HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: New Hampshire Releases Medicaid Managed Care RFP

- Redeterminations News: Arizona, Arkansas, Idaho, West Virginia

- California Medicaid Director Jacey Cooper Is Leaving to Join CMS

- District of Columbia Receives Approval for Community-Based Mobile Crisis Services SPA

- Florida Renews Medicaid Utilization Management Contract with Acentra Health

- Hawaii Receives $4 Million Project LAUNCH Federal Grant to Improve Children’s Behavioral Health

- Michigan Expects Medicaid Community Health Worker Benefit to Impact 50,000 Residents If Approved

- BCBS-NC Names Angela Boykin CEO of Medicaid Plan

- Oregon to Seek Federal Approval for Basic Health Plan

- Pennsylvania to Review Rates for Providers Serving Individuals with Intellectual Disabilities, Autism

- CMS to Lower Cost of 34 Prescription Drugs Beginning October 1

- Walmart May Buy Majority Stake in ChenMed

In Focus
New Hampshire Releases Medicaid Managed Care RFP
This week, our In Focus section reviews the New Hampshire Medicaid Care Management (MCM) request for proposals (RFP), which the state’s Department of Health and Human Services released on September 8, 2023. The new contracts will be worth approximately $1.1 billion and will provide full-risk, fully capitated Medicaid managed care services to approximately 190,000 beneficiaries. Implementation will begin September 2024.
MCM Program
The MCM program covers traditional Medicaid, the Children’s Health Insurance Program (CHIP), and the state’s adult Medicaid expansion Granite Advantage Health Care Program. MCM provides integrated acute care, behavioral health, and pharmacy services. Managed long-term services and supports are not included in the program.
Incumbents are AmeriHealth Caritas, Boston Medical Center/WellSense, and Centene/New Hampshire Healthy Families.
RFP
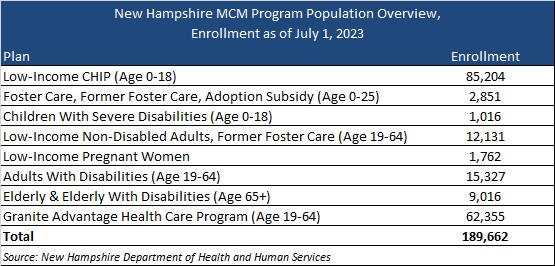
New Hampshire will award contracts to three Medicaid managed care organizations (MCOs). MCOs will cover the populations outlined in Table 1.
Table 1. New Hampshire MCM Program Enrollment as of July 1
The state outlines several key areas of focus within the RFP, including introducing a primary care and preventive services model of care—an approach centered on patient-provider relationships and provider-delivered care coordination. The RFP also will have a greater emphasis on priority populations, such as individuals with inpatient admissions for behavioral health diagnoses; children in the child welfare system; babies with low weight or neonatal abstinence syndrome; and people who are incarcerated and eligible for the Community Reentry demonstration program, pending approval from the Centers for Medicare & Medicaid Services.
Timeline
Mandatory letters of intent are due September 18, 2023, and a mandatory conference will take place September 21. Proposals are due October 30, 2023. An award date has yet to be announced, but the state contract discussions with selected MCOs will occur November 20−December 11, 2023. Contracts will run from September 1, 2024, through August 31, 2029.
Evaluation
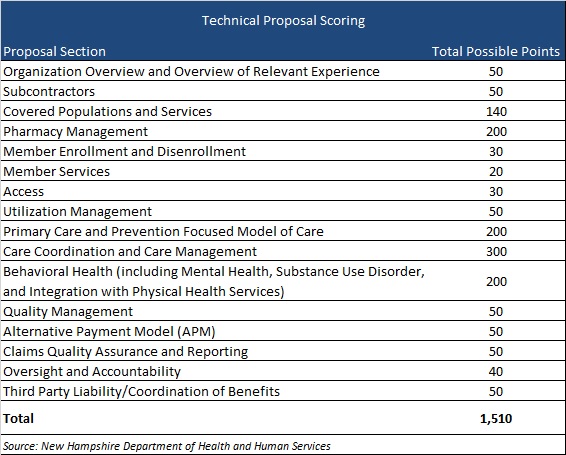
MCOs will be scored on their ability to meet a possible 2,160 points. The technical proposal comprises a possible 1,510 points, as shown in Table 2.
Table 2. Technical Proposal Scoring
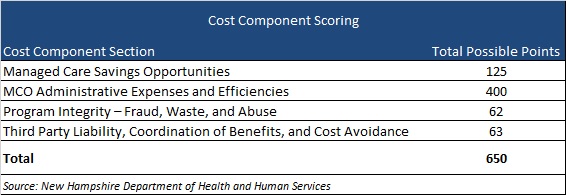
The cost component sections will make up 650 points, as shown in Table 3.
Table 3. Cost Component Scoring
HMA Roundup
Arizona
Arizona Announces Feature to Simplify Medicaid Application, Renewal Processes. The Arizona Health Care Cost Containment System (AHCCCS) announced on September 8, 2023, that it has launched AHCCCS Connect, a feature to help Medicaid members more easily apply for and renew coverage. AHCCCS Connect sends personalized reminders and updates to Medicaid applicants and members to guide them through every step of the Medicaid enrollment process. Read More
Arkansas
Arkansas Settles Lawsuit Over Medicaid Beneficiaries Who Lost HCBS Waiver Benefits. Bloomberg Law reported on September 12, 2023, that Arkansas has reached an agreement to pay $120,000 each to Medicaid beneficiaries who lost home and community-based (HCBS) waiver benefits. The three named plaintiffs filed the federal lawsuit in U.S. District Court in Arkansas. Read More
Arkansas Disenrolls 72,519 Medicaid Beneficiaries During August Redeterminations. The Arkansas Department of Human Services announced on September 8, 2023, the disenrollment of 72,519 Medicaid beneficiaries during August redeterminations. The state renewed coverage for 50,662 beneficiaries. Read More
California
California Medicaid Director Jacey Cooper Is Leaving to Join CMS. Health Payer Specialist reported on September 13, 2023, that California Medicaid director Jacey Cooper is leaving the California Department of Health Care Services on October 20. She will be joining the state demonstrations group at the Centers for Medicare & Medicaid Services (CMS) in November. Read More
Assembly Approves Ballot Measure on Behavioral Health Funding for 2024. The Associated Press reported on September 12, 2023, that the California assembly voted to put a ballot measure before voters in March 2024 to reevaluate the way counties are funding mental and behavioral health programs. The measure aims in part to address homelessness in the state. Read More
California Announces Additional $119 Million in Funding for Housing Instability, Homelessness. The California Department of Health Care Services (DHCS) announced on September 6, 2023, that their second batch of round one award funding for the Behavioral Health Bridge Housing (BHBH) program went to 12 California counties, totaling $119 million. DHCS will contribute a total of $1.5 billion to the BHBH program, with nearly a billion in the first round of awards. BHBH funding will help address housing instability and homelessness for individuals with serious behavioral health conditions, including serious mental illness or a substance use disorder. Read More
Connecticut
Connecticut Fails to Report $1.8 Million for Violating Federal EVV Rules, Audit Finds. Fox 61 reported on September 12, 2023, that the Connecticut Department of Social Service (DDS) failed to report nearly $1.8 million in federal funding losses for not complying with federal electronic visit verification (EVV) guidelines for Medicaid personal care services, according to a state audit of DDS. The audit covered fiscal years ending June 30, 2019, 2020, and 2021. Read More
District of Columbia
District of Columbia Receives Approval for Community-Based Mobile Crisis Services SPA. The Centers for Medicare & Medicaid Services announced on September 8, 2023, that it has approved the District of Columbia’s community-based mobile crisis state plan amendment (SPA). DC can now provide 24/7 Medicaid services to eligible individuals experiencing a behavioral health or substance use crisis. Read More
Florida
Florida Renews Medicaid Utilization Management Contract with Acentra Health. Acentra Health, formerly known as Kepro, announced on September 7, 2023, that it has been awarded a five-year contract with the Florida Agency for Health Care Administration to continue overseeing utilization management services for Medicaid fee-for-service beneficiaries. Acentra will also provide utilization review for certain Medicaid managed care carve-outs, including behavior analysis and prescribed pediatric extended care. The contract includes five option years. Read More
Florida House Speaker Creates Select Committee on Health Innovation. Health News Florida announced on September 11, 2023, that Florida House Speaker Paul Renner (R-Palm Coast) has created the House Select Committee on Health Innovation ahead of the 2024 legislative session in January. The committee will be chaired by Representative Kaylee Tuck (R-Lake Placid) and will focus on access and affordability in health care. Read More
Florida ACO Saves $14 Million. Fierce Healthcare reported on September 7, 2023, that the Florida Blue and primary care provider company Adelade accountable care organization (ACO) has saved over $14 million in two years. The partnership serves over 41,000 patients and saw greater reductions in hospitalizations and emergency department visits in participating practices than non-participating practices. The 59 primary care practices within the partnership also outperformed market rates of diabetes control and cancer screenings. Read More
Florida Owes $106 Million in Medicaid Managed Care Rebates to Federal Government, OIG Finds. The Center Square reported on September 6, 2023, that Florida did not refund the federal government’s share of Medicaid managed care rebates, which totaled over $106 million between 2015 and 2020, according to an Office of the Inspector General (OIG) audit. OIG recommended that the state refund the $106 million to the federal government. Read More
Hawaii
Hawaii Receives $4 Million Project LAUNCH Federal Grant to Improve Children’s Behavioral Health. The Hawaii State Department of Health (DOH) announced on September 8, 2023, receipt of a $4 million Project Linking Actions for Unmet Needs in Children’s Health (LAUNCH) federal grant to promote the behavioral health of children through age eight. The funds will go to the DOH Children with Special Health Needs Branch in annual installments of $800,000 over five years. A total of 13 states have received Project LAUNCH grants. Read More
Idaho
Idaho Completes Medicaid Redetermination Process. The Idaho Department of Health and Welfare (DHW) announced on September 8, 2023, that the state has completed the Medicaid redeterminations process, with 121,296 beneficiaries disenrolled and 31,900 renewed. Of those determined ineligible, 30 percent obtained coverage through the state’s health insurance marketplace. Idaho’s program also includes an eligibility reconsideration period that retroactively restores coverage for qualifying individuals who reapply within 90 days. Read More
Michigan
Michigan Expects Medicaid Community Health Worker Benefit to Impact 50,000 Residents If Approved. State of Reform reported on September 11, 2023, that the Michigan Department of Health and Human Services (MDHHS) estimates that the state plan amendment to recognize community health worker services as a Medicaid benefit will impact at least 50,000 residents if approved. MDHHS is currently evaluating submitted comments for potential modifications to the policy. Read More
Minnesota
Minnesota Announces $14 Million In ARPA Grants for Disabled, Aging Population. The Minnesota Department of Human Services announced on September 7, 2023, that over $14 million in grants from the federal American Rescue Plan Act (ARPA) will be allocated to 120 community-based providers to expand services to people with disabilities and aging populations in diverse communities, rural areas, and regional centers. Read More
North Carolina
BCBS-NC Names Angela Boykin CEO of Medicaid Plan. Becker’s Payer Issues reported on September 6, 2023, that Blue Cross and Blue Shield of North Carolina (BCBS-NC) has appointed Angela Boykin as the new chief executive of Healthy Blue, BCBS-NC’s Medicaid plan, effective September 1. Read More
North Dakota
North Dakota Receives Federal Approval for Revised Essential Health Benefits. North Dakota Insurance Department announced on September 5, 2023, that the federal government has approved the state’s application to change the essential health benefit (EHB) benchmark plan for Affordable Care Act (ACA) plans, including individual market Exchange plans and small-group plans offered by employers, beginning January 1, 2025. Added benefits for qualifying plans in the state include coverage of insulin/insulin supplies, hearing aids, nutritional benefits, weight loss drugs, periodontal disease, positron emission tomography scans, and opioids. Grandfathered plans or large-group plans will be exempt from EHB benchmark changes. Read More
Oregon
Oregon to Seek Federal Approval for Basic Health Plan. Oregon Public Broadcasting announced on September 12, 2023, that Oregon is seeking federal approval for a basic health plan, which would cover people who earn 138 percent to 200 percent of the federal poverty level. The program would provide services similar to Oregon Medicaid (excluding long-term care) to 100,000 individuals beginning in July 2024. Read More
Oregon Proposes Medicaid Rent Assistance Benefit to Start November 2024. The Cannon Beach Gazette reported on August 7, 2023, that the Oregon Health Authority and Oregon Housing and Community Services have announced that the short-term Medicaid rent assistance benefit under a proposed five-year Section 1115 Medicaid will begin in November 2024. The Centers for Medicare & Medicaid Services must still approve the waiver. Additionally, Medicaid members would start receiving benefits for climate-related supports in January 2024 and for food insecurity in January 2025. Read More
Residents Spend Nearly $8,000 Annually on Healthcare Costs. The Oregon Capital Chronicle reported on September 7, 2023, that Oregon has spent about $31 billion on health care in 2021, a 40 percent increase since 2013, causing residents to spend nearly $8,000 per person of their annual household budgets on insurance premiums, prescription drugs, and over-the-counter health care items, according to a study released by the Oregon Health Authority. Read More
Pennsylvania
Pennsylvania to Review Rates for Providers Serving Individuals with Intellectual Disabilities, Autism. Governor Josh Shapiro announced on September 12, 2023, that the Pennsylvania Department of Human Services will review the fee schedule for home and community-based services for Medicaid beneficiaries with intellectual disabilities and autism. The most recent increase to the fee schedule was effective January 1, 2022. Data is typically reviewed every three years. Read More
Virginia
Virginia Budget Amendments Include Increased Funds for Certain Medicaid Services. The Virginia Mercury reported on September 11, 2023, that a recently adopted Virginia budget agreement includes increased funding for certain Medicaid services, including 500 more developmental disability waiver slots; higher pay for personal care, companion and temporary services providers; easing of emergency room utilization policies; and an Exchange plan reinsurance program. Read More
West Virginia
West Virginia Disenrolls 22,562 Medicaid Beneficiaries Following Redeterminations. The West Virginia Department of Health and Human Resources announced on August 25, 2023, the disenrollment of 22,562 Medicaid beneficiaries during August redeterminations. Of those disenrolled, 18,796 lost coverage for procedural reasons and 3,766 were no longer eligibile. Read More
National
CMS to Lower Cost of 34 Prescription Drugs Beginning October 1. The Centers for Medicare & Medicaid Services (CMS) announced on September 13, 2023, a list of 34 prescription drugs that are expected to have lower Part B beneficiary coinsurance effective October 1. Savings could be between $1 and $618 per average dose. Read More
CMS Grants IHS One-Year Extension to Claim Medicaid Reimbursement Outside of Facilities. The Centers for Medicare & Medicaid Services (CMS) issued on September 8, 2023 an informational bulletin to announce that it will extend a grace period permitting Indian Health Service (IHS) and tribal facilities to continue claiming Medicaid reimbursement for services provided outside of the “four walls” of facilities. The extension will last for one year, from February 11, 2024, to February 11, 2025. Read More
HHS Announces Proposed Rule to Improve Healthcare Access for Patients with Disabilities. Modern Healthcare reported on September 8, 2023, that the U.S. Department of Health and Human Services (HHS) released a proposed rule requiring providers to accommodate patients with disabilities and ensure facilities are accessible. Providers will also need to modify medical equipment to accommodate patients with disabilities and revise biases found in clinical support tools. Providers would be prohibited from utilizing disability status as a determining factor for medical interventions. Read More
Drug Rebates Increase Costs for Medicare Beneficiaries, Save Money for PBMs, GAO Finds. The Ohio Capital Journal reported on September 11, 2023, that drug rebates increased costs for Medicare beneficiaries, according to a U.S. Government Accountability Office (GAO) report. The report recommended that the Centers for Medicare & Medicaid Services study the effects of pharmacy benefit manager (PBM) drug coverage decisions on Medicare beneficiaries. Read More
Improper, Illegal Marketing Practices Target Medicare-eligible Individuals, Survey Finds. Health Payer Specialist reported on September 12, 2023, that improper and illegal marketing practices are targeting Medicare-eligible individuals, specifically low income and black adults, according to a Commonwealth Fund survey. Practices include false advertising, unsolicited telemarketing calls, illegal requests for Social Security and Medicare numbers, and pressuring individuals to switch from traditional Medicare to Medicare Advantage. Read More
Exchange Enrollment Increased by 29 Percent Since 2020, KFF Finds. KFF reported on September 7, 2023, that Affordable Care Act (ACA) Exchange enrollment increased by approximately 29 percent between early 2020 and early 2023. About 80 percent of individual market enrollees have subsidized coverage, partly due to enhanced subsidies resulting from the Inflation Reduction Act. Exchange enrollment is expected to continue growing due to Medicaid eligibility redeterminations. Read More
73 Percent of Medicaid Disenrollments Are Due to Procedural Reasons, KFF Finds. KFF reported on September 7, 2023, that 73 percent of Medicaid unwinding disenrollments were due to procedural reasons as of September 2023. The Centers for Medicare & Medicaid Services has contacted states with high procedural disenrollment rates to express concern and encourage states to reduce the rates. Read More
Providers Criticize Budget Neutrality in Proposed 340B Rule. Modern Healthcare reported on September 6, 2023, that providers criticized the budget neutrality aspect of the proposed 340B rule in over 150 comments submitted to the Centers for Medicare & Medicaid Services (CMS). To maintain budget neutrality under the proposed changes, CMS plans to reduce reimbursement for other outpatient services, such as non-drug items, to hospitals by $7.8 billion over 16 years starting in 2025. Stakeholders have until September 11 to submit comments and a final rule is expected in November. Read More
MACPAC Meeting Is Scheduled for September 21-22. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on September 7, 2023, that its next meeting will be held on September 21-22. The topic for discussion will be Medicaid continuous coverage unwinding and the resulting challenges for states and beneficiaries. Read More
Industry News
Walmart May Buy Majority Stake in ChenMed. Reuters reported on September 8, 2023, that Walmart may purchase a majority stake in ChenMed, which operates primary care clinics for seniors. The deal would reportedly value ChenMed at several billion dollars. Read More
Ensign Group Acquires Two Skilled Nursing Facilities in South Carolina. The Ensign Group announced on September 5, 2023, that it has acquired Ashley River Healthcare, a 125-bed skilled nursing facility in Charleston, SC, and the Reserve Healthcare and Rehabilitation, a 135-bed skilled nursing facility in Hanahan, SC. The acquisitions were completed this month. Read More
AHIP Names General Counsel Julie Simon Miller Interim CEO. AHIP announced on September 7, 2023, that it has named General Counsel Julie Simon Miller interim chief executive as the search for a permanent replacement of Matt Eyles continues. Matt Eyles’ resignation is effective October 2. Read More
RFP Calendar

HMA News & Events
Upcoming HMA Conference:
You Be the Judge: Innovative and Potentially Disruptive Models in Care Delivery. Our highly popular “Shark Tank”-style breakout session returns again this year with The Pitch: Innovative and Potentially Disruptive Models in Care Delivery. Early-stage healthcare companies will present their solutions for improving care delivery, addressing equity, managing risk, and engaging members through innovative models and new technologies. A seasoned panel of managed care executives will listen to “the pitch” and weigh in on each company’s value proposition. Learn about some of the latest innovations in care delivery models and gain an understanding of how to best approach managed care partners when considering value-based contracting or other network arrangements. Click here to register.
Upcoming Wakely, an HMA Company, Webinar:
Financial Challenges and Opportunities in the Medicare Advantage Market. The Medicare Advantage (MA) financial picture is constantly evolving. This webinar will talk through key financial pressures for partners (payers and risk-taking providers) in the MA space and discuss the risk-mitigating techniques that should be considered when managing an MA book of business. If your organization is a payer or provider participating in MA, it could benefit from performing an opportunity assessment. Monday, September 25, 2pm ET. Click here to register.
Wakely, an HMA Company, White Papers:
D-SNPs – What, Why, How. Dual-eligible Special Needs Medicare Advantage plans (D-SNPs) have been a popular, growing trend in the Medicare Advantage (MA) marketplace over the past several years. D-SNPs are MA plans that are geared to meet the unique needs of beneficiaries that are dually eligible for both Medicare and Medicaid. This white paper provides the fundamentals for understanding what a D-SNP is, the different kinds of D-SNPs, and some considerations for developing D-SNP plans for inclusion in a Medicare Advantage Organization’s (MAO) portfolio of plan options. Read More
CMS Releases CY 2024 MPFS Proposed Rule. On July 13, 2023, the U.S. Centers for Medicare and Medicaid Services (CMS) issued the calendar year (CY) 2024 Medicare Physician Fee Schedule (MPFS) Proposed Rule, which describes potential changes to the fee schedule for 2024. This paper summarizes proposed changes that are likely to impact physicians in 2024. If the CY 2024 proposed changes become final, then the average Medicare reimbursement for physicians will decrease by approximately 1.2% from 2023. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Michigan Medicaid Managed Care Enrollment is Up 1.5%, Jun-23 Data
- Michigan Dual Demo Enrollment is Down 2.6%, Jun-23 Data
- New Jersey Medicaid Managed Care Enrollment is Up 4%, Jul-23 Data
- North Carolina Medicaid Managed Care Enrollment is Up 2.8%, Jun-23 Data
- Oklahoma Medicaid Enrollment is Down 1.7%, Jul-23 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 1.2%, Jul-23 Data
- Virginia Medicaid Managed Care Enrollment is Up 3.9%, May-23 Data
- Virginia Medicaid MLTSS Enrollment is Up 2.1%, May-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- New Hampshire Medicaid Care Management RFP, 2023
Medicaid Program Reports, Data, and Updates:
- Arizona AHCCCS External Quality Review Annual Reports, 2022
- Arizona Behavioral Health Annual Reports, SFY 2018-22
- Arizona LTC Home and Community Based Services Annual Reports, 2012-22
- Colorado Medicaid HEDIS Reports, 2013-22
- Michigan Medicaid Health Plan External Quality Review Reports, FY 2014-22
- Michigan Medicaid Health Plan CAHPS Reports, 2015-23
- Michigan Dental Health Plans External Quality Review Technical Reports, 2020-22
- Missouri HealthNet Managed Care External Quality Review Reports, 2015-22
- North Carolina DHHS Strategic Plan, 2021-23
- North Carolina Medicaid Managed Care Quality Strategy, 2018-23
- North Dakota Medicaid Expansion Quality Strategy Plans, 2018-23
- TennCare Annual Reports, FY 2010-22
- Tennessee Medicaid Quality Assessment and Performance Improvement Strategy Reports, 2013-22
- Tennessee Medicaid Managed Care HEDIS/CAHPS Reports, 2015-22
- Texas Initiatives to Reduce Avoidable Emergency Room Utilization and Improve Health Outcomes in Medicaid Reports, 2022-23
- Washington Medicaid Managed Care Comparative Analysis HEDIS Reports, 2013-22
- Washington State Mental Health Parity Analysis Reports, 2017-23
- Washington Healthier Washington Community Checkup Reports, 2017-23
- West Virginia PHE Medicaid Redeterminations Monthly Report to CMS, Aug-23
- West Virginia Medicaid Mountain Health Trust EQR Reports, 2009-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
