HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- CMS AHEAD Model Offers a Flexible Framework for State-Led Total Cost of Care Initiatives

- Help at Home to Cease Operations in Alabama

- Arkansas Working Group Makes Recommendations Aimed at Improving Foster Care System

- Florida Delays Bidding for Medicaid Managed Care Contract

- AmeriHealth Caritas Names Melody Bonomo as Florida Market President

- Medicaid Eligibility Redeterminations News: Florida, Kansas, Louisiana, Mississippi, Nevada, North Carolina, Texas, Virginia

- Nebraska Launches Program to Enroll Inmates Nearing Release in Medicaid

- Nevada Medicaid Plan Aims to Improve Maternal Health-related HEDIS Scores

- New Mexico Seeks Public Comments on Section 1115 Waiver Renewal Application Addendum

- North Dakota Seeks Public Comments on IDD HCBS Waiver Renewal Application

- Utah Considers Carve Out of Medicaid ACO Pharmacy Benefits to Fee-for-Service

- Vermont Releases HCBS Business Supports RFP

- NCQA Includes Equity Measure in 2023 Health Plan Quality Ratings

- CVS Health/Aetna Promotes Mark Santos to Head of Medicaid

There will not be a Weekly Roundup on September 27, 2023. The Weekly Roundup will resume on October 4, 2023.
In Focus
CMS AHEAD Model Offers a Flexible Framework for State-Led Total Cost of Care Initiatives
This week, our In Focus section reviews the new States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model, which the Centers for Medicare & Medicaid Services (CMS) Center for Medicaid and Medicare Innovation (the Innovation Center) announced on September 5, 2023. AHEAD is the third major model that the Innovation Center has introduced to its payment portfolio since July, clearly signaling that CMS has transitioned from conducting its internal review to laying the groundwork for action on approaches that will be tested over the next decade.
CMS views this model as the next iteration of earlier total cost of care (TCOC) models that were designed and tested in three states—Maryland, Vermont, and Pennsylvania. The AHEAD model includes several important updates based on its experience with these earlier models. For example, the AHEAD model is designed to be scalable in multiple states. Although it most certainly will be adapted to state-specific markets, landscapes, and provider needs, CMS intends to apply a consistent framework across participating states.
Additionally, though Medicare has been involved in formulating some state-level total cost of care initiatives, the AHEAD model promises specific investments in primary care and enhanced member engagement to support all-payer movement toward patient-centered care.
AHEAD Model Parameters
The goal of the AHEAD Model is to improve population health and health equity in states that apply and that CMS selects for participation. CMS plans to select up to eight pilot states, each eligible to receive up to $12 million to support statewide implementation over a six-year period. States will be accountable for constraining overall growth in healthcare expenditures. Requirements centered on health equity mirror other CMS policies and are integrated throughout the model.
The model focuses heavily on strengthening primary care. The primary care AHEAD component includes Medicare reimbursement for care management, a commitment to align with ongoing Medicaid transformation efforts, and expectations for primary care practices to achieve certain goals on quality measures.
The investments in primary care are paired with global budgets for hospitals. Participating hospitals will receive a fixed payment that will include both Medicare fee-for-service and Medicaid. States will need to ensure participation among other payers, including at least the state employee health plan, Marketplace Qualified Health Plans, or other commercial payers in the state or sub-state region. Other payers will have the option to pay participating hospitals based on a global budget.
All-Payer Health Equity Approaches and Developments (AHEAD)

The model will be in operation 2024−2034, and three cohorts will be to accommodate variation in readiness among participating states and providers. The first cohort pre-implementation period is scheduled to begin in summer 2024, and the performance period is scheduled to begin as soon as January 2026. CMS expects to release additional details in fall 2023.
AHEAD Opportunities and Considerations
The AHEAD Model will need significant gubernatorial leadership and possibly from state legislators, depending upon the particular state’s related healthcare laws, and the model does provide flexibility for interested states and relevant stakeholders to develop programs that are adaptable to their needs.
Health Management Associates (HMA) experts have identified the following list of policies and considerations that states; hospitals, health systems, and provider organizations; other payers, including employers; and other stakeholders will need to bear in mind when determining whether to participate in the program.
- States will need to describe their partners and provide an assessment of their readiness to implement the AHEAD model. CMS will expect states to address whether they have legislation in place related to primary care investment and/or cost growth. Potential participating states should be able to describe their vision for population health improvement and primary care transformation, a proposed strategy for hospital and primary care provider recruitment, a plan for Medicaid and multi-payer alignment, and their current population health and health equity activities. Interested states will need early input from hospitals and health systems, providers, and other payers to define, develop, and implement a model that accommodates their healthcare landscape.
- States will develop a Medicaid hospital global budget methodology that must have CMS approval. Medicaid hospital global budgets must be implemented in the first performance year. CMS will develop a standardized Medicare fee-for-service (FFS) hospital global budget methodology, that also accommodates critical access hospitals (CAHs).
- CMS will set the parameters for quality measurement, but states will have significant flexibility to establish the metrics that will be applied for accountability and bonus purposes. CMS will use the current CMS hospital quality programs as the basis for determining eligibility for a health equity improvement bonus. CAHs will have a similar opportunity. States will work with CMS to set quality measures for participating primary care practices.
- The model requires a statewide health equity plan. Additionally, participating hospitals will need to create their own health equity plans in alignment with statewide priorities and activities.
- Participating states will need to generate savings. CMS will identify state-specific factors to determine the level of expected savings. All-payer cost growth targets include Medicare FFS, Medicare Advantage, Medicaid, commercial, state employee health plans, and marketplace-qualified health plans. States will also be responsible for performance on all-payer and Medicare FFS primary care investment targets.
The HMA team will continue to evaluate the AHEAD model as more information becomes available. We also can answer questions about the Innovation Center’s other recently announced models and the linkages with new Medicare and Medicaid regulations. For more information, contact Amy Bassano ([email protected]), Caprice Knapp ([email protected]), and Andrea Maresca ([email protected]).
HMA Roundup
Alabama
Help at Home to Cease Operations in Alabama. The Alabama Daily News reported on September 17, 2023, that Chicago-based home health provider Help at Home will cease operations in Alabama effective September 30. Help at Home will lay off 785 employees in the state. Read More
Arkansas
Arkansas Working Group Makes Recommendations Aimed at Improving Foster Care System. The Arkansas Department of Human Services (DHS) announced on September 18, 2023, that a working group has released recommendations aimed at improving the state’s foster care system, including increased prevention support, reduced barriers to public assistance programs and crisis response services, and the implementation of high-quality trauma-informed care training for staff. Arkansas Governor Sarah Huckabee Sanders established the working group by executive order. Read More
Florida
Florida Delays Bidding for Medicaid Managed Care Contract. Health Payer Specialist reported on September 18, 2023, that Florida has delayed the bidding process for its Medicaid managed care contract. Final bids are now due October 25, rather than August 22, and the notice of intent to award will be released in February 2024, instead of December 2023. The five-year contracts will include long-term care and are anticipated to begin in October 2024. Read More
Advocacy Groups File Civil Rights Complaint Over Medicaid Disenrollments. Health News Florida reported on September 14, 2023, that 13 advocacy groups filed a civil rights complaint alleging that the Florida Medicaid eligibility redeterminations process is unfair to beneficiaries who are Latino, Black, or immigrants. The complaint says that a lack of multilingual workers prevented some beneficiaries from accessing Medicaid renewal materials. Read More
AmeriHealth Caritas Names Melody Bonomo as Florida Market President. The Capitolist reported on September 19, 2023, that AmeriHealth Caritas has named Melody Bonomo as Florida market president, overseeing the company’s Medicaid managed care operations in seven counties. Bonomo previously held the position on an interim basis. Read More
Florida Disenrolls 126,573 Medicaid Enrollees Following August Redeterminations. The Florida Agency for Healthcare Administration announced on September 8, 2023, the disenrollment of 126,573 Medicaid beneficiaries following August eligibility redeterminations, including 94,783 for procedural reasons. Read More
Idaho
Idaho Medicaid Requests Funding to Hire Additional Staff in Fiscal 2025. The Idaho Capital Sun reported on September 15, 2023, that the Idaho Department of Health and Welfare (DHW) has requested $5.7 million in state and federal funds to add 60 Medicaid employees in fiscal 2025. The additional staff would support customer service and cost containment efforts. The request is part of DHW’s budget proposal submitted to Governor Brad Little. Read More
Kansas
Kansas Disenrolls More Than 81,000 Medicaid Beneficiaries Following Redeterminations. The Kansas City Star reported on September 19, 2023, that Kansas has disenrolled more than 81,000 beneficiaries following redeterminations through August. Nearly three-quarters lost coverage for procedural reasons. Another 58,718 individuals had coverage temporarily discontinued for failing to return the necessary form; they have 90 days to apply for reinstatement. Read More
Louisiana
Louisiana Disenrolls 56,000 Medicaid Beneficiaries Following July Redeterminations. The Louisiana Illuminator reported on September 15, 2023, that Louisiana disenrolled 56,000 Medicaid beneficiaries during July redeterminations. The state has now disenrolled nearly 107,000 Medicaid members in total; 82,000 lost coverage for procedural reasons and 25,000 lost coverage because they were no longer eligible. Read More
Mississippi
Mississippi Disenrolls More Than 16,000 Medicaid Beneficiaries During August Redeterminations. Mississippi Today reported on September 14, 2023, that Mississippi disenrolled more than 16,000 Medicaid enrollees during August redeterminations. Coverage was renewed for 35,402 beneficiaries. Of those disenrolled, 12,918 lost coverage for procedural reasons. The state has now disenrolled 68,626 Medicaid members. Read More
Nebraska
Nebraska Launches Program to Enroll Inmates Nearing Release in Medicaid. The Lincoln Journal Star reported on September 14, 2023, that Nebraska has launched a program to facilitate Medicaid enrollment for incarcerated individuals 60 days prior to release, as mandated by state law. The program is being implemented by the state Department of Correctional Services and the Nebraska Department of Health and Human Services. Read More
Nevada
Nevada Reinstates Medicaid Coverage for 114,000 Beneficiaries. The Nevada Independent reported on September 15, 2023, that Nevada reinstated Medicaid managed care coverage for 114,000 beneficiaries who had been disenrolled between June and August 2023 following eligibility redeterminations. Disenrolled members retroactively received fee-for-service coverage until September 1, when they were reenrolled in their Medicaid managed care plan. Read More
Nevada Medicaid Plan Aims to Improve Maternal Health-related HEDIS Scores. Nevada Medicaid plan Centene/SilverSummit Healthplan announced on September 13, 2023, an initiative aimed at improving maternal health-related HEDIS scores after receiving a D-minus on the March of Dimes maternal health report card. The company will use technology and a network of advocates from Wildflower Health to encourage members to participate in their own prenatal and postpartum care. Read More
New Mexico
New Mexico Seeks Public Comments on Section 1115 Waiver Renewal Application Addendum. The New Mexico Human Services Department (HSD) announced on September 18, 2023, the state is proposing to supplement and enhance the Medicaid Turquoise Care Section 1115 renewal application, including efforts to increase the number of providers offering personal care services (PCS) under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit. The federal comment period for this demonstration extension application addendum will be open through October 19, 2023. Read More
New Mexico Leads Nation in Percentage of Residents on Medicaid, Data Show. Becker’s Payer Issues released on September 15, 2023, that New Mexico led the nation in percentage of residents on Medicaid at 33.6 percent in 2022, according to data from the Census Bureau. Utah was lowest at 10.9 percent, while the national average was 21.2 percent. Read More
New York
New York Medicaid Pays Up To $388 Million For Services Other Federally Funded Programs Should Cover, Audits Finds. The results of two New York state audits released on September 14, 2023, found that the state Medicaid program paid up to $388 million on services that should have been covered by other federally funded programs like the Essential Plan or Medicare. The audits were released by New York State Comptroller Thomas DiNapoli. Read More
North Carolina
Governor Opposes Bill Coupling Medicaid Expansion with Casino Expansion. NC Newsline reported on September 19, 2023, that North Carolina Governor Roy Cooper voiced his opposition to a plan that would couple legislative authorization of Medicaid expansion with the expansion of casinos in the state. Read More
North Carolina House To Vote on Medicaid Expansion Authorization, State Budget. The News & Observer reported on September 18, 2023, that the North Carolina House will vote on a $30 billion state budget and a standalone bill authorizing Medicaid expansion. Read More
North Carolina Disenrolls 31,526 Medicaid Beneficiaries During August Redeterminations. The Winston-Salem Journal reported on September 15, 2023, that North Carolina disenrolled 31,526 Medicaid beneficiaries following August redeterminations. The state renewed coverage for 90,482 beneficiaries. Of those disenrolled, about 22,548 individuals lost coverage for procedural reasons. Read More
North Dakota
North Dakota Seeks Public Comments on IDD HCBS Waiver Renewal Application. The North Dakota Department of Health and Human Services announced on September 18, 2023, that it is seeking public comments on the state’s Medicaid Section 1915(c) Traditional Individuals with Intellectual Disabilities/Developmental Disability (IID/DD) Home and Community-Based Services (HCBS) waiver renewal application. The waiver covers community living support, in-home supports, adult foster care, emergency slots, residential habilitation, and other HCBS. Public comments will be accepted from through October 19. The anticipated effective date of the proposed renewal is April 1, 2024. Read More
Texas
Texas Disenrolls 328,320 Medicaid Beneficiaries Following August Redeterminations. The Austin American-Statesman reported on September 20, 2023, that Texas disenrolled 328,320 Medicaid beneficiaries following August redeterminations, including 203,322 for procedural reasons. Read More
Medicaid Eligibility Redeterminations Process is Under Federal Review. The Austin American-Statesman reported on September 20, 2023, that the Centers for Medicare & Medicaid Services (CMS) is currently auditing Texas’s Medicaid eligibility redeterminations process to ensure compliance with federal guidelines. CMS has previously worked with Texas to address technical difficulties, with more than 90,000 beneficiaries regaining coverage after being improperly disenrolled. Read More
Utah
Utah Considers Carve Out of Medicaid ACO Pharmacy Benefits to Fee-for-Service. The Utah Department of Health and Human Services announced on September 15, 2023, that it will commission a study to help determine whether the state should carve out Medicaid pharmacy benefits from Accountable Care Organizations to fee-for-service. The state released a request for statement of qualifications to procure the study, with findings due to the legislature by December 31, 2023.
Vermont
Vermont Releases HCBS Business Supports RFP. The Vermont Department of Health Access released on September 19, 2023, a request for proposals (RFP) for organizations to provide business supports to home and community-based services (HCBS) providers through the state’s Medicaid Data Aggregation & Access Program (MDAAP). MDAAP provides incentives to encourage HCBS providers to implement electronic medical records. Proposals are due on October 20, with contracts expected to begin December 1, 2023. Read More
Virginia
Virginia Reinstates Medicaid Coverage for 44,622 Beneficiaries. The Richmond Times-Dispatch reported on September 19, 2023, that Virginia has reinstated Medicaid coverage for 44,622 improperly disenrolled beneficiaries following eligibility redeterminations. About half are children. The state blamed in part a glitch in its automated eligibility review system, which failed to ensure individuals were evaluated at the individual rather than household level. Individuals will be reevaluated by September 30, following a system upgrade. Those who still do not meet eligibility requirements will have 10 days to reapply. Coverage will be extended by one year for qualifying individuals. Read More
Wisconsin
Wisconsin Senate Passes Bill to Extend Postpartum Medicaid Coverage to 12 Months. The Wisconsin Senate, on September 14, 2023, passed a bill to extend postpartum Medicaid coverage to a full year, according to a press release from State Senator Joan Ballweg (R-Markesan). The legislation has been referred to the Assembly Committee on Health, Aging and Long-Term Care. Read More
National
NCQA Includes Equity Measure in 2023 Health Plan Quality Ratings. Modern Healthcare reported on September 19, 2023, that the National Committee for Quality Assurance released 2023 health plan quality ratings, including measures intended to assess an organization’s ability to address health equity and disparities based on race and ethnicity. Approximately 92 percent of plans were able to provide the data. Read More
CMS Releases Final Rule Aimed at Streamlining Enrollment for Medicare Savings Programs. Modern Healthcare reported on September 18, 2023, that the Centers for Medicare & Medicaid Services (CMS) released a final rule aimed at simplifying the enrollment and renewal process for Medicare Savings Programs. Supplemental Security Income recipients will be automatically enrolled, and states will be required to use Medicare Part D low-income subsidy data to determine eligibility. The rule, which takes effect November 17, is projected to enroll an additional 860,000 beneficiaries. A second final rule will be released in 2024. Shared savings programs, which cover premiums and cost-sharing for low-income Medicare beneficiaries, serve more than 10 million individuals. Read More
2024 Exchange Plan Premium Increases to Hit Double Digits in Some States. Health Payer Specialist reported on September 20, 2023, that Exchange plan premium rates in some states will increase by double digits in 2024, according to data for six states. Exchange plans in Maine will have an average increase of 14.6 percent, New York 12.4 percent, Connecticut 9.4 percent, Washington 8.9 percent, Oregon 6.2 percent, and Delaware less than one percent. Read More
Pandemic-Era HCBS Policies to End in Some States, KFF Finds. KFF reported on September 19, 2023, that the expiration of pandemic-era Medicaid home and community-based services (HCBS) policies will result in the end of virtual eligibility evaluations in 23 states, lower utilization limits in 21 states, reinstated prior authorization in 19 states, and paid compensation for family caregivers in 12 states. Several other states have made these policies permanent. Read More
Proposed Federal Rules Target Health Plan Noncompliance with Behavioral Health Parity Laws. Politico reported on September 17, 2023, that the Biden Administration has proposed regulations aimed at ensuring health plans comply with behavioral health parity laws, including fines for organizations that unfairly limit access to mental healthcare. The new rules would limit prior authorization of behavioral health services, require plans to audit provider networks, and examine out-of-network reimbursement rates. The proposed regulations are open for public comment until October 2. Read More
More Than 77 Percent of Hospitals Will Face Readmissions Penalties in Fiscal 2024. Modern Healthcare reported on September 15, 2023, that 77.6 percent of hospitals will face readmissions penalties in fiscal 2024, compared to approximately 74.6 percent in fiscal 2023. Most hospitals will face penalties of less than 1 percent of their readmissions. Read More
Senators Agree to Reauthorize, Increase Spending on Certain Health Programs. Senators Bernie Sanders (I-VT) and Roger Marshall (R-KS) have agreed to reauthorize and increase spending on health programs such as the Community Health Center Fund, National Health Service Corps, and Teaching Health Centers Graduate Medical Education. The bill will be marked up on September 21. Read More
Healthcare Legislation at Risk Ahead of Potential Government Shutdown. Modern Healthcare reported on September 13, 2023, a potential government shutdown this month threatens several pieces of healthcare legislation with a September 30 expiration date. Legislation on the agenda involve Medicaid Disproportionate Share Hospital payments, funding for community health centers and teaching hospitals, the Pandemic and All-Hazards Preparedness Act of 2006, the SUPPORT for Patients and Communities Act of 2018, and The President’s Emergency Plan for AIDS Relief (PEPFAR). Read More
Medicare Providers Object to Proposed Rate Cut in 2024. Modern Healthcare reported on September 18, 2023, that hospital and physician groups objected to Medicare rate cuts proposed by the Centers for Medicare & Medicaid Services for 2024. The draft regulation is expected to be finalized this fall. Read More
Chamber of Commerce Seeks to Block Medicare Drug Price Negotiation. Reuters reported on September 15, 2023, that a lawyer for the U.S. Chamber of Commerce urged a federal judge to block the Biden Administration from implementing the Medicare Drug Price Negotiation Program before October 1. Read More
FIDE-SNPs Are Falling Short on Care Coordination of Dual Eligibles, Survey Finds. Fierce Healthcare reported on September 14, 2023, that individuals in Fully Integrated Dual Eligible Special Needs Plans (FIDE-SNPs) are reporting “significantly lower ratings of care coordination” than individuals in non–D-SNP Medicaid Advantage plans, according to an analysis of Medicare Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey data. Ratings were higher for customer services and care quality. Results were reported in a JAMA Health Forum research letter. FIDE-SNPs respondents did report “significantly higher ratings” than those in coordination-only D-SNPs in care quality but were not significantly different on other measures. Read More
Industry News
CVS Health/Aetna Promotes Mark Santos to Head of Medicaid. Health Payer Specialist reported on September 13, 2023, that CVS Health/Aetna has named Mark Santos head of Medicaid. Santos was previously vice president and head of diversified commercial solutions. Read More
AccentCare Names Laura Tortorella as CEO. Modern Healthcare reported on September 14, 2023, that AccentCare appointed Laura Tortorella as chief executive, effective October 2. Tortorella, who will replace Steve Rodgers, previously served as chief operational officer for Steward Health Care System. Read More
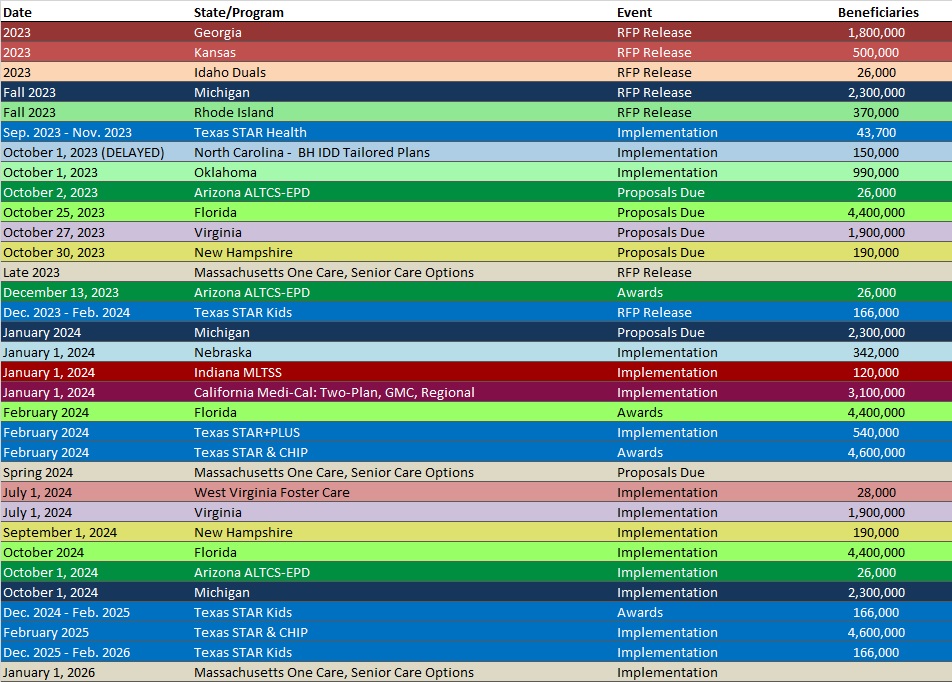
RFP Calendar
Company Announcements
MCG White Paper:
Opioid Prescribing: Best Practices and Alternatives. MCG Health Editor MD, Meghan Tierney, and Associate Vice President and Managing Editor, Stacey Popko, MD, MBA, discuss best practices for the prevention of overdoses and potential alternatives to opioid prescribing. Read More
HMA News & Events
Upcoming HMA Conference:
You Be the Judge: Innovative and Potentially Disruptive Models in Care Delivery. Our highly popular “Shark Tank”-style breakout session returns again this year with The Pitch: Innovative and Potentially Disruptive Models in Care Delivery. Early-stage healthcare companies will present their solutions for improving care delivery, addressing equity, managing risk, and engaging members through innovative models and new technologies. A seasoned panel of managed care executives will listen to “the pitch” and weigh in on each company’s value proposition. Learn about some of the latest innovations in care delivery models and gain an understanding of how to best approach managed care partners when considering value-based contracting or other network arrangements. Click here to register.
Upcoming HMA-Partnered Webinar:
Achieving Data Integrity through Technology Data Governance. Health Equity, Alternative Payment Models, addressing Social Determinants of Health; these are all “north stars” in healthcare, grounded in data collection and metrics. To achieve any standard or address proper patient care coordination, the technology platforms used to enter information must be used accurately, consistently and be configured properly. At the same time, existing features and functions within the technology must also be aligned with regulatory and reporting needs. The on-going maintenance and management of any database requires a governance grounded in cross-functional management and with standards to ensure accuracy and integrity of use. Too often, provider healthcare delivery has been unable to successfully implement these systems and maintain consistent standards and use over time. This presentation will provide an overview of the common barriers in achieving data integrity and an overview of proven methods for data governance. We will explore practical steps organizations can take to assess current structure and management practices along with addressing the needs of care delivery teams. Click here to register.
Upcoming Wakely, an HMA Company, Webinar:
Financial Challenges and Opportunities in the Medicare Advantage Market. The Medicare Advantage (MA) financial picture is constantly evolving. This webinar will talk through key financial pressures for partners (payers and risk-taking providers) in the MA space and discuss the risk-mitigating techniques that should be considered when managing an MA book of business. If your organization is a payer or provider participating in MA, it could benefit from performing an opportunity assessment. Monday, September 25, 2pm ET. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Down 6.2%, Jun-23 Data
- New Jersey Medicaid Managed Care Enrollment is Up 2.7%, Aug-23 Data
- North Dakota Medicaid Expansion Enrollment is Down 9.9%, Aug-23 Data
- North Dakota Medicaid Expansion Enrollment is Down 5%, Jul-23 Data
- Puerto Rico Medicaid Managed Care Enrollment is Flat, Sep-23 Data
- Puerto Rico Medicaid Managed Care Enrollment is Down 3.6%, Aug-23 Data
- Tennessee Medicaid Managed Care Enrollment is Up 1.1%, Aug-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Rhode Island Medicaid Actuarial and Financial Analysis Support RFP, Sep-23
- South Dakota Medicare D-SNP Contract, 2024
- Utah Pharmacy Study Cost Assessment RFSQ, Sep-23
- Vermont HCBS Business Supports RFP, Sep-23
- Virginia Medicare D-SNP Contract, 2024
Medicaid Program Reports, Data, and Updates:
- Arizona Medicaid Managed Care Capitation Rates and Actuarial Certification, 2024
- Florida PHE Medicaid Redeterminations Monthly Report to CMS, Aug-23
- Idaho Facts, Figures, Trends Annual Publication, 2012-23
- Louisiana Medicaid Managed Care Actuarial Rate Certifications and Data Books, 2018-24
- Louisiana CHIP Annual Reports, SFY 2010-23
- Louisiana Health Insurance Surveys, 2011-21
- Minnesota DHS EQR Annual Technical Reports, 2016-21
- Mississippi PHE Medicaid Redeterminations Monthly Reports to CMS, Aug-23
- Missouri HealthNet Monthly Management Reports, 2014-22, Jul-23
- Montana DPHHS Medicaid Report, 2019-23
- Ohio Financial Alignment Initiative MyCare Ohio: Evaluation Reports, 2018-22
- Oklahoma Medicaid SoonerCare Choice Annual Reports, 2012-22
- South Carolina Medicaid Managed Care Rate Certifications, SFY 2019-24
- Texas PHE Medicaid Redeterminations Monthly Reports to CMS, Aug-23
- Vermont EQRO Annual Technical Reports, 2015-23
- Wyoming Medicaid Care Management Entity EQR Report, SFY 2022
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
