HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Congress Sets Date for Medicaid “Unwinding”: What Now?

- Multiple Industry Experts to Lead Sessions at HMA's Healthcare Quality Conference

- Arizona Medicare Plan Receives $60 Million Investment from Chicago Pacific Founder to Launch ESRD C-SNP

- California Revises List of Medicaid Managed Care Award Winners in Several Counties

- Connecticut Expands Medicaid Eligibility for Children Effective January 1

- Florida Appoints Jason Weida as Interim Secretary

- Georgia Releases RFQC for Medicaid Managed Care Plans

- Georgia Establishes State Exchange Directing Buyers to Brokers, Insurers

- Idaho Legislators to Review Medicaid Expansion

- Maine to Seek Renewal of Waivers for Adults in Need of Home and Community-based Services

- Maryland Releases Behavioral Health ASO RFP

- Maryland Implements Medicaid Comprehensive Dental Coverage

- Massachusetts Selects 20 Community Partners for ACO Behavioral Health, LTSS

- Nevada Receives Federal Approval for SUD Treatment Waiver

- New Hampshire Legislature to Vote on Reauthorization of Medicaid Expansion Funding

- New York Governor Announces $1 Billion Plan to Address Behavioral Health

- North Dakota Releases Medicaid Enterprise Technical Systems Integrator RFP

- Oklahoma Faces Lawsuit from Provider-led Entity Regarding Managed Care Procurement

- Oregon Approves Amazon Acquisition of One Medical

- Rhode Island Releases NEMT Program RFQ

- Wisconsin Names Jamie Kuhn as Medicaid Director

- HHS Extends Public Health Emergency Until April 11

- CMS Allows States, Medicaid Plans to Spend 5 Percent of Premiums on Social Determinants of Health

- CVS Health Considers Acquisition of Oak Street Health

In Focus
Congress Sets Date for Medicaid “Unwinding”: What Now?
This week, our In Focus section reviews changes to Medicaid’s COVID-19 Public Health Emergency (PHE) unwinding. People enrolled in the Medicaid program have been continuously enrolled for almost three years, but that situation is about to change. In December 2022, Congress passed and the President signed into law a massive compromise bill to fund the government. It includes an important change to Medicaid’s continuous enrollment policy, which has been in effect since the early days of the COVID-19 PHE in March 2020.
Congress passed the Families First Coronavirus Relief Act (FFCRA) in March 2020. This legislation has allowed states to receive a 6.2 percentage point increase in their federal matching rate for Medicaid. As a condition for receiving the enhanced funding, states have been prohibited from disenrolling individuals who were otherwise determined ineligible for Medicaid. As a result, nearly 20 million more people are now enrolled in the Medicaid program.
The 2023 spending bill severs the link between the COVID-19 PHE declaration, the continuous enrollment requirement, and the higher federal match rate. The new law:
- Ends the Medicaid continuous coverage policy on March 31, 2023, even if the PHE declaration remains in effect. States may begin issuing terminations of ineligible individuals as early as February 1, with an effective date of April 1.
- Phases down the 6.2 percentage point increase in the federal matching rate rather than ending it abruptly at the end of the PHE as required under the FFCRA. Specifically, the increase will drop to 5 percentage points in April−June 2023, 2.5 percentage points in July−September 2023, and 1.5 percentage points in October−December 2023.
- Does not end the PHE or other flexibilities linked to the PHE.
Congress also added new parameters and reporting requirements for states as they resume annual eligibility renewals with coverage cancellation for individuals who no longer qualify. These requirements are in addition to data the Centers for Medicare & Medicaid Services (CMS) previously directed states to report. For example:
- States must maintain up-to-date enrollee contact information for individuals who will undergo an eligibility redetermination.
- States cannot disenroll individuals based only on returned mail.
- Prior to disenrolling an individual, the state must make a “good faith effort” to contact the person using more than one communication mode.
- States must submit to CMS “on a timely basis” a report explaining their eligibility redetermination activities.
- States must submit data related to individuals whose eligibility information was transferred between Medicaid and the Marketplace, with some exceptions for states that have integrated Medicaid and Marketplace eligibility systems and those that use the Federally Facilitated Marketplace.
Beyond the “Delinking”
The new law includes other important eligibility-related policies that may affect state and stakeholder planning for what is often referred to as the “unwinding” of continuous enrollment. Notably, the state Medicaid and CHIP programs will now be required to provide 12 months of continuous coverage for children. A total of 24 states already have adopted the 12-month continuous eligibility option for all children enrolled in Medicaid. While the new requirement will not take effect until January 1, 2024, additional states could adopt this option as they resume normal eligibility operations.
In addition, the new law makes permanent the option for states to extend Medicaid postpartum coverage to 12 months, up from 60 days. The one-year postpartum coverage option initially was approved in the American Rescue Plan but for a limited period of five years. Making the option permanent provides more certainty for states. Nearly two-thirds of states have already implemented or are planning to implement the 12-month postpartum coverage extension.
What Happens Next?
The definitive end date for the continuous enrollment policy sets in motion certain federal and state actions and the process for unwinding. On January 5, 2023, CMS published its first guidance to states on processes related to the new unwinding date. The agency is developing additional guidance and will use other communication tools to provide states with greater clarity on the new statutory reporting, matching rate, and federal agency expectations and oversight.
State plans: All states must submit unwinding plans to CMS by February 15; however, February 1 is the deadline for states that intend to begin renewals in February. These proposals must provide details regarding unwinding strategies, the timeline for starting enrollee renewals, and the pace of ongoing renewal processes. The specific end date for the continuous enrollment policy is driving more states to review and finalize their initiatives and engage with stakeholders.
Impact on health plans and providers: The unwinding process will create important decision points and considerations for Medicaid health plans and providers that have members and patients whom the unwinding process may affect in the next 12-18 months. The law’s requirements reinforce the imperative for states, Medicaid health plans, providers, and other partners to renew efforts to confirm enrollee contact information. The unwinding all will create new considerations for Medicaid health plans with respect to enrollee support, case mix, and rate setting issues.
State budgets and legislation: Many states will kick off their legislative sessions this month. The unwinding process—especially the phase-out of higher federal funding—has important implications for state budgets. State legislatures also may address the new continuous eligibility requirements for children and the permanent option for 12 months of postpartum coverage. As a result, Medicaid will likely remain a top priority during upcoming legislative sessions.
Federal oversight and enforcement: The law’s enhanced reporting provision is intended to provide safeguards to ensure eligible individuals remain enrolled in Medicaid. The reporting also focuses on data related to identifying and directing individuals likely to be eligible for the Marketplace program. Although CMS must publicly report these data, the agency has offered no specific timeline for posting the information. Notably CMS has oversight tools and may impose financial penalties on states that are noncompliant with the unwinding requirements.
Forthcoming federal guidance will confirm the parameters for state unwinding actions, CMS’s plans for oversight of state work, and how these efforts affect current Medicaid enrollees. Medicaid partners should closely monitor state level actions, including announcement of state unwinding plans and opportunities for collaboration. Earlier blogs describe the strategies and actions HMA is working with states and partners to undertake as they prepare for this significant change in Medicaid eligibility policies.
Please contact HMA experts Beth Kidder, Jane Longo, Michael Cohen, and Andrea Maresca with questions and for more information.
Multiple Industry Experts to Lead Sessions at HMA's Healthcare Quality Conference
A Deep Dive on What’s Next for Patients, Providers, Payers, and Policymakers
Monday, March 6, 2023
Fairmont Chicago, Millennium Park
Speakers from Arizona Medicaid, Intermountain Healthcare, Commonwealth Care Alliance, Council on Quality and Leadership, United Hospital Fund, Others to Join HMA Quality Conference
Here are some of the healthcare quality experts who will offer hands-on learning and insights at HMA’s Healthcare Quality Conference.
- Gregory Poulsen, SVP, Intermountain Healthcare, will speak on Next Steps in Positioning Your Organization for Continuous Quality Improvement.
- Mary Kay Rizzolo, CEO, Council on Quality and Leadership; Donna Martin, senior director for state partnerships and innovation, ANCOR; and Kathy Carmody, CEO, Institute on Public Policy for People with Disabilities, will lead The Final Frontier: Bringing State Intellectual and Developmental Disability Service Systems into the Quality Conversation.
- Oxiris Barbot, MD, CEO, United Hospital Fund, will help lead Identifying and Addressing Roadblocks to Healthcare Quality Improvement
- Jami Snyder, director, Arizona Health Care Cost Containment System; and Elizabeth Tobin-Tyler of Brown University School of Public Health will lead Practical Approaches to Addressing Equity and Social Determinants of Health.
- Justin Ley, CEO, Reema Health, will help lead Quality Innovations: Healthcare Disrupters that Are Driving Improved Outcomes.
- Nazlim Hagmann, MD, SVP, associate chief medical officer, Commonwealth Care Alliance, will help lead Developing a Behavioral Health Quality Strategy.
Register Now
View Agenda
Sponsorships and group discounts are available.
For additional information, contact Carl Mercurio
HMA Roundup
Alaska
Alaska Processes 54 Percent of Medicaid Applications on Time. The Anchorage Daily News reported on January 6, 2023, that only 54 percent of Medicaid applications in Alaska were processed on time since July 2022, and the current wait time is 90 to 120 days, according to figures from the Department of Health. State law requires applications to be processed in 30 days. Read More
Arizona
Arizona Medicare Plan Receives $60 Million Investment from Chicago Pacific Founder to Launch ESRD C-SNP. Arizona-based Medicare Advantage plan Gold Kidney Health Plan announced on December 27, 2022, that it has received a $60 million investment from Chicago Pacific Founder, an investment adviser that manages private equity funds. Gold Kidney will use the funds to launch an End Stage Renal Disease/Dialysis (ESRD) Medicare Advantage Chronic Special Needs Plan (C-SNP) for Medicare beneficiaries living in Maricopa, Pinal, and Gila counties in 2023. Read More
California
California Governor Proposes $10 Billion for CalAIM in Fiscal 2024 Budget. California Governor Gavin Newsom released on January 10, 2023, his fiscal 2024 budget proposal, which includes $10 billion for California Advancing and Innovating Medi-Cal (CalAIM), $8 billion for mental and behavioral health services, $6.1 billion to implement the Behavioral Health Community-Based Continuum Demonstration, and $844.5 million to continue expanding Medi-Cal to all income eligible Californian’s regardless of immigration status. Read More
California Senate Health Committee Chair to Focus on Expanding Mental Health Services, Providing Housing for Homeless. Kaiser Health News reported on January 6, 2023, that California state Senator Susan Talamantes Eggman (D-Stockton), the new chair of the Senate Health Committee, is focusing on expanding mental health services and providing housing and treatment services for homeless individuals. Eggman has also said she would consider a higher minimum wage for hospital workers to address workforce shortages. Read More
California Revises List of Medicaid Managed Care Award Winners in Several Counties. The California Department of Health Care Services announced on December 30, 2022, that it has cancelled the Medi-Cal Managed Care commercial contracts RFP and has entered into an agreement which revises the list of Medicaid managed care plans which will be contracted to operate in several of the state’s counties. Centene/Health Net Community Solutions will now operate under contracts in Los Angeles and Sacramento counties, but not San Diego. Health Net will subcontract to Molina for 50 percent of the Los Angeles membership under this agreement. Molina will remain a contractor in San Diego, but will no longer be the direct contractor in Los Angeles County. Anthem, Health Net and Molina will remain as contractors in Sacramento County. Anthem will replace Health Net as the commercial health plan in Kern County. In the state’s original award announcement last year, Centene failed to win contracts in Los Angeles, Sacramento and Kern counties. Additionally, after being excluded from the original awards, Community Health Group Partnership Plan and Blue Shield of California Promise Health Plan will continue to operate in San Diego. The original awards were protested by several plans. The revised agreement was made in conjunction with five of the state’s Medicaid plans: Anthem, Blue Shield of California Promise Health Plan, Community Health Group Partnership Plan, Centene, and Molina. Contracts are scheduled to begin in January 2024. Read More
Connecticut
Connecticut Expands Medicaid Eligibility for Children Effective January 1. The CT Mirror reported on January 10, 2023, that Connecticut expanded Medicaid eligibility to children 12 years and younger with household incomes up to 201 percent of federal poverty regardless of immigration status, effective January 1, 2023. Children who enroll before age 12 are able to keep the benefit through age 19. The state is expecting 5,500 newly eligible individuals to enroll in 2023. Read More
Florida
Florida Representative Introduces Amendment to Expand Florida Healthy Kids Eligibility. The Capitolist reported on January 5, 2023, that Florida Representative Robin Bartleman (D-Weston) filed a bill amendment that would expand eligibility for the Florida Healthy Kids and Kidcare Programs to 250 percent of federal poverty. The current income eligibility limit for the programs, which aim to provide coverage to children whose families do not qualify for Medicaid, is 200 percent of federal poverty.
Florida Appoints Jason Weida as Interim Secretary. Health News Florida reported on January 5, 2022, that Florida has appointed Jason Weida interim director of the state Agency for Health Care Administration (AHCA), following the departure of Simone Marstiller. Weida most recently served as AHCA chief of staff. Read More
Georgia
Georgia Releases RFQC for Medicaid Managed Care Plans. The Georgia Department of Community Health released on January 3, 2023, a request for statements of qualifications from Medicaid managed care plans for the state’s Georgia Families and Georgia Families 360 program. Responses to the Request for Qualified Contractors (RFQC) are due on February 7 and evaluation results will be published four to five weeks after. The Medicaid managed care request for proposals is expected to be released in early 2023. Read More
Georgia Establishes State Exchange Directing Buyers to Brokers, Insurers. GPB News reported on December 30, 2022, that Georgia established a state health insurance Exchange called Georgia Access, which directs individuals to brokers and health insurance company websites. Individuals can still purchase Exchange coverage using the federal HealthCare.gov website. The state’s initial plan to exit HealthCare.gov was rejected by federal regulators. Georgia Access does not provide a link to HealthCare.gov. Open enrollment ends on January 15. Read More
Idaho
Idaho Legislators to Review Medicaid Expansion. KTVB7 reported on January 10, 2023, that Idaho legislators will review the cost and impact of the state’s Medicaid expansion in accordance with state law to determine if the program should remain in effect. The review must be completed by January 31. Idaho voters approved Medicaid expansion in 2018. Read More
Illinois
Illinois Passes Bill Adding Definition of Rural Emergency Hospitals. Health News Illinois reported on January 11, 2023, that Illinois lawmakers approved a healthcare proposal that adds the definition of rural emergency hospitals, consistent with the new provider classification established under the Consolidated Appropriations Act of 2021. The proposal also expands those able to provide applied behavior analysis to autistic individuals, extends an existing fee waiver for healthcare providers to include podiatrists, and allows county nursing homes to participate in the nursing home tax and assessment. Read More
Iowa
Iowa to Merge Departments of Human Services, Public Health, Aging into Single Department. The Victoria Advocate reported on January 4, 2023, that the Iowa departments of human services, public health, and aging will be merging into one department, the Iowa Department of Health and Human Services. State lawmakers began the process in 2022 by establishing a framework and will continue the work during the current session. The merger is scheduled to happen on July 1. Read More
Kansas
Kansas Submits Extension Request for KanCare Section 1115 Waiver. The Centers for Medicare & Medicaid Services announced on January 5, 2023, that Kansas submitted a five-year extension request for its KanCare Section 1115 waiver. The state is asking to continue existing federal flexibilities, including 12 months of continuous eligibility for certain low-income parents or caretaker adults, federal Medicaid funds for services provided in institutes for mental disease, and continuous eligibility for children enrolled in KanCare under the Children’s Health Insurance Program who turn 19 during the public health emergency. The extension will run from January 1, 2024, through December 31, 2028. The federal comment period is open until February 4. Read More
Louisiana
Louisiana Governor Attributes Drop in Uninsured Rate to Medicaid Expansion. Louisiana Governor John Bel Edwards said on January 10, 2023, that the state’s uninsured rate fell from 22.7 percent before Medicaid expansion to 9.4 percent in the first seven years of expansion. Read More
Maine
Maine to Seek Renewal of Waivers Serving Adults in Need of Home and Community-based Services. The Maine Department of Health and Human Services announced on December 30, 2022, it is planning to seek federal approval to renew its Elderly and Adults with Disabilities waiver, known in Maine as Section 19, Home and Community Benefits for the Elderly and Adults with Disabilities. The state is also planning to seek renewal of its Adults with Other Related Conditions waiver, known in Maine as Section 20, Home and Community Based Services for Adults with Other Related Conditions. Public comments for both renewals will be accepted through January 30. Read More
Maryland
Maryland Releases Behavioral Health ASO RFP. The Maryland Department of Health (MDH) released on January 11, 2023, a request for proposals (RFP) for an administrative services organization (ASO) for the state’s public behavioral health system. The contract will run for five years, with one, two-year renewal option. UnitedHealth/Optum currently holds the behavioral health ASO contract in the state, which serves roughly 240,000 individuals who receive specialty mental health services and 100,00 who receive substance use disorder treatment. Proposals are due by March 16, 2023. Read More
Maryland Implements Medicaid Comprehensive Dental Coverage. The Avenue News reported on January 10, 2023, that approximately 800,000 Maryland Medicaid enrollees gained access to comprehensive dental coverage, effective January 1, 2023. Read More
Massachusetts
Massachusetts Selects 20 Community Partners for ACO Behavioral Health, LTSS. Healthcare Innovation reported on January 3, 2023, that Massachusetts has selected 20 organizations to participate in the state’s community partners program, which works with MassHealth Medicaid accountable care organizations (ACOs) to provide behavioral health and long-term services and supports (LTSS). The state reported fewer emergency room visits and lower costs through the first three years of the community partners program. Read More
Michigan
Michigan Implements New Medicaid Dental Reimbursement Methodology. State of Reform reported on January 6, 2023, that the Michigan Department of Health and Human Services implemented a new Medicaid dental reimbursement methodology on January 1. The new methodology, which still requires federal approval, sets Medicaid dental fee screens at the average commercial rate. A Medicaid dental payment rate increase for ambulatory surgical centers and outpatient hospitals was effective in November. Read More
Montana
Montana Lawmakers to Focus on Raising Medicaid Reimbursement Rates for Nursing Homes During Legislative Session. Modern Healthcare reported on January 9, 2023, that Montana lawmakers will focus on raising Medicaid reimbursement rates for nursing homes during the current legislative session. They will also discuss expanding telehealth services, restoring 12-month continuous eligibility for adult Medicaid beneficiaries, increasing the availability of behavioral health services, providing funding for Montana State Hospital, and increasing hospital oversight. Read More
Nebraska
Nebraska Hospitals Seek 9.6 Percent Medicaid Reimbursement Rate Hike in 2023. KMTV reported on January 2, 2023, that the Nebraska Hospital Association is calling for a 9.6 percent Medicaid reimbursement rate increase in 2023 and a 7.7 percent increase in 2024. The rate of increase was two percent in 2021 and 2022. The association attributed the need for higher rates to rising costs. Read More
Nevada
Nevada Receives Federal Approval for SUD Treatment Waiver. The Nevada Department of Health and Human Services announced on January 9, 2023, federal approval of the state’s Treatment of Opioid Use Disorders and Substance Use Disorders (SUDs) Transformation Project 1115 waiver request. The wavier, effective from January 1, 2023, through December 31, 2027, covers Medicaid services for individuals receiving SUD treatment in an institution for mental diseases. Read More
New Hampshire
New Hampshire Legislature to Vote on Reauthorization of Medicaid Expansion Funding. WCAX reported on January 2, 2023, that the New Hampshire legislature will vote on whether or not to reauthorize funding for Medicaid expansion. The state expanded Medicaid through a waiver called the New Hampshire Granite Advantage Program. The state pays 10 percent or $35 million to $39 million biannually of the cost of expansion, while the federal government covers the other 90 percent. The last time expansion funding was approved was in 2018. Read More
New Mexico
New Mexico Health Plan May Still Participate in State Medicaid Managed Care Procurement. The Corrales Comment reported on January 10, 2023, that Centene/Western Sky Community Care is not precluded from participating in the New Mexico Medicaid managed care procurement, following a settlement with the state over improper pharmacy billing. The company has not commented on whether it submitted a bid by the December 5 deadline. Western Sky has served the New Mexico Medicaid population since 2019. Read More
New York
New York Governor Announces $1 Billion Plan to Address Behavioral Health. The New York Times reported on January 10, 2022, that New York will dedicate roughly $1 billion to behavioral health, according to Governor Kathy Hochul’s State of the State address. The plan will reopen more than 800 inpatient psychiatric beds that were closed during the pandemic, create 3,500 hosing units with supportive services, expand mental health services in schools, and triple the capacity of community behavioral centers. Read More
New York Seeks Medicaid Matching Funds for Individuals in Institutions for Mental Disease. The Centers for Medicare & Medicaid Services announced on January 5, 2023, that New York submitted its Medicaid Redesign Team Section 1115 waiver amendment to federal regulators, seeking Medicaid matching funds for services delivered to individuals with a behavioral health diagnosis and residing in Institutions for Mental Diseases. The federal comment period will be open until February 4. Read More
North Carolina
North Carolina Reaches Settlement After Allegedly Disenrolling Medicaid Beneficiaries Without Properly Reviewing Applications. North Carolina Health News reported on December 21, 2022, that the North Carolina Department of Health and Human Services reached a settlement agreement with the Charlotte Center for Legal Advocacy, which filed a federal class action lawsuit alleging that the state disenrolled Medicaid beneficiaries without properly reviewing their applications. The lawsuit was originally filed in November 2017. There will be a hearing on January 13, 2023, to approve or deny the settlement agreement. Read More
North Dakota
North Dakota Extends Postpartum Medicaid Coverage from 60 Days to 12 Months. North Dakota Health and Human Services announced on January 6, 2023, that postpartum Medicaid coverage is extended from 60 days to 12 months, effective January 1. An estimated 250 individuals per year will benefit from the extended coverage. Read More
North Dakota Releases Medicaid Enterprise Technical Systems Integrator RFP. The North Dakota Department of Human Services released on January 3, 2023, a request for proposals (RFP) for a Medicaid Enterprise Technical Systems Integrator. The state is looking to modernize existing integration platforms, implement modern integration, and identify and access management capabilities. Responses are due on March 3, and awards will be announced the week of September 18. The contract is anticipated to begin on October 2. Read More
Oklahoma
Oklahoma Faces Lawsuit from Provider-led Entity Regarding Managed Care Procurement. The Tulsa World reported on January 10, 2023, that a group of Oklahoma health care providers filed a state lawsuit against the Oklahoma Health Care Authority (OHCA), alleging it did not give preferential treatment to local providers during its recent Medicaid managed care procurement, as was required by state law. The newly formed Equity Group Advancing Access and Services is asking the court to force the state to redo the procurement. Read More
Oklahoma Requests Five-year Extension of SoonerCare Section 1115 Waiver Program. The Centers for Medicare & Medicaid Services (CMS) announced on January 5, 2023, that Oklahoma requested a five-year extension of the SoonerCare Section 1115 waiver demonstration from January 2024 through December 2029. The demonstration, which would not undergo programmatic changes under the extension, covers the state’s Patient-Centered Medical Home program, health management program, health access networks, and employer sponsored insurance program. Public comments will be accepted through February 4, 2023. Read More
Oregon
Oregon Medicaid to Focus on Maintaining Coverage for Individuals After PHE Ends. KGW reported on January 10, 2023, that the Oregon Medicaid program will focus on maintaining coverage for beneficiaries following the end to the public health emergency (PHE), according to James Schroeder, newly appointed director of the Oregon Health Authority. Other priorities include implementing a waiver to increase services provided to homeless individuals; ensuring individuals can maintain coverage despite temporary changes in eligibility; improving the overall quality of life for residents; and developing behavioral health care services that are specific to each community. Read More
Oregon Approves Amazon Acquisition of One Medical. Fierce Healthcare reported on January 3, 2023, that Amazon’s proposed acquisition of primary care provider One Medical for $3.9 billion received approval from the Oregon Health Authority. The acquisition is still being reviewed by the Federal Trade Commission. One Medical has 188 medical clinics in 29 markets. Read More
Pennsylvania
Pennsylvania Senator to Reintroduce Bill Allowing Medicaid Coverage of Assisted Living. McKnights Senior Living reported on December 22, 2022, that Pennsylvania Senator Michele Brooks (R-New Castle) intends to reintroduce legislation that would allow Medicaid to reimburse assisted living communities. The bill is aimed at preventing residents from being transitioned to nursing homes when they can no longer afford assisted living care. There are currently 67 assisted living communities in the state. Read More
Pennsylvania Medicaid Plan Improperly Denied Pediatric Skilled Nursing Services, Federal Audit Finds. The Philadelphia Inquirer reported on December 21, 2022, that Pennsylvania Medicaid plan AmeriHealth Caritas/Keystone First improperly denied claims from one in five children for overnight skilled nursing services, according to an audit by the U.S. Office of the Inspector General (OIG). Keystone denied 2,482 requests for pediatric skilled nursing services during 2018 and 2019, and auditors found that 10 of the 50 denials should have been at least partially approved. Read More
Rhode Island
Rhode Island Requests Five-Year Extension of Comprehensive Section 1115 Waiver Demonstration. The Centers for Medicare & Medicaid Services (CMS) announced on January 6, 2023, that Rhode Island submitted a request to extend the state’s Section 1115 waiver demonstration, which covers the entire Medicaid program, effective January 2024 through December 2028. The extension would build on existing demonstration elements to cover housing stabilization and support programs, health equity initiatives, and pre-release supports for incarcerated individuals. Public comments will be accepted through February 5, 2023. Read More
Rhode Island Releases NEMT Program RFQ. The Rhode Island Department of Administration/Division of Purchases released on December 28, 2022, a request for qualifications (RFQ) for one vender to provide Medicaid non-emergency medical transportation (NEMT) services. The NEMT program serves eligible Medicaid beneficiaries and residents over the age of 60 who qualify under the elderly transportation program. The initial contract will run from July 1, 2023, through June 30, 2026, with four one-year options. Responses are due on February 17. The current incumbent is MTM. Read More
Tennessee
Tennessee Plan May Have Received $5.9 Million in MA Overpayments for High-Risk Diagnoses, Federal Audit Finds. Health Payer Intelligence reported on January 5, 2023, that Cigna-HealthSpring of Tennessee may have received $5.9 million in Medicare Advantage (MA) overpayments from 2016 to 2017 for high-risk diagnoses that were not supported by medical records, according to an audit by the U.S. Office of the Inspector General. The report said it took into consideration Cigna’s claims that the audit was biased, as it did not account for underpayment. Read More
Texas
Texas Legislators to Consider Several Maternal Health Bills. KERA reported on January 9, 2023, that Texas lawmakers are expected to consider legislation regarding extended postpartum coverage, Medicaid-covered doula services, maternal mortality data updates, and cultural competency education for physicians. The next legislative session begins on January 10. Read More
Texas Requests Public Comments on Best Value Criteria for STAR Kids Procurement. Texas Health and Human Services released on December 19, 2022, a request for public comments regarding the proposed Best Value Criteria the agency will use in awarding the STAR Kids managed care contract during the next procurement. Comments will be accepted through January 25. The STAR Kids request for proposals is anticipated to be released between December 2023 and February 2024. Read More
Wisconsin
Wisconsin Names Jamie Kuhn as Medicaid Director. Wisconsin Health News reported on January 11, 2023, that Jamie Kuhn was named state Medicaid director, after the departure of Lisa Olson at the end of 2022. Kuhn previously served as external affairs director for the office of Governor Tony Evers. Read More
Wisconsin Organizations Are Awarded $5 Million in Mental Health Grants. Wisconsin Health News reported on January 11, 2023, that the U.S. Department of Health and Human Services awarded Wisconsin organizations $5 million in grants for mental health services. Milwaukee Public Schools was awarded $2.9 million, and Lac Courte Oreilles Band of Lake Superior Chippewa Indians was awarded $973,000 for school-based mental health programs and services. Four Wisconsin organizations were each awarded $250,000 for training on recognizing mental health challenges for early intervention. Read More
Wisconsin Governor Calls for Medicaid Expansion. The Associated Press reported on January 4, 2023, that Wisconsin Governor Tony Evers called for Medicaid expansion during his second inaugural address. In February, Evers is expected to release a two-year state budget plan showing a projected $6.6 billion surplus. Read More
Wyoming
Wyoming Legislature to Consider Medicaid Expansion Bill. The Casper Star-Tribune reported on January 6, 2023, that Wyoming lawmakers will consider another Medicaid expansion bill during the 2023 session. The Wyoming Legislature Joint Revenue Committee advanced the bill in November 2022. Expansion would impact between 12,000 and 27,000 adults. Read More
Wyoming Receives Federal Certification for MMIS Provider Solution From HHS Technology Group. HHS Technology Group (HTG) announced on January 3, 2023, that the Wyoming Department of Health received federal certification for its Medicaid Provider Enrollment, Screening, and Monitoring system. The state is using HTG’s Discover your Provider, which is one of six certified Medicaid Management Information System (MMIS) provider solutions. Read More
National
15.9 Million Individuals Enroll in Exchange Coverage. The Centers for Medicare & Medicaid Services announced on January 11, 2023, that 15.9 million individuals have enrolled in coverage through the Exchanges since November 2022, which represents a 13 percent increase from last year. Open enrollment ends on January 15. Read More
HHS Extends Public Health Emergency Until April 11. U.S. Secretary of Health and Human Services (HHS) Xavier Becerra announced on January 11, 2023, the renewal of the public health emergency (PHE) until April 11. The PHE had previously been extended through January 13. Read More
States Expand Access to Telehealth Behavioral Health Services. Kaiser Family Foundation reported on January 11, 2023, that during the COVID-19 pandemic, states expanded telehealth access for behavioral health services by adding audio-only coverage of services, expanding the types of behavioral health services that can be delivered via telehealth, and expanding the provider types that may be reimbursed for telehealth delivery. The report notes that telehealth for behavioral services remains high. Read More
HHS Must Create Plan to Reimburse Hospitals for 340B Underpayments, Federal Judge Rules. Modern Healthcare reported on January 10, 2023, that the U.S. Health and Human Services Department must generate a plan to correct underpayments to hospitals in the wake of 340B program reimbursement cuts in 2018, according to a federal judge’s ruling. Previously, the U.S. Supreme Court ruled the payment cut was unlawful. Read More
ACOs Struggle to Integrate Medical, Social Services. Health Affairs reported on January 10, 2023, that accountable care organizations (ACOs) are struggling to integrate medical and social services, including social determinants of health. Barriers include lack of data on patient social needs and capabilities of potential community partners; lack of mature partnerships with community-based organizations; and challenges in measuring return on investment. Read More
States Seek to Address Medicaid Behavioral Health Workforce Shortages. Kaiser Family Foundation reported on January 10, 2023, that states hope to address Medicaid behavioral health workforce shortages by increasing reimbursement rates, reducing administrative burdens, adding new provider types, implementing telehealth flexibilities, and incentivizing provider participation. Read More
Medicaid Expansion States Saw 17 Percent Decrease in Postpartum Hospitalizations, Health Affairs Study Finds. Fierce Healthcare reported on January 9, 2023, that a study of Medicaid expansion states showed a 17 percent decline in postpartum hospitalizations following expansion, according to a Health Affairs study. The majority of the reduction in hospitalizations was found in the first 60 days postpartum, but the study also found evidence of reduced postpartum hospitalizations between 61 days and six months after birth. Read More
CMS Releases Resources for PHE Unwinding. The Centers for Medicare & Medicaid Services (CMS) released on January 6, 2023, a resource for managed care plans to utilize as states undergo the Medicaid and Children’s Health Insurance Program eligibility redetermination process after the COVID-19 continuous enrollment requirement sunsets. Additionally, CMS released a resource outlining the system readiness artifacts that states will need to submit at the end of the public health emergency (PHE). Read More
CMS Seeks MIPS Measurement Set Recommendations for 2024. South Florida Hospital News reported on January 4, 2023, that the Centers for Medicare & Medicaid Services (CMS) is seeking stakeholder recommendations for new or revised specialty measurement sets for the 2024 Merit-Based Incentive Payment System (MIPS). Recommendations must be submitted by February 13, 2023. Read More
CMS Allows States, Medicaid Plans to Spend Up to 5 Percent of Premiums on Social Determinants of Health. Modern Healthcare reported on January 4, 2022, that states and health plans can spend up to five percent of Medicaid premiums on nonclinical services like housing, nutrition, and transportation, according to guidance from the Centers for Medicare & Medicaid Services (CMS). Organizations that spend at least 1.5 percent on alternative benefits must report how it was determined that these benefits are cost-effective. Read More
Medicaid, CHIP, Medicare Enrollment Exceeds 144 Million in September 2022. The Centers for Medicare & Medicaid Services (CMS) announced on January 4, 2023, that Medicaid and Children’s Health Insurance Program (CHIP) enrollment approached 91 million in September 2022, an increase of more than 383,000 from August 2022. Medicare enrollment was 65 million, up nearly 161,000 from August 2022, with 30.1 million in Medicare Advantage or other plans. More than 12 million were dually eligible and are counted in the enrollment totals for both programs. Read More
Biden Signs Omnibus Appropriations Bill. Fierce Healthcare reported on January 2, 2023, that President Biden signed the $1.7 trillion Omnibus Appropriations bill, which permits states to begin Medicaid eligibility redeterminations on April 1, 2023, and extends Medicare telehealth flexibilities that were implemented during the COVID-19 pandemic through 2024, among other healthcare measures. Read More
MACPAC Reports Wide Variation in Medicaid Base Payments for Nursing Facilities. The Medicaid and CHIP Payment Access Commission (MACPAC) reported in January 2023, wide variation in Medicaid base payment rates for nursing facilities. While Medicaid base payments covered a median of 86 percent of nursing facility costs in 2019, MACPAC found that base payments made up less than 70 percent of costs in 15 percent of facilities and more than 100 percent of costs in 19 percent of facilities. Read More
U.S. DoD Awards TRICARE Managed Care Contracts to Humana, TriWest. The U.S. Department of Defense (DoD) announced on December 22, 2022, that it has awarded incumbent Humana Government Business a $70.9 billion contract for TRICARE managed care services for the U.S. east region and a $65.1 billion contract to TriWest Healthcare Alliance for the west region. The contracts, covering roughly 9.6 million beneficiaries, will run for nine years. Six states previously in the east region will transition to the west. Centene is the incumbent west region contract holder. Read More
Industry News
CVS Health Considers Acquisition of Oak Street Health. Health Payer Specialist reported on January 10, 2023, that CVS Health is considering the acquisition of Illinois-based Medicare provider Oak Street Health for more than $10 billion. Oak Street Health, which went public in 2020, focuses on Medicare patients with low incomes and chronic health problems through 169 centers across the country. Private equity firms General Atlantic and Newlight Partners own a collective 39 percent stake in the company. Read More
Humana, Centene Report Medicare Advantage Enrollment Gains. Modern Healthcare reported on January 9, 2023, that Humana reported 625,000 new enrollees in its Medicare Advantage plans, a 14 percent increase from the previous year. Centene said Medicare Advantage enrollment was slower than expected; however, it reported a “high teens” percent gain in Exchange enrollment. The two companies delivered the results at the J.P. Morgan Healthcare Conference in California. Read More
Amerigroup MD Changes Name to Wellpoint. Elevance Health announced on January 3, 2023, that its Amerigroup Maryland plan changed its name to Wellpoint, effective January 1. Read More
Help at Home Acquires Open Systems Healthcare Operations in PA, DE. Home care services provider Help at Home announced on January 3, 2023, that it has acquired Open Systems Healthcare’s home care operations in Pennsylvania and Delaware. The acquisition does not include Open Systems Healthcare’s service locations in the District of Columbia. Help At Home provides in-home, community-based care in 12 states. Read More
LCMC Health Acquires 3 HCA Healthcare Hospitals. Modern Healthcare reported on January 3, 2023, that LCMC Health completed its acquisition of three HCA Healthcare-owned hospitals in Louisiana for $150 million: Tulane Medical Center, Tulane Lakeside Hospital, and Lakeview Regional Medical Center. Read More
Fillmore Capital Partners Finalizes Agreement with OH-Based UC Health. Becker’s Hospital Review reported on December 30, 2022, that California-based private equity firm Fillmore Capital Partners has finalized an agreement to consult with management concerning operations at Ohio-based UC Health’s Daniel Drake Center for Post-Acute Care, a provider of long-term acute care. Read More
Justice Files Lawsuit Against AmerisourceBergen for Knowingly Distributing Opioids Later Resold Illegally. The New York Times reported on December 29, 2022, that the U.S. Justice Department filed a lawsuit accusing AmerisourceBergen of knowingly distributing opioids that were later illegally resold. The lawsuit was filed in conjunction with federal prosecutors in New Jersey, Colorado, Pennsylvania, and New York. Read More
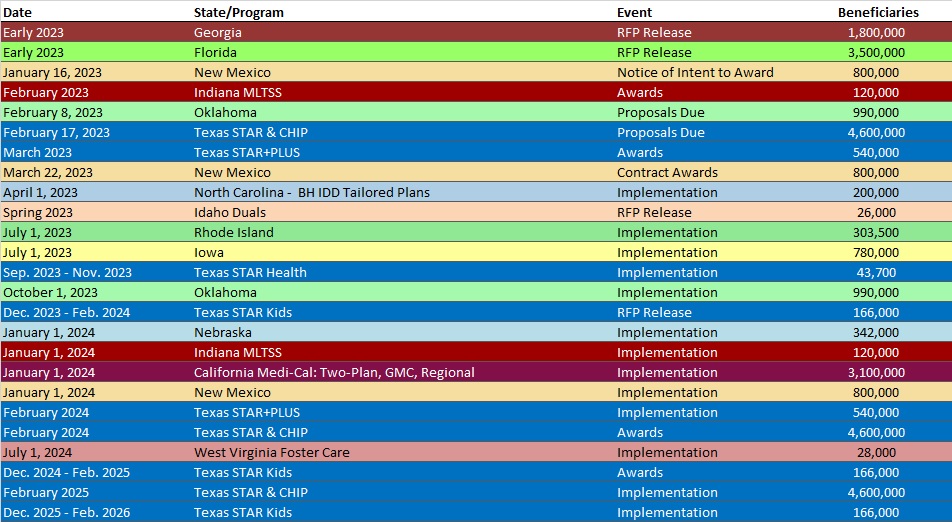
RFP Calendar
Company Announcements
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPERS
