This week, our In Focus section reviews the new 1332 State Relief and Empowerment Waiver resources released by the Centers for Medicare & Medicaid Services (CMS) on July 15, 2019. The new resources, intended to help states better understand regulations and reduce burdens associated with waiver application, include four waiver concept papers on how states can take advantage of the flexibility to wave certain Affordable Care Act (ACA) requirements, as well as their respective application templates. CMS has also released an updated application checklist of required elements.
Medicaid
California 2019-20 Budget Overview
This week, our In Focus section reviews the California fiscal 2019-20 budget. California Governor Gavin Newsom signed his first budget, and much of its related legislation on June 27, 2019. The budget appropriates $214.8 billion ($147.8 billion General Fund) in total spending with $19.2 billion in reserves. The total reserves includes $16.5 billion in the Rainy Day Fund, $1.4 billion in the Special Fund for Economic Uncertainties, $900 million in the Safety Net Reserve, and nearly $400 million in the Public School System Stabilization Account.
Dual Eligible Financial Alignment Demonstration Enrollment Update
This week, our In Focus section reviews publicly available data on enrollment in capitated financial and administrative alignment demonstrations (“Duals Demonstrations”) for beneficiaries dually eligible for Medicare and Medicaid (duals) in nine states: California, Illinois, Massachusetts, Michigan, New York, Ohio, Rhode Island, South Carolina, and Texas. Each of these states has begun either voluntary or passive enrollment of duals into fully integrated plans providing both Medicaid and Medicare benefits (“Medicare-Medicaid Plans,” or “MMPs”) under three-way contracts between the state, the Centers for Medicare & Medicaid Services (CMS), and the MMP. As of May 2019, approximately 372,600 duals were enrolled in an MMP. Enrollment was flat from May of the previous year.
HMA, CMCS Launch Resource for Medicaid Innovation Program
A team of HMA consultants, led by Izanne Leonard-Haak and Matt Roan, have collaborated with organizations under a Centers for Medicaid and CHIP Services (CMCS) contract to provide support to CMCS on the Medicaid Innovation Accelerator Program.
Kentucky Releases Medicaid MCO RFP
This week, our In Focus section reviews the Kentucky Medicaid managed care organizations (MCOs) request for proposals (RFP), issued by the Kentucky Finance and Administration Cabinet on May 16, 2019. The Kentucky Cabinet for Health and Family Services (CHFS), Department for Medicaid Services (DMS) will select up to five Medicaid MCOs to manage health care services for more than 1.2 million people, starting July 2020. Contracts are estimated at more than $7 billion.
Medicaid Plan Profit Margin Dips to 0.5 Percent in 2018, Continuing Multi-Year Decline, HMAIS Analysis Shows
This week, our In Focus summarizes the findings of an HMA Information Services analysis of Medicaid managed care plan profitabilty, based on data from annual statutory filings made with the National Association of Insurance Commissioners (NAIC). For information on how to subscribe to HMA Information Resources, contact Carl Mercurio.
Underwriting Margin
An analysis by HMA Information Services, a division of Health Management Associates, shows that Medicaid managed care plans in 34 states and Washington, DC, posted a net underwriting margin of 0.5 percent in 2018, down 10 basis points from 0.6 percent in 2017. For-profit plans posted higher underwriting margins than not-for-profit plans.
Overall, margins have fallen consistently since hitting a four-year high of 2.4 percent in 2015. The data include financial information for about 210 Medicaid managed care plans, with total membership of 37 million in 2018 and revenues of about $188 billion. Net underwriting profit in 2018 was about $911 million, compared to more than $990 million in 2017.
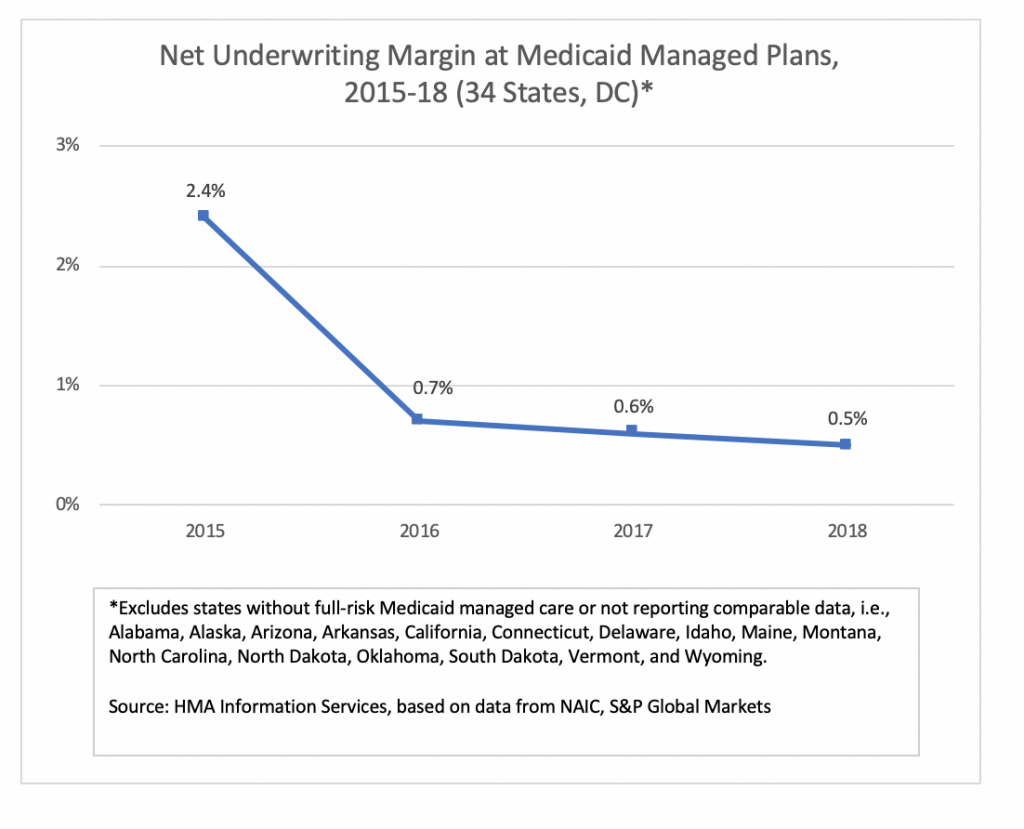
States in which the aggregate Medicaid managed care margin was below the national average in 2018 (based on plans reporting NAIC statutory filings) included Florida, Hawaii, Louisiana, Massachusetts, Mississippi, New Jersey, New Mexico, Rhode Island, Texas, and Virginia.
Not included in the tally are most Medicaid plans in California and Arizona, which don’t report financial information through NAIC. In addition, some of the largest plans in New York don’t report financial information through NAIC.
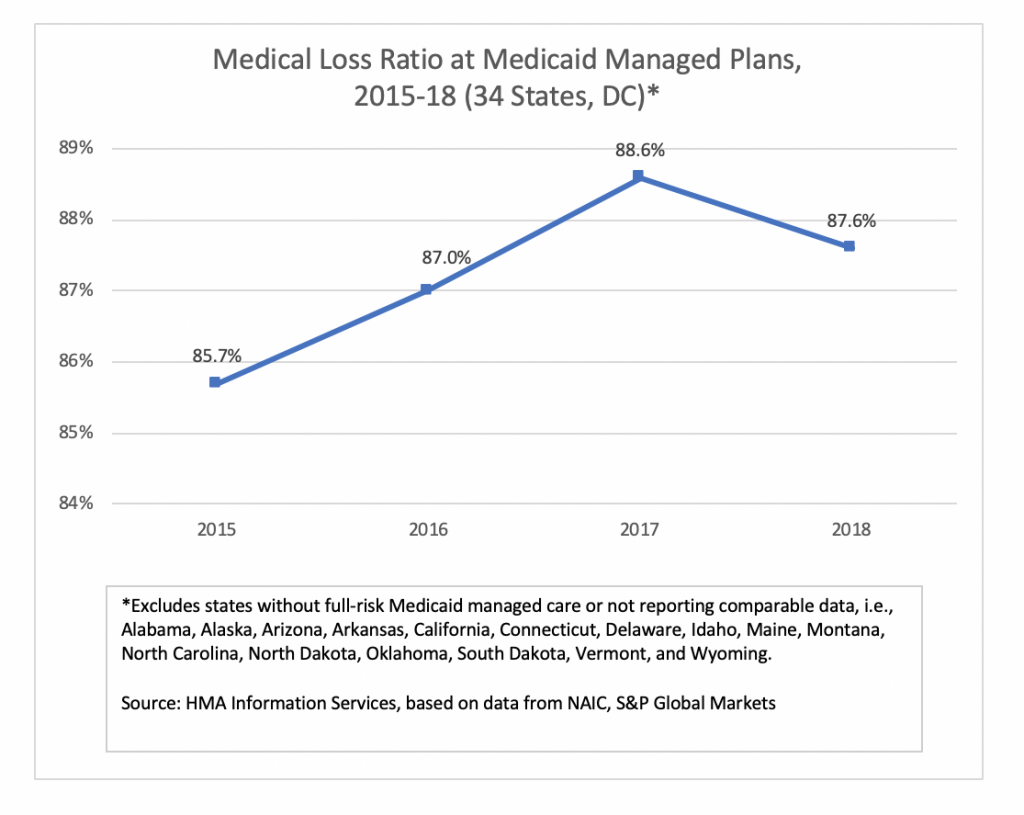
Medical Loss Ratio
Medical loss ratio (MLR) among Medicaid managed care plans in 34 states and Washington, DC, was 87.6 percent in 2018, down about 100 basis points from 2017. The MLRs calculated by HMAIS are blended and may include traditional Medicaid, expansion, and aged, blind and disabled populations, depending on the state. The improvement in average MLR was offset by an increase in administrative costs, resulting in the drop in underwriting margin.
Medicaid and Exchange Enrollment Update – January 2019
This week, our In Focus section reviews updated information issued by the Department of Health & Human Services (HHS) Centers for Medicare & Medicaid Services (CMS) on Medicaid expansion enrollment from the “January 2019 Medicaid and CHIP Applications, Eligibility Determination, and Enrollment Report,” published on April 25, 2019. Additionally, we review 2019 Exchange enrollment data from the “Health Insurance Exchanges 2019 Open Enrollment Period: Final State-Level Public Use File,” published by CMS on March 25, 2019. Combined, these reports present a picture of Medicaid and Exchange enrollment in 2019, representing 72.4 million Medicaid and CHIP enrollees and 11.4 million Exchange enrollees.
HMA Conference to Feature Insights from 40+ Speakers, Including Health Plan CEOs, State Medicaid Directors, Providers
Pre-Conference Workshop: September 8, 2019
Conference: September 9-10, 2019
Location: Chicago Marriott Downtown Magnificent Mile
Health Management Associates is proud to announce its fourth annual conference on trends in publicly sponsored health care: The Next Wave of Medicaid Growth and Opportunity: How Payers, Providers, and States Are Positioning Themselves for Success.
The HMA conference has emerged as a premier informational and networking event, attracting more than 450 executives and policy experts. Speakers this year include state Medicaid directors and leaders from Medicaid managed care, hospitals, clinics, community-based organizations, and other providers.
CMS Announces Primary Cares Initiative
On April 22, 2019, the Centers for Medicare & Medicaid Services (CMS) Innovation Center announced the Primary Cares Initiative (PCI), which will present eligible providers and other entities with the opportunity to engage in value-based payment and direct contracting payment models for primary care beginning in January 2020. CMS designed PCI to reduce expenditures and preserve or enhance quality of care for beneficiaries in Medicare fee-for-service (FFS). PCI is comprised of two tracks, Primary Care First (PCF) and Direct Contracting (DC). The PCF track, which builds on the Comprehensive Primary Care Plus (CPC+) initiative, is intended for individual primary care practices and seeks to reward providers for reductions in hospital utilization and total cost of care through performance-based payment adjustments. Also, under the PCF track, practices that specialize in serving high-need and/or seriously ill populations will receive adjusted payments to account for the populations served. Providers that participate in these models will qualify as participating in an Advanced Alternative Payment Model and be eligible to receive full bonus payments under CMS’s Medicare Incentive Payment System (MIPS).
HMA MACPAC Report Published
A team of HMA colleagues including Sarah Barth, Sharon Silow-Carroll, Esther Reagan, Mary Russell and Taylor Simmons completed a study for the Medicaid and Children’s Health Insurance Program (CHIP) Payment and Access Commission (MACPAC) to examine care coordination requirements for several Medicare-Medicaid integrated care models.
The study’s final report, Care Coordination in Integrated Care Programs Serving Dually Eligible Beneficiaries – Health Plan Standards, Challenges and Evolving Approaches, is posted to the MACPAC website.
The final report details state and federal managed care contract requirements for care coordination, summarizes stakeholders’ perspectives on care coordination based on structured interviews, and highlights promising care coordination practices and challenges for ensuring effective care coordination for dually eligible beneficiaries.