engagement. One of the most notable aspects of the new Innovation Center strategy is the promotion of consumer engagement; it places more focus on direct consumer engagement through education and incentives compared with earlier initiatives. This is one area in which the Innovation Center plans to collaborate with the private sector to develop consumer-facing tools (e.g., mobile apps, nudges toward healthy behaviors, etc.).
The focus on consumer engagement also presents opportunities for organizations to enhance their customer experience. By understanding the needs and preferences of their patients, organizations can tailor their services and care models to better meet those demands. This personalized approach not only improves patient satisfaction, but also drives continuity of care, ultimately contributing to long-term improvements in health.
Data and Technology. The new strategy also emphasizes the importance of data, indicating intentions to better equip organizations that participate in the model with data that can inform decisions and optimize their processes. CMS officials are examining policies and collaborations that will empower private sector organizations, including model participants, researchers, and technology vendors, to develop innovative data-driven solutions to drive efficiencies and improved health.
To that end, the May 16, 2025, Request for Information (RFI) from CMS and the Assistant Secretary for Technology Policy/Office of the National Coordinator for Health (ASTP/ONC), Health Technology Ecosystem (CMS-0042-NC), focuses on Medicare beneficiaries’ use of technology to improve health outcomes. The RFI, which HMA experts analyze here, underscores the administration’s intentions of taking “bold steps to modernize the nation’s digital health ecosystem.”
Medicare Advantage. The Innovation Center’s new strategy indicates that stakeholders should expect more models that address Medicare Advantage (MA). The agency stated that “features of a model could include testing changes to payment for MA plans, such as testing the impact of inferred risk scores, regional benchmarks, or changes to quality measures that better align with promoting health.” Additionally, the strategy references a forthcoming specialty-focused longitudinal care model within MA and Medicaid, signaling intentions to drive multi-payer alignment.
Saving Federal Tax Dollars. Another major aspect of the strategy is “protecting federal taxpayers.” This goal reflects a continued emphasis on total cost of care accountability and indicates a more aggressive shift to downside risk. The Innovation Center says it will “require all models to have downside financial risk and require providers to assume some of the financial risk..” Additional provisions of protecting tax dollars include reducing role of state governments in rate setting, simplifying model benchmark methodology, and ensuring “proper and nondiscriminatory provision of funds for health care services.”
What to Watch
For healthcare organizations, the Innovation Center’s agenda signals a need to prioritize consumer-centric models. Hospitals, providers, and insurers should anticipate the following:
- Increased focus on preventive care initiatives to align with new model designs
- More robust data-sharing and technology requirements, meaning investments in patient-focused digital tools will become essential
- New opportunities in MA, given potential payment model innovations affecting plan structures and risk-adjusted reimbursement
Healthcare stakeholders should monitor possible developments related to the strategy.
- While details on specific strategies have yet to emerge, the Innovation Center indicated it plans to provide more information on new models, as well as changes to existing models, in the coming months.
- The Innovation Center has not provided a goal akin to the previous administration’s effort to have 100 percent of Medicare beneficiaries in accountable care relationships by 2030. It is still unknown whether these goals are forthcoming or if this will remain vague.
- Stakeholders are still awaiting clarity on changes to existing models, including key models set to conclude at the end of 2026 (i.e., ACO REACH and Kidney Care Choices).
- Strategy language indicates that the agency may develop payment innovation in prescription drugs, medical devices, and technology.
Connect With Us
The Health Management Associates Annual Conference, Adapting for Success in a Changing Healthcare Landscape, October 14-16, 2025, in New Orleans, LA, will feature discussions on how the new strategy is reshaping the healthcare system and care delivery for patients, particularly the opportunities to revisit provider contracts with MA plans and to integrate technology to advance the prevention of chronic conditions and achieve population health goals.
For more information about the opportunities and considerations the Innovation Center agenda presents for your organization, contact HMA’s featured experts, including Amy Bassano or Kate de Lisle.
Transforming Crisis Care Intervention: The Role of 988
This week, our third In Focus section highlights the national 988 Suicide and Crisis Lifeline, the three-digit number for individuals in need of behavioral health crisis support. The 988 Lifeline is composed of 200-plus contact centers across the country, which connect people to trained counselors to deescalate crises, provide behavioral health resources, or connect individuals to an in-person responder. Supported by federal legislation to help create a nationwide, standardized, easy to remember 3-digit number, the program is still in its early stages, having been established three years ago this coming July.
In this article, Health Management Associates (HMA) experts provide important context about the 988 Lifeline and future policy direction and suggests actions state leaders can take to enhance use of this critical resource.
988 Lifeline: A Product of Coordinated Collaboration
The story of how the 988 Lifeline was created is an example of long-term advocacy and innovation that demonstrates how a solution needs to combine the state and local decisionmakers with federal policy and support. People experiencing a mental health crisis, thoughts of suicide, or concerns about substance misuse should receive the appropriate local response to seek support or care.
Prior to the 988 Lifeline, individuals experiencing a behavioral health crisis may have contacted 911 and, therefore, not always received the most appropriate response for their unique needs. In some situations, 911 responders—typically law enforcement, emergency medical services, or hospital emergency departments—are ill-equipped to direct people experiencing a behavioral health crisis. Trained behavioral health professionals responding to an individual experiencing a crisis is the appropriate intervention at most points of access. Increased diversion from 911 calls to 988 when an individual is experiencing a behavioral health crisis is an expected long-term outcome.
The federal government’s role is to continue to support the work to enhance the 988 Lifeline, but there’s so much more that needs to happen to increase education and awareness in states, localities, and Tribal nations. They still need support in building out their systems.
State Initiatives Strengthening the 988 Lifeline
Since the launch of the 988 Lifeline in July 2022, 50 percent of the states have approved some type of appropriation or some type of legislation to further cement 988 in their local communities. Some states have established trust funds or implemented 988 cell phone fees similar to what 911 does to provide financial support. Other states have established committees to study and support 988 implementation, building out the various components of a true coordinated crisis system of care.
HMA experts have identified strategic and operational recommendations to support this ongoing work, including:
- Be intentional about having the right people at the table where decisions are made, including voices with lived experience and people who are part of the policy-making process. Establishing this formal, standardized 988 system enables local communities to better allocate resources in crisis situations. In most cases, the contact with the 988 Lifeline is the best intervention to ensure people get the support or resources needed to resolve or deescalate the crisis.
- When designing a crisis system in a community, think about prevention and what happens when the crisis is over. Crisis systems established on a poor behavioral health foundation will fail. Stakeholders and decisionmakers should continue building out their systems by remembering that the entire continuum of care—from crisis to ongoing support—is needed.
- Identify the data that are needed to tell the story about the value of the 988 Lifeline and crisis care systems. Anecdotes are essential and should be paired with data, especially when ongoing funding is needed.
Where Is the 988 Lifeline Headed?
It is likely to take decades to generate greater awareness about the 988 Lifeline, to have interoperability between 911/988, to ensure every person in the country has access to the service no matter their zip code, and to see a fully transformed behavioral health crisis system will take decades to accomplish. The collaboration between federal, state, territories, Tribal nations, and local communities is pivotal to reaching these goals.
While we are at the beginning phases of this work, much has been done that should be celebrated. The 988 Lifeline has transformed how we as a nation talk about behavioral health and suicide prevention. Still, we as a collective have work ahead to achieve the vision of transforming the behavioral health crisis care system.
Connect with Us
Health Management Associates (HMA) is hosting a live, interactive event on Thursday, May 29, 2025. [The Ask the Experts: Behavioral Health Town Hall https://www.healthmanagement.com/insights/webinars/ask-hma-experts-behavioral-health-town-hall/ ] will explore the latest developments in behavioral health—from policy shifts and funding trends to real-world solutions for service delivery, workforce challenges, and system design. HMA and Leavitt Partners, an HMA Company, experts will be on hand to answer participant questions and share insights about 988 and other topics:
- Policy and funding updates at the federal level
- Innovative approaches to crisis response, 988 implementation, and substance use services
- Revenue cycle improvements and evolving payment models
- Strategies to strengthen the workforce, integrate care, and leverage digital mental health tools
For more information about 988 systems and effective practices emerging in crisis care, contact Monica Johnson, Managing Director for Behavioral Health. Prior to joining HMA, Ms. Johnson, Managing Director for Behavioral Health, was the director of the 988 & Behavioral Health Crisis Coordinating Office at the Substance Abuse and Mental Health Services Administration—the federal agency that leads public health efforts to advance the behavioral health of the nation.
HMA Roundup
Indiana
Indiana Extends Hoosier Care Connect Contracts Through June 2028. The Indiana Department of Administration announced that the Indiana Family and Social Services Administration, Office of Medicaid Policy and Planning (OMPP) intends to extend its contracts with Anthem Blue Cross and Blue Shield, Centene/Managed Health Services, and UnitedHealthcare serving the Hoosier Care Connect Program through June 30, 2028. OMPP intends to align its HCC procurement with the PathWays for Aging program and competitively re-procure the two contracts under a single solicitation. The PathWays for Aging contracts with Anthem, Humana/Arcadian Health Plan, and UnitedHealthcare are also set to expire June 30, 2028.
Iowa
Iowa Legislature Approves Medicaid Work Requirements Bill. Des Moines Register reported on May 14, 2025, that the Iowa Legislature has passed a bill requiring adults in the Iowa Health and Wellness Plan, the state’s Medicaid expansion program, to work at least 80 hours per month, enroll in job training or education, or earn the equivalent of minimum wage to maintain Medicaid coverage. The Legislative Services Agency estimates up to 32,000 people could lose coverage, with projected state savings of $14.4 million by 2027. The bill now awaits Governor Kim Reynolds’ signature.
New York
New York Submits Section 1115 Demonstration Amendment to Launch Medicaid Buy-In Program. The Centers for Medicare & Medicaid Services announced on May 20, 2025, that New York has submitted an amendment request to modify its Section 1115 Medicaid Redesign Team Demonstration. The request seeks to authorize a new Medicaid Buy-In Program for Working People with Disabilities (MBI-WPD) under the existing demonstration, aimed at expanding Medicaid eligibility for working individuals with disabilities. The amendment also proposes changes to the Special Terms and Conditions (STCs) for the Career Pathways Training (CPT) Program, increasing the maximum allowable days for backfill payments from two to five days per week to support more intensive training schedules. Public comments will be accepted through June 19, 2025.
Oregon
Oregon Releases PACE RFP. The Oregon Department of Human Services Office of Aging and People with Disabilities released on May 14, 2025, a request for proposals (RFPs) seeking organizations to be new providers for the Program of All-Inclusive Care for the Elderly (PACE) in Jackson and Josephine areas that are not currently being served by an active PACE organization. Proposals are due June 17, 2025. ODHS plans to release a notice of intent to award one or more organizations by July 23, 2025.
National
House Budget Committee Advances Budget Bill with Changes. Health Payer Specialist reported on May 19, 2025, that the House Budget Committee advanced a budget bill which cuts Medicaid spending over ten years. Key provisions include work requirements for childless adults, an end to Medicaid managed care organization taxes, penalties for states covering undocumented immigrants, and a restriction on Medicaid reimbursements to Planned Parenthood. Changes in the newest version include imposing Medicaid work requirements more quickly, which were due to take effect in 2029. The bill is expected to move to the House floor by the end of the week. As lawmakers consider cuts to Medicaid, a study by the National Bureau of Economic Research found that Medicaid expansion has saved more than 27,000 lives since 2010, with Medicaid expansion enrollees 21 percent less likely to die during a given year than those not enrolled.
HHS Implements AI Strategy to Improve Efficiency Across Health Programs. Politico reported on May 15, 2025, that Health Secretary Robert F. Kennedy Jr. told the House Appropriations Committee that the Department of Health and Human Services (HHS) is actively implementing artificial intelligence (AI) to improve efficiency in health care programs. He stated that AI is already being used to manage health data and that the department is hiring experts from firms like Palantir and Booz Allen Hamilton to support this transformation. Kennedy emphasized plans to use AI to reform Phase III clinical trials, citing their high cost and long timelines.
Industry News
Head of Aetna Medicaid Operations Steps Down. Health Payer Specialist reported on May 20, 2025, that Jane Brown, head of Medicaid operations at Aetna, is leaving CVS Health to join Gainwell Technologies. Brown has led Aetna’s Medicaid operations since November 2024, and previously spent two years as Aetna’s Kansas plan president and chief executive.
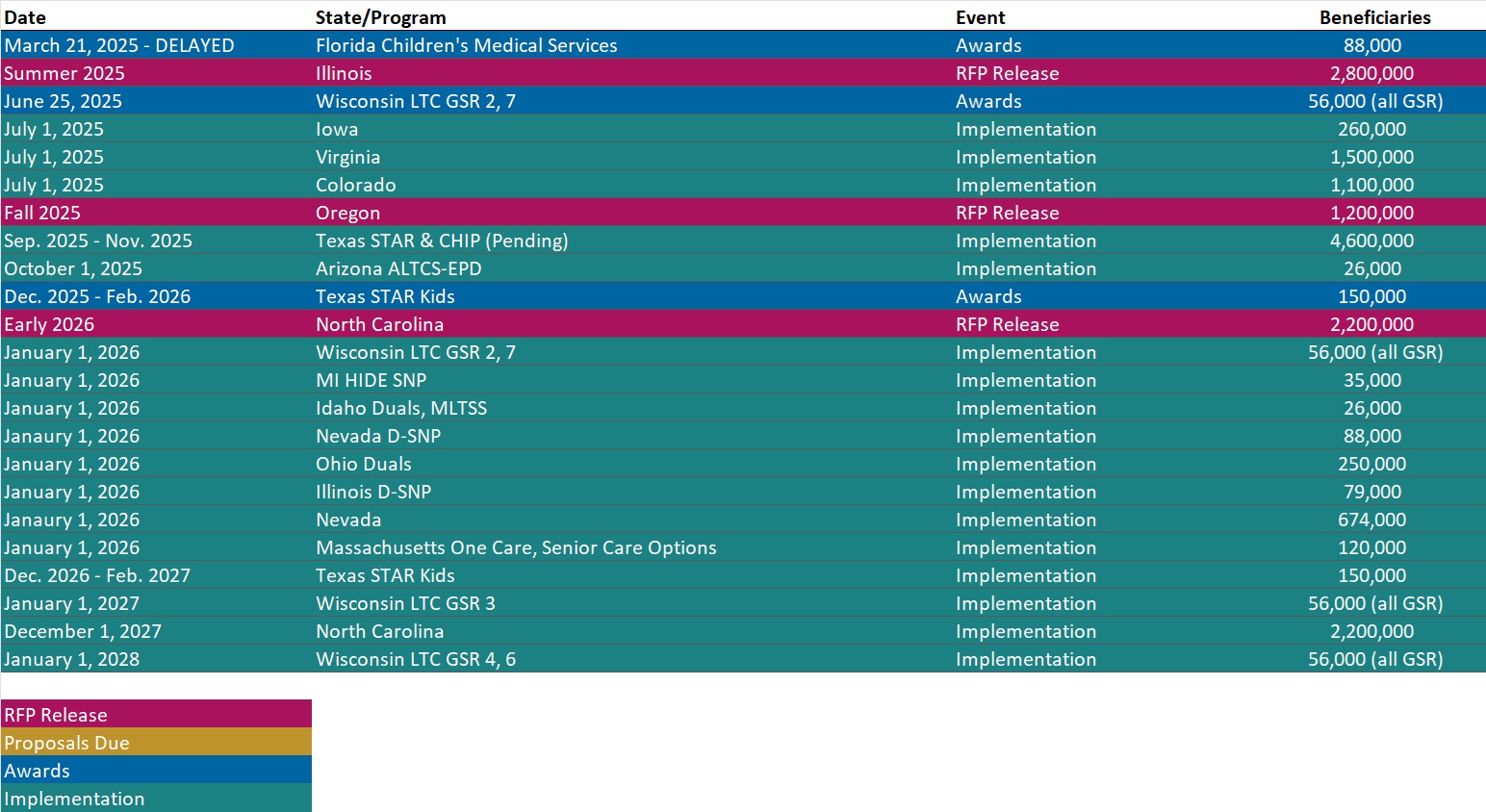
RFP Calendar
Actuaries Corner
Stopping a ‘Moral Obscenity’: Senate Judiciary Committee Expresses Support for PBM Reform. Sen. Chuck Grassley, R-Iowa, suggested Congress could once again move to overhaul PBMs’ controversial business practices after it passes President Donald Trump’s conservative megabill this summer.
Discover other developments in the Wakely Wire here.
Company Announcements
MCG White Paper:
The hospital-at-home model of care has extended beyond the pandemic allowing healthcare organizations to manage inpatient care in the home. In this exclusive downloadable white paper from MCG Health, Senior Physician Editor, Jennifer N. Goldstein, MD MSc, and Associate VP & Managing Editor, Bill Rifkin, MD, FACP, discuss the evolution, challenges, and future directions of the hospital-at-home (HaH) model of care. Download it here.
HMA News & Events
HMA Conference
Register Today for the HMA 2025 Conference. October 15, 2025 • 8:30 AM.
The healthcare landscape is transforming before our eyes, from federal budget negotiations to major policy shifts in Medicaid, Medicare, and digital health. The HMA Conference is your chance to engage with the experts shaping what comes next.
Recent actions by Congress and the Administration—including new proposals related to eligibility, cost-sharing, drug pricing, and value-based care—signal significant movement in how care is delivered and paid for across the country. These changes impact all stakeholders, across diverse perspectives and regions.
At the HMA Conference, you’ll gain insight directly from the people driving these developments—federal policy experts, agency insiders, and healthcare leaders who will be speaking, facilitating, and in attendance.
What to Expect at the HMA Conference:
- Expert-led sessions on Medicaid, Medicare & Marketplace innovations
- Updates and analysis on federal legislation and regulatory priorities
- Practical strategies for navigating uncertainty and planning ahead
- Connections with cross-sector leaders from around the country
Register Early & Save
Early bird rates are available through July 31, 2025.
We can’t wait to welcome you to New Orleans this October and continue the important work of shaping the future of healthcare—together.
HMA Webinars
Ask HMA Experts: Behavioral Health Town Hall. Thursday, May 29, 2025, 12 PM ET. Join us for a dynamic and interactive Behavioral Health Town Hall hosted by Health Management Associates (HMA). Our experts will be available to answer your questions live on a wide range of critical topics, including:
- Federal policy, personnel, and funding changes;
- Emerging strategies for addressing social determinants of health, substance use disorder and crisis coordination (including 988);
- Behavioral health revenue cycle management and alternative payment models; and
- Innovations in addressing workforce shortages, integrated service delivery, digital mental health tools, and best practices for community mental health service delivery.
Whether you’re navigating regulations, searching for new funding, designing service delivery systems, or just trying to understand what happens next, this town hall is your chance to ask questions, share insights, and discuss real-world solutions with industry experts.
Wakely Webinars
Medicare Final Notice – PACE Focused Summary. Thursday, May 22, 2025, 1 PM ET. PACE plans have some big changes on the horizon with the release of the Final Notice on April 7th. CMS has proposed and finalized changing the risk score model (how they calculate Medicare reimbursement for PACE) from version 22 to version 28. This model change will be fully in place by 2029.
Leavitt Partners Case Studies
Creating Value in Business: Alliance Building at the One Intermountain Breast Care Center. Most large organizations are built through a complex series of acquisitions and expansions over years or decades, often outpacing the organization’s ability to integrate its systems, resulting in a patchwork approach. Additionally, system optimization is often siloed within departments due to limited insight, time, competing demands, or all three. In today’s environment, streamlining internal operations is essential, particularly in the health sector, but doing so requires a delicate balancing of interests, motivations, and personalities across the organization.
The below case study from the Leavitt Center for Alliances, an HMA Initiative, describes how a convener brought together medical practitioners and staff at the One Intermountain Breast Care Center to update technology, establish universal, agreed upon best practices, and reorder procedures to improve care.
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Medicaid Market Overviews, Reports, and Data
- Updated Medicaid Managed RFP Calendar
- Updated Medicaid NEMT RFP Calendar
- HMA Federal Health Policy Snapshot
- New Medicaid enrollment, RFP documents, and other market intelligence resources for dozens of states.
- Updated Arizona, Indiana, Missouri, and South Dakota Overviews
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services.
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].