HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Kansas Releases KanCare, CHIP Medicaid Managed Care RFP

- In Focus: Georgia Releases Medicaid Managed Care RFP

- Alaska Pauses Procedural Medicaid Disenrollments

- Florida Agencies to Report on Medicaid Redeterminations to State Senate

- CareSource to Partner with Pediatric Care Provider to Bid on Florida Medicaid Contract for Children, Teens with Special Needs

- Illinois Head of Healthcare, Family Services to Step Down

- Indiana Drops Molina from Medicaid MLTSS Contract

- Indiana Medicaid MLTSS Contracts to Begin July 2024

- Indiana Awards Hoosier Rx Program Contracts to Three Companies

- Iowa to Develop HCBS for Children With Severe Behavioral Health Needs in Lawsuit Settlement

- Elevance, Blue Cross Louisiana Withdraw Merger Application

- Louisiana Lawmakers Push to Reexamine Medicaid Technology Contract

- Michigan Releases State Action Plan to Improve Birth Outcomes

- North Carolina Medicaid Expansion to Launch on December 1

- Ohio Estate Recovery Program Recovers Less Than One Percent of Fiscal 2023 Medicaid Costs

- Oklahoma Receives Federal Waiver Approval Enabling Transition to Medicaid Managed Care

- Texas Implements Vendor Contracts for Medicaid FFS Prior Authorization, Enrollment, Other Functions

- CMMI Value-based Models Result in $5.4 Billion Increase in Federal Spending, Report Finds

- Carlyle Group in Talks to Acquire Majority of 2 Medtronic Medical Device Businesses

In Focus
Kansas Releases KanCare, CHIP Medicaid Managed Care RFP
This week, our In Focus section reviews the KanCare Medicaid capitated managed care request for proposals (RFP), released October 2, 2023, by the Kansas Department of Health and Environment and Department for Aging and Disability Services. The program covers approximately 520,000 beneficiaries and is worth $4.1 billion. New contracts would begin January 2025.
KanCare Background
KanCare is the state’s Medicaid managed care program, covering both traditional Medicaid and Children’s Health Insurance Program (CHIP) members. In all, KanCare covers approximately 320,000 children, 79,000 parents and pregnant women, 59,000 individuals with disabilities, and 54,000 individuals ages 65 and older.
Managed care organizations (MCOs) provide statewide integrated physical health, behavioral health, and long-term services and supports. Covered services include nursing facility care and home and community-based services, as well as Medicaid-funded inpatient and outpatient mental health and substance use disorder services and seven Section 1915(c) HCBS waiver programs.
Kansas is not currently an expansion state. While the governor’s 2024 budget plan called for Medicaid expansion, lawmakers rejected the proposal during the last legislative session.
In 2022, the state legislature delayed the procurement until 2023 to ensure that it occurred after the gubernatorial election and extended current MCO contracts through 2024.
RFP
Kansas expects to select three MCOs. The RFP includes a renewed focus on integrated, whole-person care, workforce retention, and accountability measures for the MCOs. The state lists the main goals for the KanCare procurement as:
- Improve member experience and satisfaction
- Improve health outcomes by providing integrated, holistic care with a focus on the impacts of social determinants of health
- Reduce healthcare disparities
- Expand provider network and direct care workforce capacity and skill sets
- Improve provider experience and encourage provider participation in Medicaid
- Increase the use of cost-effective strategies to improve health outcomes and the service delivery system
- Leverage data to promote continuous quality improvement
Timeline
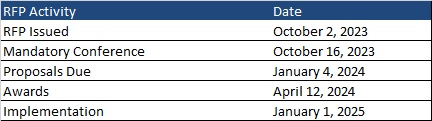
A mandatory pre-bid conference will take place on October 16, 2023. Proposals are due January 4, 2024, with awards expected April 12, 2024. Contracts will be effective January 1, 2025, through December 31, 2027, with up to two one-year renewal options. Following is the timeline leading up to implementation.
Current Market
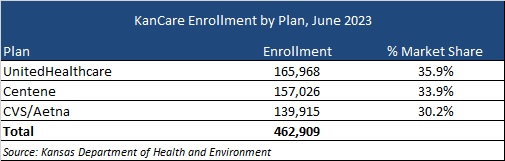
Incumbents are Centene, CVS/Aetna, and UnitedHealthcare. A breakdown of market share by enrollment as of June 2023 can be seen in the table below. Other insurers have already cited their interest in bidding for the new contracts.
Georgia Releases Medicaid Managed Care RFP
This week, our second In Focus section reviews the Medicaid managed care request for proposals (RFP) for the Georgia Families and Families 360° programs, released September 22, 2023, by the Georgia Department of Community Health (DCH). The programs cover approximately 1.8 million beneficiaries and are currently worth $5.7 billion. New contracts will carve in certain aged, blind, and disabled (ABD) populations into managed care, estimated to be worth an additional $3.1 billion.
Georgia Families and Georgia Families 360°
Georgia Families consists of the state’s traditional Medicaid program and the state’s Children’s Health Insurance Program (CHIP), PeachCare for Kids. This includes the new Medicaid expansion program Georgia Pathways to Coverage and the Planning for Healthy Babies (P4HB) program. Georgia Families 360° covers 27,000 children in foster care, adoption assistance, and certain juvenile justice programs.
RFP
Georgia intends to select at three or four care management organizations (CMOs) for Georgia Families. One of the selected CMOs also will be awarded a contract to serve Georgia Families 360°.
Under the procurement, Georgia intends to carve in ABD non-dual and non-home and community-based services population into managed care. In total, the state has approximately 600,000 ABD beneficiaries; however only a subset of the ABD population will be included in the initial phase of the transition. Additional ABD categories are expected to transition in later years.
Timeline
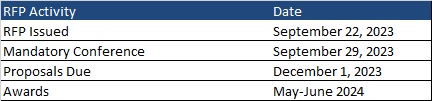
A mandatory bidders conference will take place on September 29. Proposals are due December 1. Awards will be announced in May or June 2024. Contracts will run from the date of award until the end of the state fiscal year, with six one-year optional renewals. The timeline is as follows:
Current Market
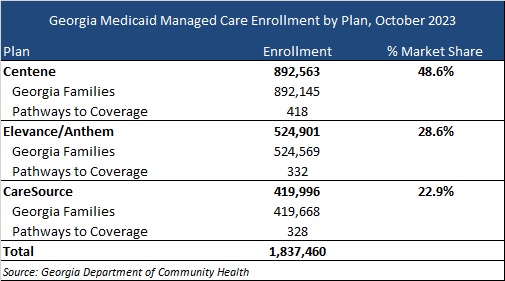
Incumbents are CareSource, Centene/Peach State, and Elevance/Anthem. The following table provides a breakdown of market share by enrollment as of October 2023.
HMA Roundup
Alaska
Alaska Pauses Procedural Medicaid Disenrollments. The Anchorage Daily News reported on October 2, 2023, that the Alaska Division of Public Assistance has temporarily paused procedural Medicaid enrollment terminations after thousands of beneficiaries lost coverage for which they may still be eligible. Additionally, families will have at least an extra 30 days to respond to requests for income verification and other information. Over the last two months, nearly 14,000 beneficiaries were disenrolled for procedural reasons. Read More
Arizona
Arizona Seeks Public Feedback on Plan to Set Applied Behavioral Analysis Provider Rates. The Arizona Health Care Cost Containment System (AHCCCS) announced on September 22, 2023, that it is seeking public feedback on its annual fee schedule rate updates, including a proposal to set fee-for-service (FFS) rates for Applied Behavior Analysis (ABA) services. The set rates would apply to ABA FFS codes currently paid as a percentage of the billed amount. Managed care plans will be able to negotiate their own rates. The public comment period is open through September 30. Read More
Florida
Florida Agencies to Report on Medicaid Redeterminations to State Senate. WMNF reported on October 2, 2023, that the Florida Agency for Health Care Administration, Department of Children and Families, and Florida Healthy Kids will each report on Medicaid eligibility redeterminations to the state Senate Health and Human Services Appropriations Committee on October 11. Between April and August, Florida disenrolled over 500,000 Medicaid beneficiaries. Read More
CareSource to Partner with Pediatric Care Provider to Bid on Medicaid Contract for Children, Teens with Special Needs. Health Payer Specialist reported on September 27, 2023, that CareSource will partner with Florida-based provider chain Spark Pediatrics to bid on a Florida Medicaid managed care contract serving children and teens with special needs and chronic illness. The partnership, named ImagineCare, is through CareSource Florida subsidiary the Columbus Organization. Bids are due October 25. Read More
Illinois
Illinois Head of Healthcare, Family Services to Step Down. Health News Illinois reported on October 4, 2023, that Theresa Eagleson, head of the Illinois Department of Healthcare and Family Services, will step down at the end of this year. Lizzy Whitehorn, who currently serves as first assistant deputy governor for Health and Human Services, will take over on January 1, 2024, pending state Senate confirmation. Read More
Indiana
Indiana Drops Molina from Medicaid MLTSS Contract. Health Payer Specialist reported on October 3, 2023, that Indiana will not award Molina Healthcare a four-year, $3.85 billion Medicaid managed care long term services and supports (MLTSS) contract because the plan will not meet the federal requirement of having a dual eligible special needs plan available in the state by January 2024. The state previously recommended Molina for the program in March 2023. Read More
Medicaid MLTSS Contracts to Begin July 2024. The Indiana Capital Chronicle reported on October 2, 2023, that Indiana Medicaid Managed Care Long Term Services and Supports (MLTSS) contracts will take effect July 1, 2024, after previously being scheduled for January 1. Read More
Indiana Receives CMS Approval for Medicaid Mobile Crisis State Plan Amendment. The Centers for Medicare & Medicaid Services (CMS) approved on September 19, 2023, an Indiana Medicaid state plan amendment, which will allow the state to develop mobile crisis intervention teams to connect eligible individuals to behavioral health providers 24 hours a day. The program is effective July 1, 2023. Read More
Indiana Awards Hoosier Rx Program Contracts to Three Companies. Health Payer Specialist reported on October 4, 2023, that the Indiana Department of Administration awarded contracts to Cigna, CVS Health/SilverScript, and Centene/Wellcare for the state’s Hoosier Rx program, which provides financial assistance to seniors enrolled in Medicare Part D and Medicare Advantage plans. All three companies are incumbents. Read More
Iowa
Iowa to Develop HCBS for Children With Severe Behavioral Health Needs in Lawsuit Settlement. CBS News reported on October 3, 2023, that Iowa’s Department of Health and Human Services will develop home and community-based services (HCBS) for Medicaid eligible children with severe mental and behavioral needs as part of an agreement in a class action lawsuit filed by civil rights groups. The parties have until July 1, 2024, to reach a final settlement, which must include a plan for implementation of services and performance metrics. Read More
Kansas
Kansas Governor Embarks on Medicaid Expansion Tour. JC Post reported on September 21, 2023, that Kansas Governor Laura Kelly has launched a statewide “Healthy Workers, Healthy Economy” tour, aimed at pressuring lawmakers to hold a vote on Medicaid expansion this spring. About 79 percent of Kansans support expansion. Read More
Kentucky
Kentucky Seeks Public Comment On HCBS Waiver Programs. The Kentucky Department of Medicaid Services announced on September 27, 2023, that it is seeking public feedback on a plan to make public health emergency flexibilities permanent for all 1915(c) Home and Community Based Services (HCBS) waiver programs. The public comment period will run through October 27. Read More
Louisiana
Elevance, Blue Cross Louisiana Withdraw Merger Application. Modern Healthcare reported on September 26, 2023, that Elevance Health and Blue Cross Blue Shield of Louisiana withdraw a $2.5 billion merger application from state regulatory consideration in the face of criticism that the deal would increase healthcare costs and stifle competition. The insurers cited a need “to provide more time for key stakeholders to understand the benefits” of the deal. No timeframe was given for refiling the merger application. Read More
Lawmakers Push to Reexamine Medicaid Technology Contract. The New Orleans City Business reported on September 21, 2023, that Louisiana lawmakers are pushing to reevaluate the state’s decision to award Conduent a 10-year, $245 million Medicaid technology contract. Gainwell Technologies, the current contractor, filed a lawsuit stating the bidding process was flawed and has been granted a restraining order delaying the award of the contract until October 27, when an initial court hearing will be held. Read More
Massachusetts
Massachusetts Receives Approval for Community-Based Mobile Crisis Services SPA. The Centers for Medicare & Medicaid Services announced on September 29, 2023, that it has approved the Massachusetts community-based mobile crisis state plan amendment (SPA). The state can now create mobile crisis intervention teams to provide Medicaid crisis services 24/7 to eligible individuals experiencing a behavioral health or substance use crisis. Read More
Michigan
Michigan Releases State Action Plan to Improve Birth Outcomes. The Michigan Department of Health and Human Services (MDHHS) Division of Maternal and Infant Health announced on October 2, 2023, the launch of a four-year program aimed at improving birth outcomes for Michigan families. Priorities include expanded access to reproductive health; full-term, healthy weight babies; infant sleep safety; and mental, behavioral health and well-being. Read More
Michigan Releases Medicaid Rate Increases in Fiscal 2024 Budget. The Michigan Department of Health and Human Services (MDHHS) released on September 29, 2023, proposed and final Medicaid program provider rate updates included in the fiscal 2024 budget. MDHHS rate modifications include hospital rate increases for level I and II designated trauma facilities; 260 percent increase for brain injury services; 7.5 percent for individual professional services; 10 percent for anesthesia professional services; 10 percent for home health services; and 100 percent of Medicare base rates for ground ambulatory services. The public comment period will be open through October 31. If approved, increases are effective for services as of October 1, 2023. Read More
Michigan Allows 17 Additional Mental Health Clinics to Receive Enhanced Medicaid Funding. WLNS reported on September 28, 2023, that 17 additional Michigan mental health clinics will receive enhanced Medicaid for providing crisis services 24/7; services to anyone who requests care for mental health or substance use disorder; outpatient mental health and substance use disorder treatment services; immediate screenings, risk assessments and diagnoses; and care coordination. Read More
Michigan Disenrolls 13,523 Medicaid Beneficiaries Following August Redeterminations. Upper Michigan Source reported on September 21, 2023, that Michigan has disenrolled 13,523 Medicaid beneficiaries during August redeterminations, including 2,336 who lost coverage for procedural reasons. The state renewed coverage for 148,654 beneficiaries. Another 98,109 up for renewal in August have not completed enrollment forms. Read More
Mississippi
Mississippi Medicaid Reimbursement Reforms to Generate $700 Million For State Hospitals. News 12 WJTV reported on September 21, 2023, that Mississippi Governor Tate Reeves announced a series of Medicaid reimbursement reforms that are estimated to generate approximately $700 million for hospitals across the state. The first initiative will provide direct payments to hospitals serving managed Medicaid patients. The second initiative will supplement Medicaid base payment rates for hospitals by reimbursing inpatient and outpatient hospital services in the fee-for-service system up to the Medicare upper payment limit. If approved, both proposals would be effective as of July 1, 2023. Read More
Nebraska
Nebraska Extends Postpartum Medicaid Coverage to 12 Months. KETV reported on September 27, 2023, that Nebraska is expanding postpartum Medicaid coverage to a full year, effective January 1. Read More
New Hampshire
New Hampshire Implements Updated Plan To Support Aging Adults. New Hampshire Public Radio reported on October 2, 2023, that New Hampshire implemented an updated state plan on aging aimed at better supporting older adults, specifically through expanding access to home and community-based services. The plan took effect October 1, and runs through 2027. Read More
New Hampshire Reinstates Medicaid Coverage for 3,176 Beneficiaries. New Hampshire Bulletin reported on September 21, 2023, that New Hampshire has retroactively reinstated Medicaid coverage for 3,176 people, including 1,351 children, in response to updated guidance regarding redeterminations from the Centers for Medicare & Medicaid Services. The guidance is aimed at ensuring that ex parte eligibility reviews are handled properly. The change will also allow nearly 1,200 people who are up for renewal in October to remain covered. Read More
New York
New York Inspector Reports $3.4 Billion in Medicaid Recoveries, Cost Avoidance. Crain’s New York Business reported on October 3, 2023, that the New York Office of the Medicaid Inspector General posted $3.4 billion in recoveries and cost avoidance for the state Medicaid program in 2022, a six percent increase over 2021. Read More
North Carolina
North Carolina Requests 5-Year Extension of Authority to Use Federal Funds for Individuals with SUD in IMDs. The Centers for Medicare & Medicaid Services announced on September 26, 2023, that North Carolina is asking for approval of a five-year extension for use of federal matching funds for services delivered to beneficiaries with substance use disorder (SUD) who reside in institutions for mental diseases (IMDs). The authority, which expires October 31, 2023, is part of the state’s section 1115 North Carolina Medicaid Reform Demonstration. The public comment period is open from September 26, 2023, through October 26, 2023. Read More
Medicaid Expansion to Launch on December 1. WRAL News reported on September 25, 2023, that North Carolina Medicaid expansion will go live on December 1, providing coverage to as many as 600,000 individuals across the state. Read More
North Carolina Launches Initiative to Promote Supported Employment Services for Individuals With Disabilities. The North Carolina Department of Health and Human Services announced on September 20, 2023, an initiative to promote supported employment services under a Medicaid waiver for individuals with intellectual and developmental disabilities. Services, which are part of a broader Inclusion Works initiative, include pre-employment, employment stabilization, and long-term support. Read More
North Carolina Releases Early Results From Healthy Opportunities Pilot Program. STAT News reported on September 22, 2023, that early results suggest that food delivery programs associated with the North Carolina Healthy Opportunities Pilot are more effective in addressing food security than programs relying on food subsidies. A more comprehensive report is set to be made public soon. Read More
Ohio
Estate Recovery Program Recovers Less Than One Percent of Fiscal 2023 Medicaid Costs. The Dalton Daily News reported on October 2, 2023, that the Ohio Medicaid estate recovery program recovered less than one percent of state Medicaid costs in fiscal 2023. In fiscal 2022, the program collected 0.25 percent of total Medicaid expenditures. Read More
Oklahoma
Oklahoma Receives Federal Waiver Approval Enabling Transition to Medicaid Managed Care. The Oklahoma Health Authority announced on October 2, 2023, that it has received federal approval for the state’s 1915(b) waiver, which will enable the state to transition from Medicaid fee-for-service to managed care effective April 1, 2024. The transition includes medical and children’s specialty plans under the SoonerSelect program. Managed dental plans will launch February 1, 2024. Federal regulators also approved the state’s proposal to increase supplemental payments to hospitals. Read More
Oregon
Oregon Holds Hearing on Medicaid CCO Profits. The Lund Report reported on September 28, 2023, that the Oregon House Committee on Behavioral Health and Health Care held a hearing after Medicaid coordinated care organizations (CCOs) reported nearly $440 million in Medicaid profits from 2020 through early 2023, according to an analysis by the Lund Report. Profits were driven by increased enrollment during the pandemic. Read More
Rhode Island
Rhode Island Agencies Propose Rate Increases for Various Mental, Elderly Health Services. The Providence Journal reported on October 3, 2023, that the Rhode Island Executive Office of Health and Human Services is proposing Medicaid reimbursement rates for several programs, including the state’s early intervention program for children, mental health services for the elderly, child therapeutic services, adult day care, the PACE program, and managed care administration. The proposal also requests funds to boost Medicaid program integrity and rental assistance for Medicaid beneficiaries at risk of homelessness. Read More
Rhode Island Seeks 1115 Waiver Amendment to Allow HCBS in Acute Hospital Settings. The Centers for Medicare & Medicaid Services announced on September 12, 2023, that Rhode Island submitted for federal approval an amendment to the state’s section 1115 Rhode Island Comprehensive Demonstration to allow the provision of home and community-based personal care services in acute care hospital settings. Public comment period is open from September 25, 2023, through October 25, 2023. Read More
Texas
Texas Implements Vendor Contracts for Medicaid FFS Prior Authorization, Enrollment, Other Functions. Texas Health and Human Services announced on September 26, 2023, the implementation of vendor contracts for the state’s Medicaid & Healthcare Partnership (TMHP), which handles Medicaid fee-for-service claims processing, provider enrollment, and a wide range of other functions. Accenture State Healthcare Services is now the state’s business operations and business integration vendor, handling Medicaid fee-for-service project management, prior authorizations, medical necessity determinations, call center, Medicaid enrollment, and other functions. Deloitte Consulting is now the state’s application maintenance and development vendor, handling provider enrollment, electronic visit verification, and other functions. A third vendor, Conduent State Healthcare, is expected to implement a contract for claims processing and other functions in December 2024. Read More
Governor Announces $4.5 Million Grant to Improve Healthcare Access in Rural Communities. Texas Governor Greg Abbott announced on September 25, 2023, a $4.5 million grant that will be awarded to four hospitals deemed critical to serving the state’s rural population. The Texas Rural Emergency Hospitals Financial Stabilization Grant will provide each hospital up to $1.1 million over two years to improve healthcare access in rural communities. Hospitals eligible for the grant funding include Crosbyton Clinic Hospital, Anson General Hospital, Falls Community Hospital and Clinic in Marlin, and St. Marks Medical Center in La Grange. The hospitals have until October 13, 2023, to apply for the grant. Read More
Texas Disenrolls 900,000 Medicaid Beneficiaries Since Redeterminations Began. The Texas Tribune reported on September 28, 2023, that Texas has disenrolled nearly 900,000 Medicaid beneficiaries since April. More than 600,000 have been for procedural errors, according to KFF. In September, 24,000 children were mistakenly removed because of a system glitch. The Texas Democratic Congressional delegation has urged the Centers for Medicare & Medicaid Services to require the state to pause all Medicaid disenrollment. Read More
Washington
Washington Selects 2024 Medicaid Value-based Purchasing Measures. The Washington State Health Care Authority announced on September 25, 2023, value-based purchasing quality performance measures for 2024 Medicaid managed care contracts. The selections are based on recommendations from external quality organization Comagine Health and represent a shift towards outcomes-based measures. Read More
National
Manufactures Begin Medicare Drug Price Negotiations With Federal Government. The New York Times reported on October 3, 2023, that drug makers agreed to begin negotiating prices with the federal government on 10 Medicare medications, even as several manufactures have filed lawsuits opposing the initiative. Read More
U.S. Senator Calls for Increased Oversight of Medicaid Plan Care Denials. U.S. Senator Bob Casey (D-PA) urged federal regulators on October 3, 2023, to crack down on Medicaid managed care plans that harm patients by denying necessary care. The letter seeks information on federal and state actions to protect Medicaid enrollees. Read More
CMMI Value-based Models Result in $5.4 Billion Increase in Federal Spending, Report Finds. Fierce Healthcare reported on October 2, 2023, that value-based care models operated by the Center for Medicare and Medicaid Innovation (CMMI) increased direct federal spending by $5.4 billion between 2011 and 2020, according to a report from the Congressional Budget Office (CBO). CMMI spent $7.9 billion to operate models, although those models only resulted in savings of $2.6 billion. CBO also anticipates CMMI will increase federal spending an additional $1.3 billion from 2021 to 2030. Read More
Short-term Federal Spending Deal to Fund Health Programs Until November. Modern Healthcare reported on October 2, 2023, that Congress agreed to a short-term federal spending deal that will ensure funding for safety net hospitals, community health centers, teaching hospitals, and the National Health Service Corps until November 17. The law additionally permits the National Disaster Medical System to deploy federal workers for emergencies and maintains the Special Diabetes Program and Special Diabetes Program for Indians. Read More
Federal Grant of Nearly $2 Million Targets Maternal Health in Predominantly Black Rural Areas. KFF News reported on October 2, 2023, that the Health Resources & Services Administration awarded nearly $2 million in grants to address maternal health in predominantly Black rural areas as part of the Rural Maternity and Obstetrics Management Strategies Program. The Institute for the Advancement of Minority Health in Madison, MS, will receive $1 million; and Mary Hitchcock Memorial Hospital in Lebanon, NH, will receive nearly $1 million. Read More
U.S. District Judge Rules Against Blocking Medicare Drug Price Negotiation Program. Reuters reported on September 29, 2023, that U.S. District Judge Michael Newman denied an attempt by the U.S. Chamber of Commerce to stop the Medicare drug price negotiation program. Newman’s ruling will allow the program to begin on October 1, but he allowed the lawsuit to continue, denying a motion by the government to dismiss it completely. Read More
One Third of Medicaid Enrollees with Opioid Disorder Did Not Receive Treatment, OIG Report Finds. The New York Times reported on September 29, 2023, that approximately one third of Medicaid beneficiaries with opioid disorder, or 500,000 people, did not receive treatment, according to a report from the U.S. Department of Health and Human Services Office of Inspector General (OIG). In 10 states, less than half of recipients received treatment. Black patients and those under the age of 19 were also less likely to access medication. The report recommended that the Centers for Medicare & Medicaid Services reduce disparities through improved outreach. Read More
CMS Seeks Public Comments on Assessing Mental Health, Addiction Equity in Medicaid, CHIP. The Centers for Medicare and Medicaid Services (CMS) announced on September 29, 2023, that it is seeking public comments on a series of questions regarding processes for assessing compliance with mental health and addiction equity requirements in Medicaid and the Children’s Health Insurance Program (CHIP). The public comment period is open through December 4. Read More
HHS Reminds States of Mandatory 12-Month Continuous Medicaid, CHIP Coverage Requirement for Children. The U.S. Department of Health and Human Services announced on September 29, 2023, that it has sent a letter reminding states of mandatory, 12-month continuous Medicaid and Children’s Health Insurance Program (CHIP) coverage requirements for children under age 19, effective January 1, 2024. The letter also notes that states may request waivers extending continuous coverage requirements for both children and adults. Read More
Medicaid, CHIP Enrollment Falls in June 2023, CMS Reports. The Centers for Medicare & Medicaid Services (CMS) announced on September 29, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) was nearly 92.6 million in June 2023, a decrease of 1.2 million from May 2023. Medicare enrollment was 66 million, up 109,118 from May 2023, including 32 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
Four States Fail to Meet All FMAP Funding Requirements, Audit Finds. MedCity News reported on September 28, 2023, that New York, Florida, Texas, and Minnesota did not meet all requirements to receive enhanced federal Medicaid (FMAP) funding during the Covid-19 public health emergency between January 1, 2020, and June 30, 2021, an Office of Inspector General (OIG) report found. The audit found that Texas and Minnesota terminated Medicaid coverage for 26,915 enrollees for unallowable reasons, while New York, Florida, and Minnesota ended coverage for 220,113 enrollees for potentially unallowable reasons. The OIG also found that Minnesota may have wrongly charged some Medicaid enrollees cost-sharing for Covid-19 related services, totaling up to $951,202. The OIG made two recommendations for CMS: work with the states to understand what amount of funding they received from the enhanced Covid-19 funding that needs to be refunded; and specifically work with Minnesota to understand if any Medicaid enrollees experienced cost-sharing for Covid-19 services and reimburse those beneficiaries. Read More
Medicaid Disenrollment Rates Are Similar by Race, Ethnicity, KFF Reports. KFF reported on September 28, 2023, that Medicaid disenrollment rates following resumption of eligibility redeterminations are similar across race and ethnicity for states, according to a KFF analysis. Findings are limited to the states that report disenrollment rates by race and ethnicity: Arizona, California, Indiana, Minnesota, and Oregon. Read More
CMS Releases Transportation Policy Guide. The Centers for Medicare & Medicaid Services (CMS) released on September 28, 2023, a guide to Medicaid transportation policies. New policies aim to help address wait times, long-distance trips, and transportation for the direct benefit of Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) beneficiaries. Read More
CMS Lacks Sufficient Data on Private Equity Owned Nursing Homes, Report Finds. Politico reported on September 26, 2023, that the Centers for Medicare & Medicaid Services (CMS) lacks sufficient data on private equity ownership of nursing homes, according to a General Accountability Office report. The report found that CMS data does not contain all private equity owners and the agency lacks the ability to easily identify private equity companies. Read More
Medicare Advantage, Prescription Drug Plan Premiums to Rise 3.5 Percent in 2024. The Centers for Medicare & Medicaid Services announced on September 26, 2023, that average premiums for Medicare Advantage plans and the Medicare Part D prescription drug program is projected to rise 3.5 percent from $17.86 in 2023 to $18.50 in 2024. Read More
HHS Awards $206 Million in Grants to Support Youth Mental Health. The U.S. Department of Health and Human Services (HHS) announced on September 25, 2023, $206 million in grants to support youth mental health. The Substance Abuse and Mental Health Services Administration awarded $131.7 million to connect at-risk youth and families to behavioral health services, the Health Resources and Services Administration awarded $55 million to improve mental healthcare access in schools and underserved areas, and the Administration for Children and Families awarded $20 million to launch the First National Center to Support Mental Health Services in the Child Welfare System. Read More
Six States Extend, Enhance Adult Medicaid Dental Coverage. NBC News reported on September 24, 2023, that Hawaii, Tennessee, Kentucky, Michigan, Maryland and New Hampshire have begun or expanded adult Medicaid dental coverage this year. Read More
CMS to Increase Oversight of Medicare Advantage Plans. Healthcare Dive reported on September 22, 2023, that the Centers for Medicare & Medicaid Services (CMS) is expected to increase oversight and regulations of Medicare Advantage (MA) plans, which currently cover over half of Medicare beneficiaries. MA plans have faced recent criticism for care denials and rising costs. Read More
CMS Releases Medicaid, CHIP Quality Data. The Centers for Medicare & Medicaid Services (CMS) announced the release of fiscal 2021 and 2022 Medicaid and Children’s Health Insurance Program (CHIP) quality data. The core data sets included 33 adult measures and 25 child measures. Read More
Industry News
Medicare Advantage Plans to Expand in 2024. Health Payer Specialist reported on October 2, 2023, that UnitedHealthcare will expand its footprint to four new states in 2024, and Cigna will serve Medicare and dual eligible beneficiaries in Nevada. Allina Health/Aetna also plans to expand to an additional county in Minnesota next year. Other payers including Independence Blue Cross, Blue Shield of California, Scan, and Alignment Health, have also released new details on their Medicare Advantage plans as open enrollment approaches. Read More
Carlyle Group in Talks to Acquire Majority of 2 Medtronic Medical Device Businesses. Reuters reported on October 2, 2023, that private equity firm Carlyle Group has entered into negotiations to acquire a majority stake in Medtronic’s patient monitoring and respiratory interventions businesses. Medtronic would retain a 35 percent stake in the businesses, which are valued at $7 billion. Read More
Elara Caring Acquires American Family Home Health. Home health provider Elara Caring announced on October 4, 2023, that it has acquired American Family Home Health, a 35-person home health care provider in Huntley, IL. Read More
Halifax Group to Acquire Home Care Division of Sodexo. Home Healthcare News reported on September 29, 2023, that Halifax Group, a private equity firm based in Washington, DC, will acquire the home care division of Sodexo, including California-based personal care provider Comfort Keepers. Halifax now serves the U.S., U.K., Ireland, France, Denmark, Norway, Sweden and Brazil. The transaction is expected to close in the fourth quarter. Financial details were not disclosed. Read More
Seven Payers’ Prior Authorization Practices Are Under Investigation by U.S House, Senate Committees. Health Payer Specialist reported on September 29, 2023, that U.S. Senate and House committees are investigating prior authorization practices among seven Medicare and Medicaid managed care plans: Aetna, AmeriHealth Caritas, CareSource, Centene, Elevance, Molina Healthcare, and UnitedHealthcare. The House Committee on Energy and Commerce and the Senate Committee on Finance are seeking information on prior authorization for early and periodic screening, diagnostic and treatment services for children; information on use of algorithms and artificial intelligence in prior authorization; and information on denials from 2018 to 2022. Read More
Centene to Lay Off 2,000 Employees. Modern Healthcare reported on September 26, 2023, that Centene will lay off 2,000 employees, more than 3 percent of its workforce. Read More
Cano Health Sells Bulk of Primary Care Center Assets in Texas, Nevada to Humana. Cano Health announced on September 26, 2023, that it has sold the bulk of the assets associated with senior primary care centers in Texas and Nevada to Humana’s CenterWell Senior Primary Care for about $66.7 million. As of August 2023, the centers in Texas and Nevada cared for approximately 15,200 members. Read More
UnitedHealth Group to Eliminate Some Medicare Advantage Plans. Modern Healthcare announced on September 22, 2023, that UnitedHealth Group will eliminate some of its Medicare Advantage offerings in 2024, including some jointly branded UnitedHealthcare-AARP plans, some dual eligible special needs plans, and its private fee-for-service MedicareDirect plan. However, United said it would expand its individual Medicare Advantage footprint in 2024. Read More
Judge Rules that Elevance Cannot Block Former Employee from Joining Molina Healthcare. Becker’s Payer Issues reported on September 21, 2023, that an Indiana judge ruled that Elevance Health cannot block its former west region Medicare president Vinod Mohan from joining Molina Healthcare in September. Elevance had filed a lawsuit stating that Mohan might disclose confidential information to Molina, which hired Mohan to serve as senior vice president of Medicare. Read More
RFP Calendar

Company Announcements
MCG White Paper:
Opioid Prescribing: Best Practices and Alternatives. MCG Health Editor MD, Meghan Tierney, and Associate Vice President and Managing Editor, Stacey Popko, MD, MBA, discuss best practices for the prevention of overdoses and potential alternatives to opioid prescribing. Download the white paper.
MCG Blogs:
MCG Managing Editor, Cheyenne Zychowski, MSN, RN, has penned a new article exploring how hospital inpatient reviews for Medicare programs may vary in the wake of the Centers for Medicare & Medicaid Services (CMS) Final Rule on Medicare Advantage. Read More
Learn about recent clarifications to the Two-Midnight Rule for Medicare Advantage plans (CMS 4201-F), as well as how evidence-based guidelines still play a critical role for the appropriate assessment of two-midnights and hospital discharge. Read More
Learn about the role of ambulatory surgical centers, how patients are selected for this level of care, and how to identify the best procedures for these facilities. Read More
Learn about inpatient rehabilitation facilities (IRFs), and tools for guiding comprehensive and compliant post-care care. Read More
HMA News & Events
Upcoming HMA Webinar:
Achieving Data Integrity Through Technology Data Governance. Health Equity, Alternative Payment Models, addressing Social Determinants of Health; these are all “north stars” in healthcare, grounded in data collection and metrics. To achieve any standard or address proper patient care coordination, the technology platforms used to enter information must be used accurately, consistently and be configured properly. At the same time, existing features and functions within the technology must also be aligned with regulatory and reporting needs. The on-going maintenance and management of any database requires a governance grounded in cross-functional management and with standards to ensure accuracy and integrity of use. Too often, provider healthcare delivery has been unable to successfully implement these systems and maintain consistent standards and use over time. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Down 9.6%, Aug-23 Data
- Arizona Medicaid Managed Care Enrollment is Down 8.4%, Jul-23 Data
- Indiana Medicaid Managed Care Enrollment Is Down 1.9%, Jul-23 Data
- Indiana Medicaid Managed Care Enrollment Is Flat, Jun-23 Data
- Kentucky Medicaid Managed Care Enrollment is Down 4.2%, Sep-23 Data
- Kentucky Medicaid Managed Care Enrollment is Down 3.2%, Aug-23 Data
- Louisiana Medicaid Managed Care Enrollment is Down 4.9%, Aug-23 Data
- Louisiana Medicaid Managed Care Enrollment is Down 3.1%, Jul-23 Data
- Michigan Medicaid Managed Care Enrollment is Up 1.4%, Jul-23 Data
- Michigan Dual Demo Enrollment is Down 4.9%, Jul-23 Data
- Mississippi Medicaid Managed Care Enrollment is Down 0.6%, Jul-23 Data
- Missouri Medicaid Managed Care Enrollment is Up 5.1%, Jun-23 Data
- Nebraska Medicaid Managed Care Enrollment Is Down 1.6%, Sep-23 Data
- Nebraska Medicaid Managed Care Enrollment Is Flat, Aug-23 Data
- Pennsylvania Medicaid Managed Care Enrollment is Down 1.6%, Jul-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- District of Columbia Medicare Advantage D-SNP Model Contract, 2023
- Georgia Medicaid Care Management RFP, 2023
- Kansas KanCare Medicaid & CHIP Capitated Managed Care RFP, Oct-23
Medicaid Program Reports, Data, and Updates:
- Alaska Health Facilities Data Reporting Program Annual Reports, 2016-21
- Arizona Medicaid Advisory Committee Meeting Materials, Jan-23
- Arkansas Office of the Medicaid Inspector General Annual Reports, 2018-22
- Arkansas DHS Annual Statistical Reports, 2018-22
- Florida KidCare Program Evaluation, CY 2021
- Georgia Medicaid Managed Care Rate Certifications, FY 2019-24
- Iowa Medical Assistance Advisory Council Meeting Materials, Aug-23
- Kansas Medical Assistance Reports, FY 2014-24
- Kansas Office of the Medicaid Inspector General Audit Reports, 2021-23
- Kentucky MCO Annual EQRO Compliance Reviews, 2017-22
- Maryland HealthChoice HEDIS Reports, 2018-21
- Maryland Annual Oral Health Legislative Report, 2019-22
- Michigan PHE Medicaid Redeterminations Monthly Reports to CMS, Aug-23
- Minnesota Medicaid Managed Care Rate Certifications, 2023
- Montana Department of Public Health and Human Services Financial Compliance Audit, FY 2019-22
- Pennsylvania HealthChoices CAHPS Quality Measures, 2020-21
- Rhode Island Long Term Care Services and Finance Performance Report, 2019-22
- Rhode Island Medicaid Managed Care Program Annual External Quality Review Technical Reports, 2015-21
- Tennessee TennCare Budget Presentation, FY 2020-24
- Texas End of Continuous Medicaid Coverage Dashboard Reports, Sep-23
- Vermont ACO Quality Measures, 2018-23
- Vermont Green Mountain Care Board Annual Reports, 2014-22
- Vermont Health Care Expenditure Analyses, 2013-20
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].
