HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: KFF Predicts Medicaid Implications of End of PHE

- Alabama Medicaid Faces Complaint Against Sobriety Requirement for Hepatitis C Treatment

- Florida Releases Medicaid Managed Care RFI Ahead of Statewide Procurement

- Louisiana Begins Statewide Rollout of Crisis Response Services for Medicaid Members

- Maryland Governor Increases Medicaid Rates to Match Medicare in Fiscal 2023 Budget

- Medicaid Redeterminations: Massachusetts, Texas

- Missouri Awards Medicaid Managed Care Contracts

- New York Governor Hopes to Expand Reach of PACE

- North Carolina Audit Finds Deficiencies in Medicaid Eligibility Process, Provider Payments

- Oklahoma Senate Rejects Medicaid Value-Based Contracting Measures

- Oregon Task Force Meets to Discuss Federal Funding Options for Medicaid Bridge Plan

- Pennsylvania Faces Lawsuit from Hospital Association Over Medicaid Managed Care Contract Language

- Federal Lawmakers Introduce Mental Health Legislation

- Kinderhook Invests in Smoky Mountain Urgent Care as Part of Multi-State, Rural Primary Care Plan

- Medicaid Directors from AZ, CA, IN, NC to Address Redeterminations, FMAP, TeleHealth, Equity, Other Key Topics at HMA Conference in Chicago, October 10-11

In Focus
KFF Predicts Medicaid Implications of End of PHE
This week, our In Focus reviews the Kaiser Health Foundation (KFF) analysis, Fiscal and Enrollment Implications of Medicaid Continuous Coverage Requirement During and After the PHE Ends, published on May 10, 2022.
Background
The end of the public health emergency (PHE), slated for mid-July 2022, will come with significant implications for state Medicaid programs. If the PHE is not extended further, states that meet maintenance of eligibility (MOE) requirements under the Families First Coronavirus Response Act (FFCRA) will lose the enhanced 6.2 percentage point increase in the federal Medicaid match rate (FMAP) on September 30, 2022. The continuous Medicaid enrollment requirement under the MOE will also end August 1, 2022.
KFF examined two potential scenarios on how states may manage the resumption of eligibility redeterminations and disenrollments, based on two scenarios predicted by past KFF surveys. In a February 2022 survey of Medicaid directors, state officials predicted Medicaid enrollment would decline by five percent after the PHE ends. Meanwhile, in a January 2022 survey, states signaled they expect on average about 13 percent of Medicaid enrollees to be disenrolled at the end of the continuous enrollment requirement.
Enrollment
From 2019 through the end of fiscal 2022 (September 30, 2022), KFF estimates that Medicaid enrollment will grow 22.2 million, or approximately 25 percent, to 110.3 million. Baseline Medicaid growth would account for 3.5 million of the gain, while the MOE continuous enrollment requirement would account for 18.7 million. Of this predicted growth, children represent 42 percent, Affordable Care Act (ACA) expansion adults 33 percent, other adults 20 percent, persons with disabilities three percent, and seniors three percent. Over this same period, KFF estimates baseline growth would have been four percent, prior to the pandemic and MOE.
Based on the two scenarios, KFF predicts that Medicaid enrollment will decline from 5.3 million (assuming a five percent decline) to 14.2 million (assuming a 13 percent decline) from fiscal 2022 to fiscal 2023, with the largest losses expected among ACA expansion adults, other adults, and children.
Spending
KFF estimates that between fiscal 2020 and fiscal 2022, states will have received $100.4 billion in fiscal relief due to the enhanced FMAP. KFF estimates state costs due to the additional MOE enrollees is $47.2 billion. On average, the total expected fiscal relief is 2.3 times the costs of the additional enrollment. See table below.
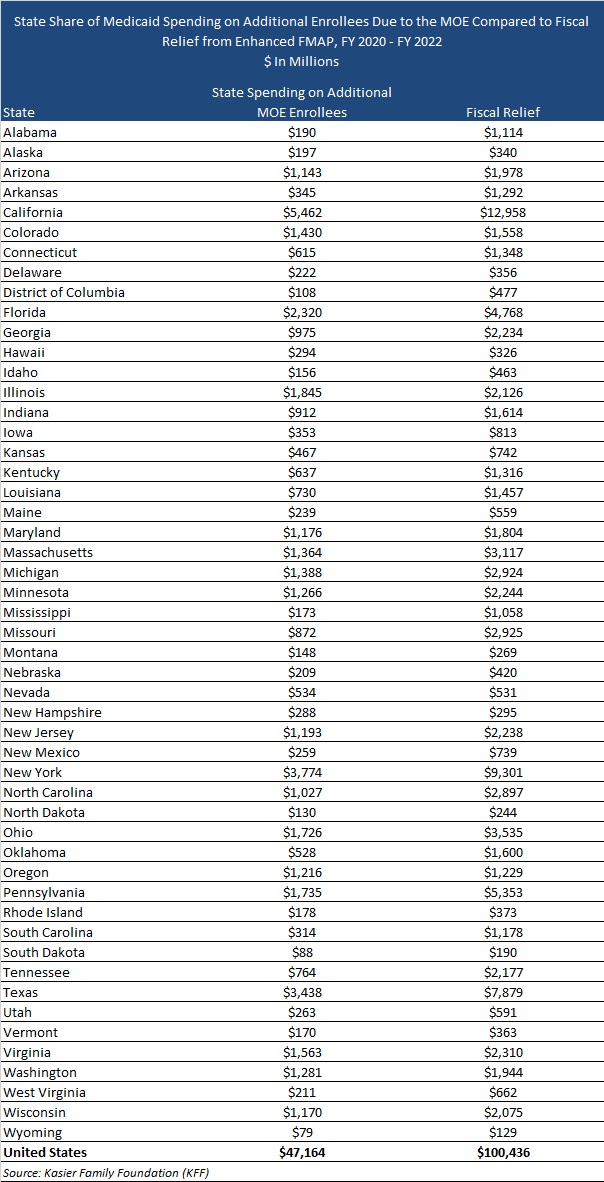
States that did not expand Medicaid tended to draw more federal fiscal relief than expansion states. However, during the pandemic, Idaho, Missouri, Nebraska, Oklahoma, and Utah expanded their Medicaid programs.
KFF estimates state Medicaid spending over the entire pandemic period will be six percent lower compared to baseline state Medicaid spending without the enhanced FMAP or enrollment growth due to the MOE, while federal spending will be 19 percent higher than baseline federal spending. After the end of the PHE, state Medicaid directors expect total Medicaid spending to increase by two percent due to changes in per enrollee expenses following the end of the PHE.
HMA Roundup
Alabama
Alabama Medicaid Faces Complaint Against Sobriety Requirement for Hepatitis C Treatment. AL.com reported on May 11, 2022, that AIDS Alabama and the Harvard Center for Health Law and Policy Innovation filed a federal administrative complaint against the Alabama Medicaid Agency, alleging that a six-month sobriety requirement for individuals on Medicaid seeking hepatitis C treatment violates the Americans with Disabilities Act. Under this policy, individuals must be drug and alcohol free for six months for Medicaid to cover the cost of hepatitis C treatment. The complaint was filed with the U.S. Department of Justice. Read More
Alabama Seeks Public Comments on Elderly, Disabled HCBS Waiver Renewal Application. Alabama Medicaid announced on May 5, 2022, it is seeking public comments on the proposed Elderly and Disabled Home and Community-Based Services (HCBS) Waiver renewal application. The application includes additional services, including skilled nursing, home modification, and assistive technology and durable medical equipment. The comment period is open until June 8. Read More
Florida
Florida Releases Medicaid Managed Care RFI Ahead of Statewide Procurement. Florida Politics reported on May 9, 2022, that the Florida Agency for Health Care Administration released a request for information (RFI), seeking best practices and innovations in business models for potential use in improving the state’s Medicaid managed care and Medicaid managed long-term care programs. The next Medicaid managed care procurement cycle is slated to begin in late 2022. Responses to the RFI are due by June 3. Read More
Lousiana
Louisiana Begins Statewide Rollout of Crisis Response Services for Medicaid Members. BRProud reported on May 4, 2022, that the Louisiana Department of Health has introduced a crisis response network for Medicaid beneficiaries across the state. The Louisiana Crisis Response System currently consists of mobile crisis response, community brief crisis support, and behavioral health crisis care in five Medicaid regions, including greater New Orleans. The system will continue with a phased rollout to the state’s remaining five regions and will add crisis stabilization services. Read More
Maryland
Governor Increases Medicaid Rates to Match Medicare in Fiscal 2023 Budget. The Daily Record reported on May 5, 2022, that Maryland Medicaid reimbursement rates will be increased to match Medicare rates beginning in July, according to Governor Larry Hogan’s supplemental budget for Fiscal 2023. Previously, Medicaid providers were paid 94 percent of Medicare reimbursement rates. Read More
Massachusetts
Massachusetts Prepares to Restart Medicaid Redeterminations When PHE Ends. Health Payer Intelligence reported on May 4, 2022, that MassHealth is preparing for the end of the public health emergency (PHE) by dedicating $5 million to community outreach, including an ethnic media campaign and canvasing communities with a high risk of coverage loss. The state is also hoping to increase “ex-parte” redeterminations, partner with insurers to connect with enrollees, hire more caseworkers to process paperwork, and update its communications strategy. Medicaid enrollment in Massachusetts increased by over 431,000 from February 2020 to February 2022. Read More
Missouri
Senate Stalls on Bill to Extend Postpartum Medicaid Coverage from 60 Days to 12 Months. The Columbia Missourian reported on May 10, 2022, that a bill (SB 698) that would extend postpartum Medicaid coverage in Missouri from 60 days to 12 months is stalling in the state Senate. The House has already approved the measure. An estimated 4,565 individuals in Missouri would be impacted by extended coverage. Read More
Missouri Awards Medicaid Managed Care Contracts. The Missouri Department of Social Services announced on May 2, 2022, contract awards for the state’s MO HealthNet Medicaid managed care program to incumbents Centene/Home State Health Plan, Anthem/Missouri Care, and UnitedHealthcare. Centene/Home State Health Plan also won a contract for a single, statewide specialty plan for foster children and children receiving adoption subsidy assistance. MO HealthNet serves nearly 950,000 members, including the state’s newly implemented Medicaid expansion population. Contracts will be effective for one year with four one-year renewal options. Read More
New York
Governor Hopes to Expand Reach of PACE. Crain’s New York reported on May 9, 2022, that New York Governor Kathy Hochul is hoping to expand the state’s Program of All-inclusive Care for the Elderly (PACE) program through administrative streamlining measures included in the proposed state budget. The measures include establishing PACE as a state-wide program separate from managed care and with its own licensure process. There are currently nine PACE organizations in New York, with 5,800 members. Read More
North Carolina
North Carolina Audit Finds Deficiencies in Medicaid Eligibility Process, Payments to Uncredentialed Providers. The North State Journal reported on May 5, 2022, that North Carolina had deficiencies in its Medicaid eligibility and termination processes and likely made payments to uncredentialled providers in fiscal 2021, according to a state audit. The audit found three eligibility errors in a sample of 152 beneficiaries, a rate of nearly two percent. Read More
Oklahoma
Senate Rejects Medicaid Value-Based Contracting Measures. The Journal Record reported on May 9, 2022, that the Oklahoma Senate rejected measures that would allow the state Medicaid program to enter into capitated contracts with provider-led accountable care organizations, sending the legislation back to committee for discussion. The Oklahoma House overwhelmingly approved the measures. Read More
Oregon
Oregon Task Force Meets to Discuss Federal Funding Options for Medicaid Bridge Plan. State of Reform reported on May 10, 2022, that the Oregon Bridge Health Care Program Task Force is considering three waiver options to obtain federal funding for a health insurance plan for individuals no longer eligible for Medicaid after the public health emergency ends. The task force will meet again on May 24, with a final decision on the bridge program waiver expected by June 14. Read More
Pennsylvania
Pennsylvania Faces Lawsuit from Hospital Association Over Medicaid Managed Care Contract Language. The Progress News reported on May 5, 2022, that the Hospital and Healthsystem Association of Pennsylvania has filed a lawsuit against the state’s Department of Human Services (DHS), alleging that the collective bargaining language in the draft Medicaid managed care contracts is beyond of the scope of DHS’ authority and will limit access to health care. The contracts historically are worth $65 billion. A group of health care organizations, the Medicaid Access Commission of Pennsylvania, has also submitted a letter to Governor Tom Wolf and DHS opposing the language that would effectively prevent non-unionized providers that have had work stoppages in the last five years from inclusion in managed care networks.
South Dakota
South Dakota Medicaid Expansion Ballot Measure May Require 60 Percent Voter Approval. SDPB Radio reported on May 6, 2022, that South Dakota voters will decide during the primary election whether to require 60 percent voter approval of ballot measures like Medicaid expansion. Senator Lee Schoenbeck (R-Watertown) moved the question from the general election in hopes of making Medicaid expansion more difficult to pass. Read More
Texas
Texas Medicaid Plan Offers Guide to Help Members Renew Coverage at End of PHE. Community First Health Plans announced on May 10, 2022, an online resource guide to help members renew their Medicaid and Children’s Health Insurance Program coverage after the end of the public health emergency on July 15. Community First has more than 160,000 Medicaid members in Texas. Read More
National
Federal Lawmakers Introduce Mental Health Legislation. Bloomberg Law reported on May 10, 2022, that Senators Bill Cassidy (R-LA) and Chris Murphy (D-CT) introduced the Mental Health Reform Reauthorization Act of 2022. The bill would stress improved coordination between agencies focusing on opioid addiction services, reauthorize funding for the Community Mental Health Services Block Grant program, allocate $25 million annually for five years so states can enforce existing mental health parity laws, and push the Centers for Medicare & Medicaid Services to strengthen mental health services for youth. House lawmakers also introduced mental health legislation to bolster federal health programs and compliance with mental health parity laws. Read More
Safety Net Hospitals Expect to See Losses from 340B Discount Limits, Survey Finds. Modern Healthcare reported on May 5, 2022, that disproportionate share hospitals, rural referral centers, and sole community hospitals expect median losses of about $2.2 million annually in contract pharmacy savings because of 340B discount limits, according to a survey from hospital industry group 340B Health. The survey also found that more than 75 percent of respondents will need to make cuts or adjustments to programs if the discount restrictions continue. Read More
U.S. Senate Subcommittee Holds Hearing on PBMs, Pushes for Transparency. Fierce Healthcare reported on May 5, 2022, that a subcommittee of the U.S. Senate Commerce Committee held a hearing on pharmacy benefit managers (PBMs) to push for transparency. PBMs “are part of an increasingly integrated, uncompetitive system”, according to Senator Richard Blumenthal (D-Connecticut), the subcommittee’s chairman. Read More
Tennessee, South Carolina Receive Federal Approval of 12-Month Postpartum Medicaid Coverage Amendments. The Centers for Medicare & Medicaid Services (CMS) announced on May 6, 2022, approval of Medicaid state plan amendments for Tennessee and South Carolina to extend Medicaid coverage to 12 months postpartum for eligible women through the American Rescue Plan Act. The amendments will expand coverage to an estimated 22,000 and 16,000 pregnant and postpartum individuals in Tennessee and South Carolina, respectively. Read More
Industry News
Kinderhook Invests in Smoky Mountain Urgent Care as Part of Multi-State, Rural Primary Care Plan. Private equity firm Kinderhook Industries announced on May 10, 2022, an investment in Smoky Mountain Urgent Care PC, a physician-owned group of clinics in rural North Carolina. The transaction is the first in Kinderhook’s plan to invest in rural family medicine providers in several states to help them grow, adopt leading technologies, and utilize best practices to better serve their communities. Benson Sloan, previously an executive at naviHealth, will serve as chief executive of the effort. Additionally, David Castor, MD, will join as regional medical director. Read More
Atar Capital Completes Acquisition of Psychological Assessment & Intervention Services. Atar Capital announced on May 10, 2022, that is has completed the acquisition of Psychological Assessment & Intervention Services (PAIS) through its portfolio company Pathways Health and Community Support. PAIS provides person-centered home and community-based services in West Virginia. Read More
Conduent Is Eligible to Bid on State Medicaid Third Party Liability Contracts Under NASPO ValuePoint. Conduent announced on May 11, 2022, that it is eligible to bid on state Medicaid third-party liability contracts under the National Association of State Procurement Officials (NASPO) ValuePoint cooperative purchasing program.
Sentara Healthcare to Launch Care Model for Uninsured, Medicaid Populations in Virginia, North Carolina. Healthcare Innovation reported on May 6, 2022, that Sentara Healthcare will launch a care model focused on the uninsured and Medicaid populations in Virginia and northeastern North Carolina. Community care centers will be established to allow health professionals from Sentara and other health systems to collaborate with community partners and focus on services that address social determinants of health. The centers will be operated by Sentara Health Plans, including Optima Health and Virginia Premier. Read More
Western Dental Acquires Mid-Atlantic Dental Partners. Western Dental announced on May 5, 2022, the acquisition of Mid-Atlantic Dental Partners, a dental support organization with 215 offices in 17 states operating under four regional brands: Dental One Partners, DentalWorks, Perfect Teeth, and Mid-Atlantic Dental Partners. The terms of the transaction were not disclosed, however Mid-Atlantic Dental Partners ownership group will receive a combination of cash and stock in the Western Dental parent company. Read More
Centene Divests Two Pharmacy Businesses as Part of Plan to Exit PBM Space. Centene announced on May 5, 2022, a definitive agreement to sell Magellan Rx to Prime Therapeutics and a separate definitive agreement to sell PANTHERx Rare to a consortium of The Vistria Group, General Atlantic, and Nautic Partners. Centene expects to receive approximately $2.8 billion from the transactions. In 2021, Centene announced plans to exit the pharmacy benefit management (PBM) space. Read More
Elite Patient Care, Provider Health Services, AllyAlign Health Combine to Form Curana Health. Elite Patient Care, Provider Health Services, and AllyAlign Health announced on May 4, 2022, that they have combined to form Curana Health, a partnership focused on providing healthcare services to senior living communities. The organization includes a medical group (Curana Health Medical Group), an operator of Medicare Advantage health plans (AllyAlign Health), and an Accountable Care Organization (Curana Health ACO). The combined Curana Health organization covers 26 states and over 1,000 senior living community partners. Read More
Anthem Completes Acquisition of Integra Managed Care. Anthem announced on May 5, 2022, that it had completed its acquisition of Integra Managed Care, a New York-based managed long-term care plan serving over 40,000 Medicaid beneficiaries in New York, Nassau, Suffolk, and Westchester counties. Integra is now part of Anthem’s Government Business Division.
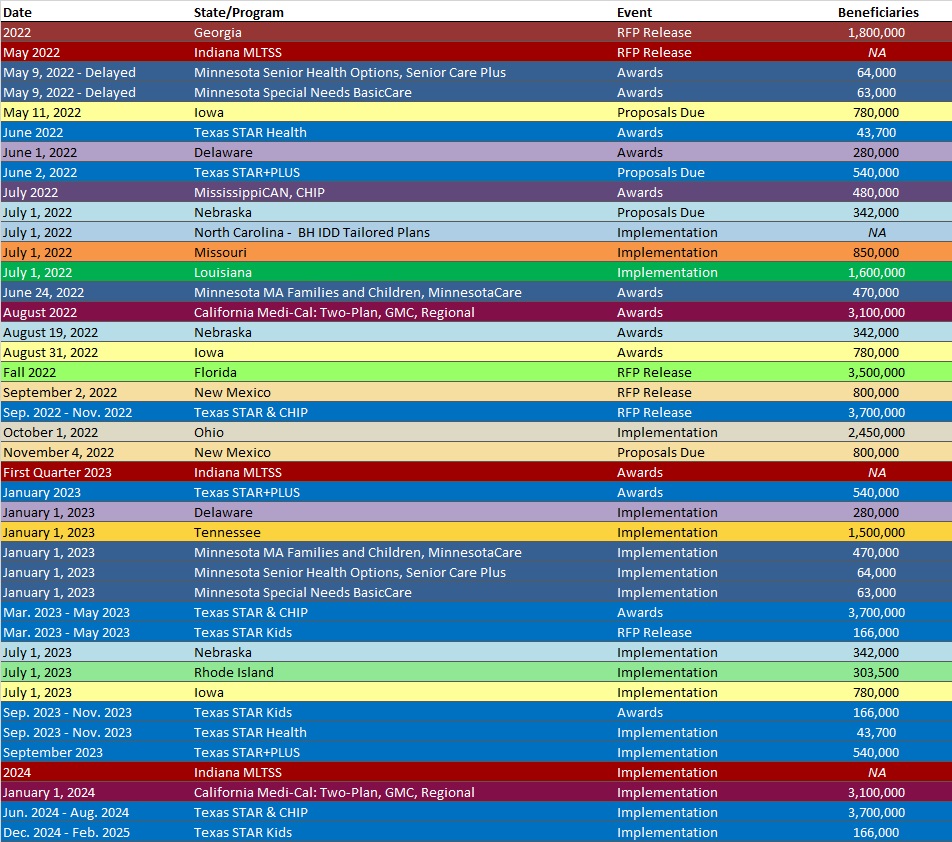
RFP Calendar
HMA News & Events
Medicaid Directors from AZ, CA, IN, NC to Address Redeterminations, FMAP, TeleHealth, Equity, Other Key Topics at HMA Conference in Chicago, October 10-11
Medicaid directors from Arizona, California, Indiana, and North Carolina will address Medicaid eligibility redeterminations, the expiration of enhanced FMAP, telehealth, equity, and other important topics during a keynote Q&A session at the fifth annual HMA conference, October 10-11, 2022, at the Fairmont Chicago, Millennium Park. To register visit https://conference.healthmanagement.com/.
The overall theme of this year’s conference is How Medicaid, Medicare, and Other Publicly Sponsored Programs Are Shaping the Future of Healthcare in a Time of Crisis. HMA will also host a pre-conference workshop on Sunday, October 9, on important trends and developments in value-based care.
HMA’s last national conference brought together 500 executives from health plans, providers, state and federal government, community-based organizations and others serving Medicaid, Medicare, and other vulnerable populations. Sponsorships and group discounts are available. For additional information, contact Carl Mercurio.
Confirmed speakers to date include (in alphabetical order):
Keynote Address: Politics and the ‘New Normal’ for U.S. Healthcare
Drew Altman, President and CEO, Kaiser Family Foundation
Keynote Q&A: State Medicaid Priorities, Challenges – Now and After the Public Health Emergency
Jacey Cooper, Medicaid Director, Chief Deputy Director, California Department of Health Care Services
Allison Matters Taylor, Medicaid Director, Indiana
Dave Richard, Deputy Secretary, North Carolina Medicaid
Jami Snyder, Director, Arizona Health Care Cost Containment System
Keynote Q&A: Key Strategies, Opportunities, and Concerns for Medicaid Managed Care
John Barger, National VP, Dual Eligible and Medicaid Programs, Humana, Inc.
Aimee Dailey, President, Medicaid, Anthem, Inc.
Rebecca Engelman, EVP, Medicaid Markets, AmeriHealth Caritas
Brent Layton, President, COO, Centene Corporation
Kelly Munson, President, Aetna Medicaid
Timothy Spilker, CEO, UnitedHealthcare Community & State
Featured Speakers
Michael Brodsky, MD, Medical Director, Behavioral Health and Social Services, L.A. Care Health Plan
Daniel Elliott, MD, Medical Director, Christiana Care Quality Partners, eBrightHealth ACO, ChristianaCare Health System
Andrew Martin, National Director of Business Development (Housing+Health), UnitedHealth Group
Martin Lupinetti, President, CEO, HealthShare Exchange (HSX)
Todd Rogow, President, CEO, Healthix
Jim Sinkoff, Deputy Executive Officer, CFO, SunRiver Healt
Tim Skeen, Senior Corporate VP, CIO, Sentara Healthcare
Mark Sasvary, Chief Clinical Officer, CBHS, IPA, LLC
Debra Sanchez-Torres, Senior Advisor, Centers for Disease Control and Prevention
Joshua Traylor, Senior Director, Health Care Transformation Task Force
Courtnay Thompson, Market President, Select Health of SC, an AmeriHealth Caritas Company
Amanda Van Vleet, Associate Director, Innovation, NC Medicaid Strategy Office, North Carolina Department of Health & Human Services
Shannon Wilson, VP, State Markets East, Priority Health
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
- Connecticut SNP Membership at 79,761, Mar-22 Data
- District of Columbia SNP Membership at 12,334, Mar-22 Data
- Georgia SNP Membership at 239,246, Mar-22 Data
- Iowa SNP Membership at 25,083, Mar-22 Data
- Ohio SNP Membership at 135,804, Mar-22 Data
- Pennsylvania SNP Membership at 207,704, Mar-22 Data
- Rhode Island SNP Membership at 10,222, Mar-22 Data
- Tennessee SNP Membership at 135,331, Mar-22 Data
- Utah SNP Membership at 15,097, Mar-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama Medicaid Recovery Audit Contractor RFP, May-22
- Florida Medicaid Managed Care Re-Procurement RFI, May-22
- Maryland Minimum Data Set and Long Term Care Planning Consultant RFP, May-22
- Maryland MMIS-II Support and Maintenance Resources RFP, Mar-22
- Missouri HealthNet Managed Care RFP, Awards and Evaluation, 2021-22
- New Hampshire Electronic Infectious Disease Surveillance System RFP, Mar-22
- Ohio Benefits System Maintenance and Operation Services RFP, May-22
Medicaid Program Reports, Data and Updates:
- Missouri HealthNet Managed Care External Quality Review Reports, 2015-21
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, Apr-22
- Tennessee External Quality Review Organization Technical Reports, 2016-21
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
About HMA
HMA is an independent, national research and consulting firm specializing in publicly funded healthcare and human services policy, programs, financing, and evaluation. We serve government, public and private providers, health systems, health plans, community-based organizations, institutional investors, foundations, and associations. Every client matters. Every client gets our best. With more than 20 offices and over 500 multidisciplinary consultants coast to coast, our expertise, our services, and our team are always within client reach.
Among other services, HMA provides generalized information, analysis, and business consultation services to investment professionals; however, HMA is not a registered broker-dealer or investment adviser firm. HMA does not provide advice as to the value of securities or the advisability of investing in, purchasing, or selling particular securities. Research and analysis prepared by HMA on behalf of any particular client is independent of and not influenced by the interests of other clients.
