This week's roundup:
- In Focus: HMA Community Strategies Conducts Evaluation for the City of Los Angeles FamilySource System

- Alabama Releases RFP for Medicaid Enterprise Data Services Solution

- Arizona Releases Strategic Roadmap to Modernize Medicaid Enterprise System

- Florida Medicaid Disenrollment Could Impact Up to 1.8 Million Households

- Florida Senate Committee Approves Bill to Place Restrictions on PBMs

- Georgia Senate Committee Misses Deadline, Imperiling Mental Health Bill

- Kentucky Governor Vetoes Bill that Would Block Expanded Dental, Vision, Hearing Benefits for Medicaid Beneficiaries

- Louisiana Governor Proposes $196 Million for Medicaid Redeterminations Process

- New York Providers File Lawsuit to Delay Transition of Medicaid Pharmacy Benefits from Managed Care to FFS

- North Carolina Enacts Medicaid Expansion

- Tennessee Legislature Considers Bill to Block State from Contracting with Medicaid Plans Covering Gender-affirming Treatment in Any State

- Medicaid, CHIP Enrollment Tops 92.3 Million in December 2022

- Mosaic Dental Collective Partners with Audax Private Equity

- BCBS-NM Names Nancy Smith-Leslie as Vice President of Medicaid

In Focus
HMA Community Strategies Conducts Evaluation for the City of Los Angeles FamilySource System
This week, our In Focus section highlights a HMA Community Strategies program evaluation of the City of Los Angeles FamilySource System (FSS). Systemic health disparities have exposed Los Angeles’ racially and ethnically diverse populations to increased risks of economic hardship, educational underachievement, and housing instability. To better understand this imbalance and drive toward change, the City of Los Angeles, through Community Development Block Grants (CDBG), Community Service Block Grants (CSBG) and General Funds established the FamilySource System, a place-based program, to address disparities, prevent and alleviate poverty, increase equity, and better coordinate support for these communities. The purpose of the FSS is to provide a myriad of braided social, educational, work and family support services designed to assist low-income families to become more self-sufficient by increasing family income and academic achievement for youth and adults.
HMA Community Strategies conducted this evaluation of the FamilySource System and economic impact study to identify key trends, barriers, and interventions that could better illuminate disparities in Los Angeles and move to greater income, education, and housing equity.
Contributions to this report were made by Charles Robbins, Megan Beers, Ryan Maganini, Matthew Ward, and Yamini Narayan.
HMA Roundup
Alabama
Alabama Governor Proposes Almost $34 Million for Expected CHIP Enrollment Increase. The Alabama Daily News reported on March 29, 2023, that Alabama Governor Kay Ivey’s proposed fiscal 2024 budget includes nearly $34 million in funding for a projected increase in enrollment in ALL Kids, the state Children’s Health Insurance Program (CHIP). All Kids enrollment, currently at nearly 70,000, is expected to increase by 15,000 to 20,000 in the next year, driven by Medicaid redeterminations. Read More
Alabama Releases RFP for Medicaid Enterprise Data Services Solution. The Alabama Medicaid Agency released on March 21, 2023, a request for proposals (RFP) for an Enterprise Data Services (EDS) solution as part of its future Medicaid Enterprise System (MES). The EDS vendor will deliver integrated data from disparate data sources, generate reports, perform analytics, and provide data visualizations. It will also provide business intelligence tools. The EDS solution will replace services currently under the Alabama Medicaid Management Information System (AMMIS). Read More
Arizona
Arizona Releases Strategic Roadmap to Modernize Medicaid Enterprise System. The Arizona Health Care Cost Containment System (AHCCCS) released on March 23, 2023, a strategic roadmap outlining project recommendations and considerations to modernize and assess the need to replace its Medicaid Enterprise System (MES). The roadmap will be prepared by NTT Data Services. AHCCCS and Med-QUEST Division, Hawaii’s Medicaid program, share an MES system. Read More
Connecticut
House Committee Advances Bill to Increase Medicaid Provider Reimbursement Rates. The Connecticut Mirror reported on March 24, 2023, that the Connecticut House Human Services Committee advanced a bill (House Bill 6685) to increase Medicaid provider reimbursement rates. The bill would increase rates to 70 percent of Medicare rates by June 2024 and 100 percent by June 2028. Read More
Florida
Florida to Submit Extension Request for Medicaid Section 1115 Family Planning Waiver. Florida Politics reported on March 28, 2023, that the Florida Agency for Health Care Administration plans to submit an extension request for its Medicaid Section 1115 Family Planning waiver, which covered more than 64,000 women as of fiscal 2020. The state is proposing spending of $10 million over the life of the waiver, with $1.98 million in fiscal 2024. Public meetings are scheduled for April 10 and 18, and comments will be accepted until April 26. Read More
Florida House Proposes $76 Million to Increase Medicaid Reimbursement Rates for Providers Who Treat Children. The Tampa Bay Times reported on March 28, 2023, that the Florida House budget includes a proposed $76 million to increase Medicaid reimbursement rates for providers who treat children. Lawmakers are also considering a bill to make families earning up to three times of poverty eligible for health coverage subsidies through KidCare. It is estimated that the bill would allow coverage for an additional 42,000 children. Read More
Senate Committee Approves Bill to Place Restrictions on PBMs. Health News Florida reported on March 28, 2023, that the Florida Senate Health Policy Committee approved a bill (SB 1550) to place restrictions on pharmacy benefit managers (PBMs), including preventing companies from requiring that patients use pharmacies affiliated with PBMs. The House Healthcare Regulation Subcommittee is scheduled to take up its version of the bill (HB 1509) next week. Read More
Medicaid Disenrollment Could Impact Up to 1.8 Million Households. The South Florida Sun Sentinel reported on March 26, 2023, that Medicaid disenrollments could impact up to 1.8 million Florida households with children when redeterminations begin. Income requirements are expected to cause about 900,000 disenrollments. An additional 850,000 Medicaid members have not updated their information. Children who lose coverage will be referred to Florida KidCare, a state-sponsored health insurance program with low monthly premiums. KidCare enrollment is expected to more than double from 114,000. Read More
Georgia
Senate Committee Misses Deadline, Imperiling Mental Health Bill. The Associated Press reported on March 23, 2023, the Georgia Senate Health and Human Services Committee missed a deadline to advance a mental health bill to the full Senate. A rewritten version of the bill, which passed out of the House (House Bill 520), will now require a two-thirds vote by the Senate to set aside rules and allow the bill to advance. Read More
Idaho
Idaho to Study State Medicaid Hospital Payments, Bankruptcy of Health Data Exchange. The Idaho Press reported on March 25, 2023, that the Idaho Joint Legislative Oversight Committee approved studies of the state’s hospital Medicaid payments and why the Idaho Health Data Exchange went bankrupt. The studies will be conducted by the Office of Performance Evaluations. The hospital Medicaid payment study will cover payment methodology and compare Idaho’s hospital Medicaid payment rates and spending to other states. Read More
Committee Advances Revised Fiscal 2024 Medicaid Budget Bill. The Idaho Capital Sun reported on March 22, 2023, that the Idaho legislature’s Joint Finance-Appropriations Committee (JFAC) advanced a revised Medicaid fiscal 2024 budget bill, with proposed funding reduced by $152 million to about $4.55 billion. The JFAC made the reduction after an earlier budget bill failed in the House. Read More
House Committee Will Not Hold Hearing on Postpartum Medicaid Extension Bill. Northern Rockies News Service reported on March 23, 2023, that the Idaho House Health and Welfare Committee will not hold a hearing on a bill (House Bill 201) to extend postpartum Medicaid coverage from 60 days to 12 months during the current session, according to chair John Vander Woude (R-Nampa). While he supports the bill, Vander Woude, said he wants the legislature to pass a Medicaid budget first. Read More
Illinois
Commission Approves Rules to Enforce Health Plan Network Adequacy Regulations. KTVI reported on March 22, 2023, that the Illinois Joint Commission on Administrative Rules has approved a set of rules for enforcing health plan network adequacy requirements. The rules clarify health plan requirements under the state’s Network Adequacy and Transparency Act. Read More
Iowa
House Republicans to Increase Medicaid Reimbursement Rates for Nursing Homes. Radio Iowa reported on March 23, 2023, that Republicans in the Iowa House are planning to increase Medicaid reimbursement rates for nursing homes. Governor Kim Reynolds has proposed a $15 million rate increase. Read More
Kentucky
Kentucky Governor Vetoes Bill that Would Block Expanded Dental, Vision, Hearing Benefits for Medicaid Beneficiaries. Kentucky Governor Andy Beshear vetoed on March 24, 2023, a bill (Senate Bill 65) that would block the expansion of dental, vision, and hearing benefits for adults on Medicaid. Beshear implemented the new benefits in October 2022. Read More
Louisiana
Louisiana Governor Proposes $196 Million for Medicaid Redeterminations Process. The Louisiana Illuminator reported on March 29, 2023, that Louisiana Governor John Bel Edwards proposed spending nearly $196 million for the Medicaid redeterminations process, including a promotional campaign; hiring new staff; and outreach efforts through hospitals, pharmacies, and not-for-profits organizations. The state is expecting up to 355,000 beneficiaries to lose coverage. Read More
Audit Points to Possible Improper Medicaid Behavioral Payments. NOLA reported on March 22, 2023, that the Louisiana Department of Health may have made $13 million in improper Medicaid behavioral health payments, according to a state audit. The audit looked at payments from 2015 to 2022. Read More
Montana
Providers Struggle with Low Medicaid Reimbursement Rates. Kaiser Health News reported on March 24, 2023, that health care providers in Montana are struggling financially due to low Medicaid reimbursement rates. The Montana Legislature is considering two separate bills that would increase rates. Read More
Nebraska
Senator Introduces Bill to Increase Medicaid Reimbursement Rates for Rural Behavioral Health Providers. KNOP reported on March 24, 2023, that Nebraska Senator Mike Jacobson (R-Lincoln) introduced a bill to increase Medicaid reimbursement rates for rural behavioral health providers. Other bills introduced were aimed more generally at increasing rural Medicaid reimbursement rates. Read More
Nevada
Nevada Senate Committee Holds Hearing on Bill to Provide Medicaid Coverage to Undocumented Individuals. The Nevada Current reported on March 29, 2023, that the Nevada Senate Committee on Health and Human Services held a hearing on a bill (Senate Bill 419) to expand Medicaid to undocumented individuals. Eight states and the District of Columbia currently provide Medicaid coverage for income-eligible children regardless of immigration status, with a few of the states extending the coverage to undocumented adults as well. Read More
New Hampshire
House Committee Considers Budget Amendment for $70 Million Increase in Medicaid Reimbursement Rates. The New Hampshire Bulletin reported on March 27, 2023, that the New Hampshire House Finance Committee is considering a budget amendment aimed at providing an additional $70.2 million over two years to increase Medicaid reimbursement rates. Governor Chris Sununu’s proposed budget includes a $34 million or 3.1 percent increase per year. Read More
New York
Providers File Lawsuit to Delay Transition of Medicaid Pharmacy Benefits from Managed Care to FFS. The Buffalo News reported on March 27, 2023, that New York community health providers Evergreen Health and Heritage Health and Housing filed a lawsuit seeking a temporary restraining order to halt the transition of the state’s Medicaid pharmacy benefit program from managed care back to fee-for-service. The transition is scheduled for April 1. The state Assembly and Senate also both advanced language in their budgets that would block the transition. Read More
North Carolina
North Carolina Enacts Medicaid Expansion. The Associated Press reported on March 27, 2023, that North Carolina Governor Roy Cooper signed a Medicaid expansion bill into law. The bill includes a provision that requires a separate state budget law to be enacted before expansion is implemented. Expansion is expected to impact about 600,000 individuals.
Ohio
Lawmakers to Reintroduce Bill to Allow Medicaid to Cover Doula Services. The Ohio Capital Journal reported on March 23, 2023, that a bipartisan bill will be introduced in the Ohio House and Senate to allow Medicaid coverage for doula services. The bill would also require the Department of Medicaid to release annual reports on outcomes related to doula services. The bill has been introduced in two previous sessions, but it was never passed by both chambers. Read More
Oklahoma
Oklahoma Extends Postpartum Medicaid Coverage. The U.S. Department of Health and Human Services announced on March 23, 2023, that Oklahoma received approval to extend postpartum Medicaid coverage from 60 days to 12 months. Oklahoma is the 30th state to receive approval to extend coverage. The extension will impact approximately 14,000 Oklahomans. Read More
Tennessee
Legislature Considers Bill to Block State from Contracting with Medicaid Plans Covering Gender-affirming Treatment in Any State. Modern Healthcare reported on March 27, 2023, that the Tennessee legislature is considering a bill that would prohibit the state from contracting with Medicaid plans that cover gender-affirming treatment for anyone in the country. If enacted, the state would have 30 days from the effective date to revise its Medicaid plan contracts. According to a state legislature budget analysis, the bill would impact plan choice, quality, and cost. Read More
Washington
Hospitals, Lawmakers Agree on Hospital Tax to Fund Medicaid Payment Increase. The Seattle Times reported on March 23, 2023, that Washington hospitals and state lawmakers reached an agreement on a provider tax aimed at increasing Medicaid reimbursement rates and bringing in $1 billion in additional federal matching funds. A bill for the proposed plan is expected to be introduced shortly. Read More
Wisconsin
Lawmakers Introduce Postpartum Medicaid Extension Bill. The Milwaukee Journal Sentinel reported on March 23, 2023, that Republican lawmakers in the Wisconsin legislature introduced a bill to extend postpartum Medicaid coverage from 60 days to 12 months. Nearly half of lawmakers have signed on to the bill, but it is not clear if it has enough votes to pass. Read More
Activists Push Lawmakers on Medicaid Expansion. The Wisconsin Examiner reported on March 23, 2023, that the Wisconsin Poor People’s Campaign held a rally at the state capitol to push lawmakers to expand Medicaid. Surveys have shown that approximately 70 percent of Wisconsin residents support expansion. Read More
National
Medicaid, CHIP Enrollment Tops 92.3 Million in December 2022. The Centers for Medicare & Medicaid Services (CMS) announced on March 28, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) topped 92.3 million in December 2022, an increase of more than 512,000 from November 2022. Medicare enrollment was nearly 65.5 million, up more than 116,000 from November 2022, including 30.3 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
House Panels Question HHS Secretary on Medicare Advantage Spending. CQ News reported on March 28, 2023, that House lawmakers on two panels questioned U.S. Department of Health and Human Services (HHS) Secretary Xavier Becerra on proposed spending increases for Medicare Advantage. Becerra defended the proposal from the Centers for Medicare & Medicaid Services in hearings before the House Appropriations Labor-HHS-Education subcommittee and the Ways and Means Committee. Read More
U.S. Representative Introduces Bill to Decrease Fraud in Medicaid, Medicare. Kaiser Health News (KHN) reported on March 28, 2023, that U.S. Representative Lloyd Doggett (D-TX) introduced a bill (HR 1745) that would give the Centers for Medicare & Medicaid Services (CMS) the authority to deactivate National Provider Identifiers (NPIs) tied to anyone convicted of waste, fraud, or abuse and whose name appears on the exclusions list kept by the Office of Inspector General. The bill would also require CMS to implement recommendations from the inspector general to improve NPI reporting and provider transparency. The bill comes after a KHN investigation found that people accused or convicted of fraud can still use NPIs to bill Medicare and Medicaid for services. Read More
U.S. Senate Committee to Hold Hearing on PBMs. CQ Health reported on March 27, 2023, that the U.S. Senate Finance Committee will hold a hearing on pharmacy benefit managers (PBMs). Last week, the Senate Commerce, Science and Transportation Committee advanced a bill that would impose more transparency requirements on PBMs and ban spread pricing. Read More
MACPAC Recommends Ownership Data be Collected for Medicare, Medicaid Facilities. The Medicaid and CHIP Payment and Access Commission (MACPAC) recommended on March 27, 2023, that private equity and real estate investment trust ownership data be collected for both Medicare and Medicaid-certified facilities. MACPAC made the recommendation in a comment letter to the Centers for Medicare & Medicaid Services (CMS) on a proposed rule that requires disclosure of nursing facility ownership information. The proposed rule currently only establishes a standard process for collecting ownership data for Medicare-certified nursing facilities, not Medicaid. MACPAC also supports future efforts to use the new ownership data to examine the effects of ownership on quality outcomes. Read More
CMS Extends Medicare Advantage Value-based Insurance Design Model through 2030. The Centers for Medicare & Medicaid Services (CMS) announced on March 23, 2023, that the Medicare Advantage Value-Based Insurance Design Model will be extended through 2030. The model will also introduce changes intended to more fully address the health-related social needs of patients, advance health equity, and improve care coordination for patients with serious illness. For 2023, there are 52 participants. Read More
Medicaid Lags on Primary Care Access for Children with Special Needs, MACPAC Finds. The Medicaid and CHIP Payment and Access Commission (MACPAC) reported on March 23, 2023, that children with special health care needs covered by Medicaid were less likely than those with private insurance to have a primary care provider, according to a MACPAC issue brief. The brief also found that children on Medicaid were more likely to have had an emergency room visit or hospitalization in the past 12 months. About one in five children have special health care needs, and over one third of them are covered by Medicaid. The brief used data from the 2018 and 2019 National Survey of Children’s Health. Read More
Industry News
Mosaic Dental Collective Partners with Audax Private Equity. Mosaic Dental Collective announced on March 28, 2023, a partnership with investment firm Audax Private Equity. Terms were not disclosed. Mosaic is a dental services organization supporting 49 affiliated dental offices in California and Washington. Read More
BCBS-NM Names Nancy Smith-Leslie as Vice President of Medicaid. The Albuquerque Journal reported on March 28, 2023, that Blue Cross Blue Shield of New Mexico named Nancy Smith-Leslie as its new vice president of Medicaid. Previously, Smith-Leslie was a consultant for Sellers Dorsey and also served as the state’s Medicaid director from 2015 to 2018.
CVS Health Expects to Close Acquisition of Signify Health. Modern Healthcare reported on March 27, 2023, that CVS Health said it expects to complete its $8 billion acquisition of home health provider Signify Health this week, pending resolution of certain remaining conditions of the merger agreement. Read More
Ohio Attorney General Files Lawsuit Alleging Companies Colluded to Raise Prices of Prescription Drugs. Modern Healthcare reported on March 27, 2023, that Ohio Attorney General Dave Yost filed a lawsuit alleging that Cigna subsidiary Express Scripts and Blue Cross Blue Shield-affiliated Prime Therapeutics worked with Switzerland-based Ascent Health Services to raise the prices of drugs. The suit alleges that the companies shared drug pricing and rebate information to fix rebates and prices. Read More
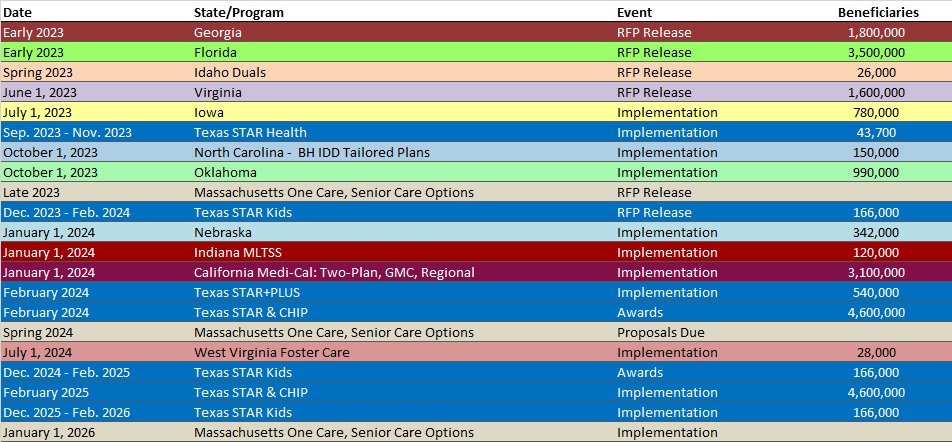
RFP Calendar
Company Announcements
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- District of Columbia Medicaid Managed Care Enrollment is Flat, Jan-23 Data
- District of Columbia Medicaid Managed Care Enrollment is Up 6.7%, 2022 Data
- Illinois Medicaid Managed Care Enrollment is Flat, Jan-23 Data
- Illinois Dual Demo Enrollment is Down 5.9%, Jan-23 Data
- Michigan Medicaid Managed Care Enrollment is Flat, Jan-23 Data
- Michigan Dual Demo Enrollment is Down 4.6%, Jan-23 Data
- Nevada Medicaid Managed Care Enrollment is Flat, Jan-23 Data
- New Mexico Medicaid Managed Care Enrollment is Flat, Jan-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama Medicaid Agency COVID Unwinding for SSI, ABD Populations RFP, Mar-23
- Alabama MES Modernization Program Enterprise Data Services RFP, Mar-23
- Idaho Medicaid Audit Services RFP, Mar-23
- Maryland Management of Pharmacy Reimbursement Methodology RFP, Mar-23
- Michigan Annual Reports & Audits for Disproportionate Share Hospital Medicaid Program RFP, Mar-23
- New York Consumer Assistance for ABD and Medicare Outreach as a Condition of Medicaid Eligibility RFA, Mar-23
Medicaid Program Reports, Data, and Updates:
- Arizona, Hawaii MES Modernization Roadmap, Feb-23
- California Governor’s Proposed Budget, FY 2023-24
- Colorado Health Cabinet Affordability Summit Materials, Mar-23
- Georgia Medical Care Advisory Committee Meetings, 2021-22
- Illinois Governor’s Proposed Budget, SFY 2024
- Iowa Medicaid MCO Quarterly Performance Data Reports, 2016-22
- New Jersey DMAHS Quality Strategy Report, 2022
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, Mar-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.