This week, our In Focus reviews the New Hampshire Medicaid Care Management (MCM) Services Draft request for proposals (RFP), released by the state Department of Health and Human Services (DHHS) on July 9, 2018. The MCM program, worth $750 million in annualized spending, will provide full-risk, fully capitated Medicaid managed care services to approximately 181,000 beneficiaries from July 1, 2019 through June 30, 2024. The final RFP is expected August 10, 2018.
The MCM program incentivizes value-based care over volume-based. The state is looking for managed care organizations (MCOs) that will improve population health, address the opioid crisis, expand community mental health services, and expand services in the child welfare system, among others. MCOs must provide person-centered, integrated care that offers all Medicaid managed care services.
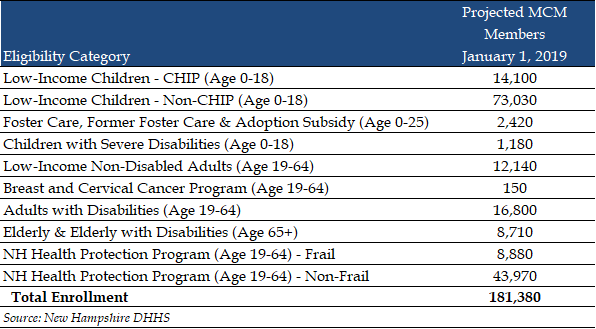
Eligible Populations
The MCM program will cover approximately 181,000 beneficiaries, including 43,970 Medicaid expansion members, who will transition from the New Hampshire Health Protection Program to MCM’s new Granite Advantage Health Care Program. Other eligible populations include: pregnant women, children, parents/caretakers, non-elderly, non-disabled adults under the age of 65, and individuals who are aged, blind or disabled. Excluded populations are those with eligibility under Family Planning Only, Health Insurance Premium Payment, In and Out Spend Down, Medicare Savings Program Only, members with Veterans Affairs benefits, and Retroactive/Presumptive Eligibility segments.
Services Covered
Plans will provide acute care, behavioral health, and pharmacy services for the covered populations. Long Term Services and Supports (LTSS), Developmental Disability and Acquired Brain Disorder services, and New Hampshire Division of Children, Youth, and Families (DCYF) Medicaid services are not covered. These services will continue to be offered through fee-for-service (FFS) outside of the MCM program, as will all services for select MCM exempt populations.
MCOs will develop and maintain a statewide Participating Provider network that adequately meets all covered medical, mental health, substance use disorder, and psychosocial needs of beneficiaries in every geographic area. MCOs will be required to provide emergency services at rates that are no less than the DHHS FFS rates, regardless of whether the provider has a partnership with the MCO or not. MCOs will also need to provide Non-Emergency Medical Transportation (NEMT) services for members.
Contracts
DHHS expects to award three MCOs with five-year contracts, running from July 1, 2019 through June 30, 2024. The current program, worth $540 million, will grow to $750 million in annualized spending with the addition of the Medicaid expansion program.
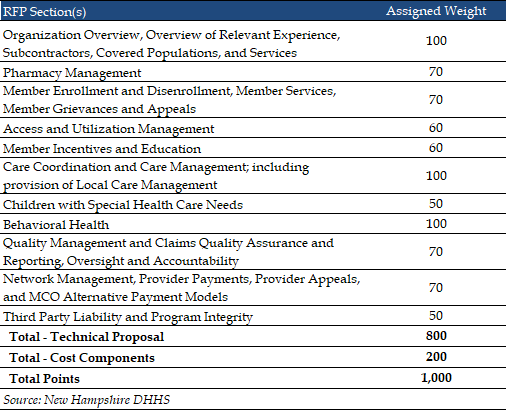
Evaluation Criteria
MCOs can score up to 800 points on their technical proposal, while the Cost Components of the RFP will be worth 200 points.
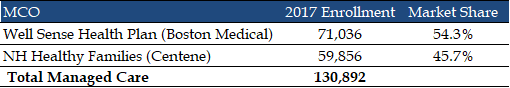
Current Market
New Hampshire transitioned to Medicaid managed care in 2013. As of 2017, there were 130,892 enrollees in the MCM program, served by Well Sense Health Plan (Boston Medical Center) and New Hampshire Healthy Families (Centene).
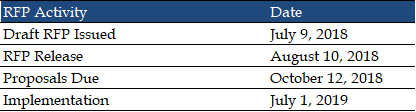
RFP Timeline
DHHS expects to release the final RFP on August 10, 2018. Proposals will be due in October and implementation will begin July 1, 2019.
Link to New Hampshire MCM Draft RFP
Link to New Hampshire MCM Draft Contract