HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: CMS Finalizes Significant Changes to Medicare Advantage and Medicare Part D Programs for 2025

- In Focus: Medicaid Managed Care Final Rule: What to Watch for

- California Medicaid FFS Contracts with Heali’s Food as Medicine Platform

- Colorado Settles Lawsuit Regarding Mental Health Care for Children, Agrees to Outside Examination of Program

- Avesis, Elevance Health Partner with Uber to Improve Maternal Health in Georgia

- Michigan Announces Medicaid Managed Care Awards

- New York Governor Invests $359 Million to Expand Supportive Housing Options

- North Dakota Approves Pilot Program for Paid Family Caregivers

- Vermont Receives Approval for Medicaid Mobile Crisis State Plan Amendment

- Virginia Governor Vetoes Prescription Drug Affordability Board Legislation

- CMS Announces Final Rule to Promote Competition, Access to Care in Medicare Advantage, Part D Plans

- Medicaid Supplemental, Base Payments Vary Among States, MACPAC Finds

- Lawmakers Call on FTC, DOJ to Block Optum-Steward Acquisition

In Focus
CMS Finalizes Significant Changes to Medicare Advantage and Medicare Part D Programs for 2025
This week, our In Focus section reviews a wide-ranging and comprehensive final rule released April 4, 2024, by the Centers for Medicare & Medicaid Services (CMS). The regulation revises and updates policies that affect Medicare Advantage (MA) and Medicare Part D coverage beginning in the upcoming plan year.
The policies adopted in the final rule aim to strengthen consumer protections and guardrails, promote fair competition, and ensure MA and Part D plans can best meet the healthcare needs of Medicare beneficiaries, including individuals dually eligible for Medicare and Medicaid. In addition, the final rule includes important new policies to expand access to behavioral health providers, promote equity in healthcare coverage, and improve access to and use of Medicare Advantage supplemental benefits. These policy changes complement payment policy changes that were recently finalized in the April 1, 2024, CMS CY 2025 Rate Announcement and will take effect June 3, 2024.
Below HMA experts walk through the major policies CMS finalized.
Expanding Access to Behavioral Health Providers
CMS finalized several regulatory changes to improve Medicare beneficiaries’ access to behavioral health services through strengthened MA network adequacy standards. These changes include:
- Establishing network evaluation standards for a new facility-specialty provider category, called outpatient behavioral health. This category includes a range of behavioral health providers, including marriage and family therapists (MFTs), mental health counselors (MHCs), opioid treatment programs, community mental health centers, addiction medicine specialists and facilities. Outpatient behavioral health will be included in network adequacy evaluations.
- Permitting MFTs and MHCs to enroll and start billing Medicare—as a result of statutory changes established in the Consolidated Appropriations Act (CAA) of 2023—and establishing corresponding changes to network adequacy standards for MA plans.
- Requiring MA plans to independently verify that behavioral health providers added to their network furnish services to at least 20 patients within a 12-month period.
- Adding outpatient behavioral health facility-specialty to the list of the specialties that will receive a 10 percent credit toward meeting network adequacy time and distance standards.
Impact: Adding the outpatient behavioral health category is expected to enhance Medicare beneficiaries’ access to a broader scope of behavioral health specialists. As result of the new policy and network expectations, MA plans may need broaden their networks, and providers that contract with MA plans may need to strengthen their capacity to address Medicare billing and reporting requirements, including quality reporting initiatives.
Require Mid-Year Enrollee Notification of Supplemental Benefits
The number of MA plans that offer supplemental benefits to beneficiaries is increasing, with the most frequently offered supplemental benefits including coverage for vision, dental, and hearing services. Moreover, many MA plans also are offering supplemental benefits to address unmet social determinants of health needs, including home meal delivery, transportation, and in-home services and supports. At the same time, use of these benefits is reportedly low, and there are gaps in research and data analysis about how these benefit offerings are affecting beneficiaries’ cost and health outcomes.
As a result, CMS is finalizing policies that require MA plans to engage in outreach to beneficiaries. Specifically, the final rule requires MA plans to send enrollees a mid-year notification regarding their unused supplemental benefits. The notification must include information on the scope of the benefit, patient cost-sharing, and detailed instructions on how beneficiaries can access their unused benefits.
Impact: This change is intended to improve beneficiary awareness of plans’ supplemental benefit offerings and encourage greater use of these benefits. As a result of the regulatory changes, MA plans may look to further refine and adjust their MA supplemental benefit offerings to further improve the healthcare experience for Medicare beneficiaries.
New Standards for Supplemental Benefits under SSBCI
MA plans also offer supplemental benefits to beneficiaries through the Special Supplemental Benefits for the Chronically Ill (SSBCI) program, whereby people with ongoing and complex chronic conditions can receive supplemental benefits that are tailored to their specific health and social needs. In the final rule, CMS establishes new requirements for MA plans to demonstrate the value of these services by submitting evidence that the item or service will improve or maintain the overall health of chronically ill beneficiaries.
Impact: This new reporting requirement is intended to ensure that SSBCI items and services are evidence-based and meaningful. As these regulatory changes are implemented under tight timelines, plans will need to move quickly to compile clinical data and evidence on the effectiveness of these targeted benefits, while also considering changes in their benefit offerings to better meet the needs of beneficiaries with complex and chronic conditions.
MA Star Rating Changes
In the final rule, CMS describes its ongoing work to streamline quality measures, including the agency’s progress in moving toward the Universal Foundation of core quality measures that are aligned across CMS’s quality and value-based programs. CMS notes that MA plans are beginning to report additional measures that are part of the Universal Foundation. Under previous regulations, CMS proposed to make the following changes to specific measures in the Star Ratings system:
- Remove the standalone Part C medication reconciliation post-discharge measure
- Add the updated Part C colorectal cancer screening measure with the NCQA (National Committee for Quality Assurance) specification change
- Add the updated Part C care for older adults−functional status measure with the NCQA specification change.
Impact: These changes build on earlier CMS efforts to improve the Star Rating system, including adding a health equity index and reducing the weight of patient experience and access measures to better align with the CMS Quality Strategy.
Ensure More Dual-Eligible Managed Care Beneficiaries Receive Medicare and Medicaid Services from the Same Organization
CMS finalized several significant changes designed to improve access to integrated care for dually eligible beneficiaries, including the following:
- CMS is limiting enrollment in certain Dual Eligible Special Needs Plans (D-SNPs) to individuals who are also enrolled in an affiliated Medicaid managed care organization (MCO).
- CMS also limits the number of D-SNP benefit packages that an MA organization can offer in the same service area as an affiliated Medicaid MCO. If a state Medicaid agency requires it, MA plans may offer more than one D-SNP for full-benefit dually eligible individuals in the same service area as the MA organization’s affiliated Medicaid MCO.
- Dually eligible beneficiaries will have an opportunity to enroll in an integrated D-SNP monthly under a new integrated care special enrollment period (SEP).
- CMS is lowering the D-SNP look-alike threshold from 80 percent to 70 percent for plan year 2025 and to 60 percent for plan year 2026 and into the future.
Impact: These are considerable changes that are designed to increase the percentage of dually eligible beneficiaries enrolled in MA plans that also are contracted to cover Medicaid benefits. In addition, these changes will expand access to integrated member materials, unified appeals processes across Medicare and Medicaid, and continued beneficiary access to Medicare services during an appeal.
Require Health Equity Assessments of Utilization Management Practices and Procedures
CMS finalized several regulatory changes to the composition and responsibilities of MA plans’ utilization management (UM) committees, including the following:
- At least one member of the UM committee must have expertise in heath equity.
- The UM committee must conduct an annual assessment of UM practices and procedures on health equity, with a particular focus on the impact on beneficiaries who are low-income, dually eligible for Medicare and Medicaid, or have a disability.
- MA plans must make the health equity analysis publicly available on the plan’s website.
Impact: These policy changes are aimed at assessing the impact of utilization management through a health equity lens and ensuring that these policies and procedures do not have a disproportionate impact on access to medically necessary care for underserved populations.
Other Provisions
The final rule makes several other notable regulatory changes to MA and Part D, which include:
- Allowing Part D plans to substitute biosimilars for the reference biologic product during the plan year as part of formulary maintenance changes, which is expected to expand access to lower cost biosimilars for Medicare beneficiaries
- Limiting out-of-network cost sharing for D-SNP PPOs
- Standardizing the MA risk adjustment data validation appeals process
- Establishing new guardrails for plan compensation to agents and brokers to prevent anti-competitive steering of beneficiaries and new requirements to third-party marketing organizations
- Changes to Medicare Part D medication therapy management (MTM) eligibility criteria
What’s Next
CMS continues its work to incorporate requirements for consumer engagement and transparency of data to address health equity. This final rule is poised to have a significant impact on plan benefit design and the landscape of health insurance markets in states and regions of states. CMS has created additional opportunities for states to advance integrated care initiatives that align with Medicaid, which will have downstream implications for MA and Medicaid plans, providers, and partnering organizations.
The Health Management Associates team will continue to analyze and assess these regulatory changes that CMS has finalized. We have the depth, experience, and expertise to assist in tailored analysis and model policy impacts of the recently finalized changes. For more information or questions about the policies described, contact Amy Bassano ([email protected]), Julie Faulhaber ([email protected]), Andrea Maresca ([email protected]), or Greg Gierer ([email protected]).
Medicaid Managed Care Final Rule: What to Watch for
Our second In Focus section provides a refresher on the Medicaid and Children’s Health Insurance Program managed care access, finance, and quality proposed rule that the Centers for Medicare & Medicaid Services (CMS) published in May 2023. As Health Management Associates, Inc. (HMA), has noted, the final rule is expected to be published later this month. If finalized as proposed, several provisions in the rule will signal the start of a new era of accountability and transparency for the Medicaid program.
The policy changes are expected to fall into the following major categories: in lieu of services (ILOS), the Medicaid and CHIP Quality Rating System (MAC QRS), medical loss ratios (MLRs), network adequacy, and state directed payments (SDPs). These revised policies will affect Medicaid coverage and reimbursement for years to come. Following is a summary of the proposed policy changes to watch for in the final rule.
ILOS
CMS has proposed to expand upon and codify the sub-regulatory guidance around ILOS outlined in State Medicaid Director Letter #23-001. The letter advised state that they have the option to use the ILOS authority in Medicaid managed care programs to reduce health disparities and address unmet health-related social needs, such as housing instability and nutrition insecurity. The final rule would expand upon and codify that guidance.
For example, although the ILOS proposal adds reporting requirements and guardrails to address fiscal accountability, the proposed rule also noted that the substitution of an ILOS for a state plan service or setting should be cost-effective but does not need to meet budget neutrality requirements. States are also permitted to specify that an ILOS can be an immediate or longer-term substitute for a state plan service or setting.
MAC QRS
CMS has proposed a MAC QRS framework that includes: (1) mandatory quality measures, (2) a quality rating methodology, and (3) a mandatory website display format. State Medicaid agencies and managed care organizations (MCOs) will be required to adopt and implement the MAC QRS framework that CMS develops or adopt and implement an alternative but equivalent managed care quality rating system. CMS will update the mandatory measure set at least every two years. Any planned modifications to measures will be announced publicly through a call letter or similar guidance, with measures based on: (1) value in choosing an MCO; (2) alignment with other CMS programs; (3) the relationship to enrollee experience, access, health outcomes, quality of care, MCO administration, or health equity; (4) MCO performance; (5) data availability; and (6) scientific acceptability.
State Medicaid agencies will be required to collect from MCOs the data necessary to calculate ratings for each measure and ensure that all data collected are validated. In addition, state Medicaid agencies will be expected to calculate and issue ratings to each MCO for each measure.
Lastly, state websites will be required to contain the following elements: (1) clear information that is understandable and usable for navigating the website itself; (2) interactive features that allow users to tailor specific information, such as formulary, provider directory, and ratings based on their entered data; (3) standardized information so that users can compare MCOs; (4) information that promotes beneficiary understanding of and trust in the displayed ratings, such as data collection timeframes and validation confirmation; and (5) access to Medicaid and CHIP enrollment and eligibility information, either directly on the website or through external resources.
MLRs
CMS has proposed three areas for revision to its existing MLR standards, which require MCOs to submit annual MLR reports to states, which, in turn, must provide CMS with an annual summary of those reports. Areas for revision include: (1) requirements for clinical or quality improvement standards for provider incentive arrangements, (2) prohibited administrative costs in quality improvement activity (QIA) reporting, and (3) additional requirements for expense allocation methodology reporting.
With regard to provider incentive arrangements, CMS proposes to require that contracts between MCOs and providers: (1) have a defined performance period that can be tied to the applicable MLR reporting period(s), (2) include well-defined quality improvement or performance metrics that the provider must meet to receive the incentive payment, and (3) specify a dollar amount that can be clearly linked to successful completion of these metrics as well as a date of payment. MCOs would be required to maintain documentation that supports these arrangements beyond attestations.
In terms of QIA reporting, CMS proposes to explicitly prohibit MCOs from including indirect or overhead expenses when reporting QIA costs in the MLR. CMS also intends to add requirements regarding how MCOs can allocate expenses for the purpose of calculating the MLR by requiring MCOs to offer a detailed description of their methodology.
Network Adequacy
CMS has proposed a range of new network adequacy requirements intended to improve timely access to care for managed care enrollees. Those related to appointment wait time standards and secret shopper surveys are among the most prominent.
For appointment wait time standards, CMS proposes that state Medicaid agencies develop and enforce wait times associated with routine appointments for four types of services: (1) outpatient mental health and substance use disorder (SUD) for adults and children, (2) primary care for adults and children, (3) obstetrics and gynecology (OB/GYN), and (4) an additional service type determined by each state Medicaid agency using an evidence-based approach. The maximum wait times must be no longer than 10 business days for routine outpatient mental health and SUD appointments and no more than 15 business days for routine primary care and OB/GYN appointments. State Medicaid agencies could impose stricter wait time standards but not more lax ones. The wait time standard for the fourth service type will be determined at the state level.
State Medicaid agencies also will be required to engage an independent entity to conduct annual secret shopper surveys to validate MCO compliance with appointment wait time standards and the accuracy of provider directories to identify errors, as well as providers that do not offer appointments. For an MCO to be compliant with the wait time standards, as assessed through the secret shopper surveys, it would need to demonstrate a rate of appointment availability that meets the wait time standards at least 90 percent of the time.
SDPs
CMS has proposed several important changes to the requirements governing the use of SDPs, strengthening both the accountability required of and flexibility afforded to states. For example, CMS proposes to require that provider payment levels for inpatient and outpatient hospital services, nursing facility services, and the professional services at an academic medical center not exceed the average commercial rate. Furthermore, states would be required to condition SDPs upon the delivery of services within a contract rating period and prohibited from using post-payment reconciliation processes.
With regard to flexibility, CMS proposes to remove unnecessary regulatory barriers to support the use of SDPs by states to implement value-based payment arrangements and include non-network providers in SDPs. The proposal also permits states to implement, without prior approval, minimum fee schedules in Medicaid consistent with Medicare provider rates.
What’s Next
CMS is expected to publish the final rule in April. In addition, CMS plans to publish a separate final rule addressing new regulations pertaining to access to care, which will have equally significant impacts on states, MCOs, and providers. If you have questions about how HMA can support your efforts related to the managed care final rule’s implications and the context of other federal regulations for states, MCOs, or providers , contact Michael Engelhard, Managing Director, Regional Managed Care Organizations, and Andrea Maresca, Managing Director, Information Services.
HMA Roundup
Arizona
Arizona Reports $291 Million in Medicaid Fraud Savings, Recoveries. The Arizona Health Care Cost Containment System (AHCCCS) reported on April 5, 2024, that the Office of the Inspector General (OIG) collected a total of $291.4 million in savings and recoveries in 2023. Of the total, $272.6 million were from provider savings and recoveries and $18.8 million were member savings and recoveries. The OIG opened 8,869 cases, more than in any of the five prior years, and closed 8,039 cases. Read More
California
California Medicaid FFS Contracts with Heali’s Food as Medicine Platform. MedCity News reported on April 7, 2024, that Heali, a nutrition tech company, has contracted with California’s Medicaid fee-for-service (FFS) program to provide evidence-based dietary recommendations tailored to more than 200 chronic conditions. Food products and recipes are analyzed using AI and peer-reviewed medical research. Read More
Colorado
Colorado Settles Lawsuit Regarding Mental Health Care for Children, Agrees to Outside Examination of Program. The Colorado Sun reported on April 9, 2024, that the Colorado Department of Health Care Policy and Financing must hire an outside consultant to examine its mental health services for children after a class-action lawsuit alleged that the system’s lack of coordination resulted in high rates of institutionalization and poor access to care and medication. Under the settlement agreement, the state did not admit to violating federal or state laws but did agree to pay for an outside examination of its Medicaid policies. Additionally, the Department of Health Care Policy and Financing will be required to develop a plan including in-home mental health services, mobile crisis intervention, and stabilization services within the year and implement the plan within five years. Read More
Georgia
Avesis, Elevance Health Partner with Uber to Improve Maternal Health in Georgia. Fierce Healthcare reported on April 9, 2024, that supplemental benefits administrator Avesis and Elevance Health subsidiary Amerigroup Georgia have partnered with Uber Health as part of a pilot project aiming to improve maternal health in Georgia. The program has utilized community health partners including the Georgia Primary Care Association and federally qualified health centers (FQHCs) in order to provide Amerigroup’s Medicaid members with two individualized nutrition counseling sessions, a scale, and $300 of Uber Eats vouchers. Of the 745 referrals from FQHCs, approximately 85 percent of individuals have chosen to participate in the program. Read More
Idaho
Idaho Governor Asks Legislators to Amend Bill to Avoid Disruption in Medicaid Waiver Demonstration Services. The Idaho Capital Sun reported on April 9, 2024, that Idaho Governor Brad Little sent a letter asking legislators to amend a recently enacted bill, sponsored by Representative Megan Blanksma (R-Hammett), that requires legislative approval for Medicaid Section 1115 demonstrations and Section 1915 waivers. Little is concerned the bill may hamper the administration’s ability to make changes to the Idaho Behavioral Health Plan and reduce payments to skilled nursing facilities by $30 to $40 million and $70 million for immediate care facilities. Representative Blanksma indicated she expects to resolve the concerns with the bill. Read More
Indiana
Indiana Creates Waitlist for Medicaid Aged, Disabled Waiver. WFYI Indianapolis reported on April 5, 2024, that the Indiana Family and Social Services Administration recently announced they had reached the maximum number of slots for the state’s Medicaid Aged and Disabled waiver program. The state will establish a waitlist for the program, which will help to address the state’s $1 billion Medicaid shortfall. Although the state will add a total of 5,000 additional slots for this and a separate home and community based services program starting in July, the number of individuals on the waitlist already surpasses that amount. Read More
Iowa
Iowa House Approves Bills Extending Postpartum Medicaid Coverage, Limiting Eligibility. The Iowa Capital Dispatch reported on April 3, 2024, that the Iowa House approved a bill that would extend postpartum Medicaid coverage to 12 months but limit eligibility from 380 percent of the federal poverty level to 215 percent. It is estimated that 1,300 women and 400 infants will lose Medicaid coverage per month under the new restrictions. Separately, the House passed a bill to allow the Iowa Department of Health and Human Services to directly oversee the More Options for Maternal Support program and contract with providers, removing the previous requirement to hire a third-party administrator. Read More
Kansas
Kansas Senators to Vote on Procedural Motion for Medicaid Expansion. The Kansas Reflector reported on April 9, 2024, that on April 26, Kansas Senators are scheduled to vote on a motion that would allow the full chamber to debate on a Medicaid expansion bill. The procedural motion to bring Senate Bill 355 to the floor for consideration would require approval from 24 of the 40 senators. Read More
Michigan
Michigan Announces Medicaid Managed Care Awards. The Michigan Department of Health and Human Services (MDHHS) announced on April 8, 2024, its intent to award managed care contracts for the Comprehensive Health Care Program to nine health plans: incumbents CVS/Aetna, Blue Cross Blue Shield of Michigan, Centene, HAP CareSource, McLaren Health Plan, Molina, Priority Health Choice, UnitedHealthcare, and Upper Peninsula Health Plan. The Medicaid managed care organizations (MCOs) will serve 10 regions, each consisting of multiple counties. MDHHS developed new health plan contracts that are designed to address social determinants of health through investment in and engagement with community-based organizations. A key change in the new contracts is the addition of “in lieu of services” which will allow plans to pay for evidence-based nutrition services. Implementation is expected on October 1, 2024, and will run for five years with three, one-year renewal options. Read More
Michigan Extends CSHCS Coverage to Medically Eligible Individuals Up to Age 26. The Michigan Department of Health and Human Services announced on April 5, 2024, that the state will extend Children’s Special Health Care Services (CSHCS) coverage to medically eligible individuals up to age 26, effective retroactive to October 1, 2023. Previously, eligibility went up to age 21. Read More
Mississippi
Mississippi Lawmakers to Negotiate Final Details on Medicaid Expansion Bill in Public Meetings. Mississippi Today reported on April 9, 2024, that House Speaker Jason White and Lieutenant Governor Delbert Hosemann will will hold public conference committee meetings on a Medicaid expansion bill. Officials will try to reach a compromise on the different House and Senate-approved proposals. If lawmakers reach an agreement, the revised bill will go back to the full Senate and House again for consideration. Read More
Missouri
Missouri Senate Advances Bill Blocking Medicaid Payments for Planned Parenthood. Missouri Independent reported on April 10, 2024, that the Missouri Senate has advanced a bill which would prohibit Medicaid from paying for health care services from any organization that affiliates with abortion providers, including Planned Parenthood. The bill now returns to the House. Read More
New York
New York Governor Invests $359 Million to Expand Supportive Housing Options. Crain’s Health Pulse reported on April 1, 2024, that New York Governor Kathy Hochul has made a $359 million investment through a mix of bonds and subsidies to expand supportive housing options, including supportive units for homeless individuals with mental illness and substance use disorder and units for formerly incarcerated individuals. A total of 329 supportive housing units will be created in the Brownsville area of Brooklyn and the Mount Hope neighborhood in the Bronx. Tenants 50 years of age will be connected with primary and behavioral health care, employment support, and financial literacy classes. The state will also build 385 affordable units in East New York, including 94 supportive apartments for families experiencing homelessness. Read More
New York Legislators Consider MCO Tax to Garner Additional Medicaid Federal Matching Dollars. The New York Times reported on April 5, 2024, that some New York legislators are proposing a Medicaid managed care organization (MCO) tax that would generate additional federal matching dollars for the state’s Medicaid program. Specifically, the proposal would require MCOs to pay a tax to the state, which the state would use to draw down federal funds, a portion of which would be used to increase rates. Read More
Health Care Providers Remain Financially Stable Following Pharmacy Benefit Program Transition to FFS. Crain’s New York Business reported on April 5, 2024, that New York health care providers have maintained financial stability following the state’s transition from a managed care to a fee-for-service (FFS) model for its Medicaid pharmacy benefit program. The transition ended providers’ payments from the federal 340B drug program, which raised concerns of potential financial losses. The state indicated that it is still on track to save the anticipated $400 million per year and has reinvested approximately $900 million into hospitals, federally qualified health centers, and Ryan White clinics. Read More
North Carolina
North Carolina On Track to Launch Behavioral Health IDD Tailored Plans July 1. North Carolina Health News reported on April 4, 2024, that officials from North Carolina’s four Local Management Entity-Managed Care Organizations (LME-MCOs) indicated that the Behavioral Health and Intellectual/Developmental Disabilities (BH IDD) Tailored Plans will be implemented on July 1 during a meeting with the legislature’s Joint Legislative Oversight Committee on Medicaid. Tailored plans will serve approximately 150,000 individuals with severe mental health conditions or intellectual and developmental disabilities. Implementation has been delayed multiple times since 2022, most recently from October 2023. The four awarded LME-MCOs are Alliance Health, Partners Health Management, Trillium Health Resources, and Vaya Health. Read More
North Dakota
North Dakota Approves Pilot Program for Paid Family Caregivers. KFYR TV reported on April 8, 2024, that North Dakota has approved a family paid caregiver pilot program which will pay those caring for a disabled child or adult at home who cannot obtain outside help and is enrolled in certain Medicaid programs. The application period began on April 1. Read More
Oregon
Oregon Medicaid Plans to Establish Diabetes Prevention Program. The Oregon Health Authority announced on April 9, 2024, that it plans to submit Medicaid state plan amendments to the Centers for Medicare & Medicaid Services (CMS) to add a National Diabetes Prevention Program and to allow fee-for-service coverage of non-covered outpatient drugs when Oregon pharmacies can not supply the FDA-approved, non-imported version of the drug. The public comment period will be open through May 10. Read More
Pennsylvania
Pennsylvania Disenrolls 500,000 Medicaid Beneficiaries During Redeterminations Since April. WHYY PBS reported on April 4, 2024, that Pennsylvania has disenrolled approximately 500,000 Medicaid beneficiaries since eligibility redeterminations began in April 2023. State officials indicated that the process is anticipated to conclude by the end of June. In February, Pennsylvania disenrolled 44,234 Medicaid beneficiaries, including 24,866 due to ineligibility and 19,368 due to procedural reasons. Read More
Texas
Texas Submits Extension Request for Healthy Texas Women Section 1115 Waiver Demonstration with Shift to Managed Care. The Centers for Medicare & Medicaid Services (CMS) announced on April 4, 2024, that Texas requested an extension for the Healthy Texas Women (HTW) Section 1115 waiver demonstration for five years through December 2029. The demonstration proposes to transition the delivery of HTW services from the current fee-for-service model to a managed care model. The waiver would also include a more robust health and family planning services benefit package for low-income women not otherwise eligible under Texas Medicaid. The public comment period will run through May 5. Read More
Texas Terminates Conduent’s Awarded Contract as TMHP Claims Vendor. Texas Health and Human Services announced on April 4, 2024, that Texas terminated Conduent’s contract for the Texas Medicaid & Healthcare Partnership (TMHP) claims vendor. Incumbent Accenture will continue operating as the TMHP claims vendor until further notice. Read More
Vermont
Vermont Receives Approval for Medicaid Mobile Crisis State Plan Amendment. The Centers for Medicare & Medicaid Services approved on April 4, 2024, a Vermont Medicaid state plan amendment, which will allow the state to develop mobile crisis intervention teams to connect eligible individuals to behavioral health providers 24 hours a day. The program is effective January 1, 2024. Read More
Virginia
Virginia Governor Vetoes Prescription Drug Affordability Board Legislation. STAT reported on April 9, 2024, that Virginia Governor Glenn Youngkin vetoed a bill, sponsored by Delegate Karrie Delaney (D-Fairfax), that would have created a Prescription Drug Affordability Board. The board would have been tasked with setting upper payment limits for select prescription medications. Read More
National
CMS Announces Final Rule to Promote Competition, Access to Care in Medicare Advantage, Part D Plans. The U.S. Department of Health and Human Services released on April 4, 2024, the Contract Year (CY) 2025 Medicare Advantage (MA) and Medicare Part D final rule, intended to promote competition, increase access to care, and protect beneficiaries from inappropriate marketing and prior authorization. Specifically, the rule will establish compensation limits for agents and brokers to prevent anti-competitive practices, require MA plans to retain a health equity expert to analyze prior authorization policies, and expand access to behavioral health providers and services. The rule also requires plans to make efforts to inform beneficiaries of available supplemental benefits and allows Part D plans to utilize more lower cost biosimilar biological products to ensure more affordable treatment options. Read More
Medicaid Supplemental, Base Payments Vary Among States, MACPAC Finds. The Medicaid and CHIP Payment and Access Commission (MACPAC) released in April 2024, an issue brief that found that Medicaid hospital supplemental payments varied among states in fiscal 2022. These payments accounted for less than five percent of Medicaid spending in 13 states and more than 25 percent of Medicaid spending in six states. Directed payments were the main type of supplemental payment in 23 states, while disproportionate share hospital (DSH) supplemental payments were the largest in 13 states, and non-DSH payments were the largest in 14 states. Read More
Health Disparities Have Increased Between Rural and Urban Individuals, USDA Finds. KFF Health News reported on April 9, 2024, that health disparities between individuals living in rural and urban communities widened by approximately 37 percent between 1999 through 2001 and 2017 through 2019, according to a recent report from the U.S. Department of Agriculture (USDA). The report found that adults aged 25 to 54 living in rural communities experienced higher incidence of cancer, heart disease, lung disease, hepatitis, and pregnancy-related deaths in comparison to their urban counterparts. The natural-cause mortality rate for Non-Hispanic American Indian and Alaska Native individuals increased by 46 percent. Although the report does not examine causes for increased mortality rates, researchers noted that disparities in health care resources and lack of access to Medicaid in non-expansion states may play a role. Read More
Several States Lack Behavioral Providers for Medicare, Medicaid Populations, OIG Finds. Bloomberg Law reported on April 3, 2024, that there were fewer than five mental health providers accepting Medicare and Medicaid patients per 1,000 enrollees, according to a review conducted by the Department of Health and Human Services Office of Inspector General (OIG). The review surveyed provider availability in 20 counties across 10 states including Arizona, Illinois, Iowa, Mississippi, Nebraska, New York, Ohio, Oregon, Tennessee, and Virginia. Read More
MACPAC Meeting Is Scheduled for April 11-12. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on April 5, 2024, that its next meeting will be held on April 11-12. Among the topics for discussion will be options for improved transparency of Medicaid financing, and options to help states use state Medicaid agency contracts to better integrate care for people who are dually eligible for Medicare and Medicaid. Read More
Industry News
UnitedHealth Group Held to New Ransom Demands Over Stolen Data During Cyberattack. Health Payer Specialist reported on April 9, 2024, that a new group of hackers are holding UnitedHealth Group to a ransom demand after claiming to have stolen data from Change Healthcare. Hacked data reportedly includes medical and dental records, payment and claims information, patient personal identifiable information, and more than 3,000 source code files of Change Healthcare software. Read More
Lawmakers Call on FTC, DOJ to Block Optum-Steward Acquisition. Modern Healthcare reported on April 8, 2024, that federal lawmakers sent a letter to the Federal Trade Commission and the Department of Justice conveying their concerns regarding UnitedHealth’s subsidiary Optum’s proposed acquisition of Steward Health Care’s physician group. Lawmakers, including Senators Elizabeth Warren (D-MA) and Edward Markey (D-MA), have alleged that the Optum-Steward transaction would reduce competition in Massachusetts and could hurt the quality of care if physicians have to limit their network participation. Read More
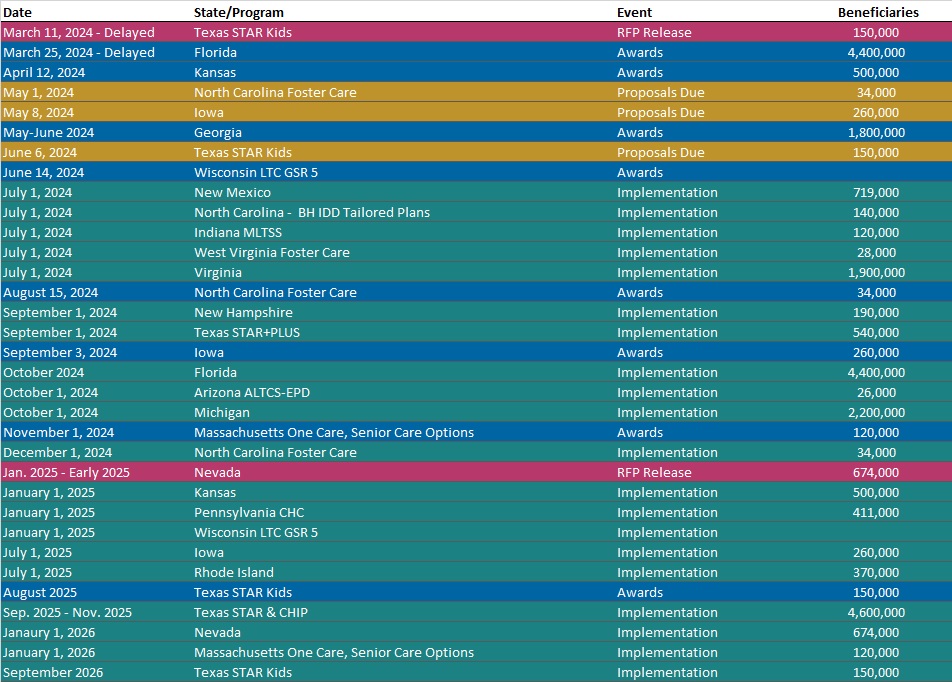
RFP Calendar
Company Announcements
MCG Health White Paper:
Obesity Treatment: The Current State of the Evidence: MCG Physician Editor, Jennifer N. Goldstein, MD, MSc, explores the current state of evidence around obesity treatment including lifestyle, pharmacologic, and surgical interventions as well as treatment recommendations. Read More
HMA News & Events
HMA Webinars:
Equity Considerations for Addressing Opiate Use Disorder. Tuesday, April 23, 2024, 1 PM ET. Nationally, we are seeing trending disparities in opioid use disorder prevalence and overdose deaths—whether it be brown and black communities or pregnant and parenting people. We will overview 3 projects that demonstrate how HMA has partnered with States and Counties to address opioid use disorder with an equity focus. Register Here
Substance Use Disorder (SUD) Ecosystem of Care: Building Systems-Thinking in the SUD Ecosystem. Wednesday, May 1, 2024, 12 PM ET. The final webinar of this three-part series emphasizes the importance of a comprehensive and interconnected spectrum of engagement and treatment strategies. To truly build and maintain an SUD ecosystem with accountability across the system and ‘no wrong door,’ best practices must embrace a systems-thinking approach. An interconnected system requires building strong partnerships across the SUD ecosystem and engagement and treatment strategies will focus on leveraging those partnerships to facilitate engagement of individuals throughout the system. Register Here
Wakely, an HMA company, Webinar:
How the New MA/PD Risk Models & Post-IRA Part D Benefit are Changing the View of Medicare Profitability. Monday, April 22, 2024, 3 PM ET. Medicare risk scores continue to evolve, with increasing weight given to the MA’s 2024 v28 HCC risk score model and the introduction of a new post-IRA RxHCC risk score model for payment year 2025. In addition, basic Part D benefit costs are expected to change dramatically due to the overhaul of the Part D defined standard benefit in 2025 as part of the Inflation Reduction Act. These key changes to the Medicare Advantage and Part D programs have the potential to cause material shifts in the revenue, claims, and the drivers of profit/loss for MA/PD plans. This raises the question: how will the profiles for historically profitable/unprofitable members change in 2025 & beyond? Wakely has conducted in-depth analyses to explore the impact of risk score model changes and 2025 Part D defined standard benefit changes has on the overall profitability of certain MA-PD cohorts. In this webinar, we will share an overview of some of the results and discuss how plans can potentially use this analysis to inform strategies. Register Here
