HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- HMA News: Health Management Associates’ CEO Douglas Elwell Retiring; COO Charles (Chuck) Milligan to Lead Firm

- In Focus: Medicaid Managed Care Enrollment Update—Q4 2023

- In Focus: Policy and Operational Implications of the Change Healthcare Cyberattack

- Arkansas Awards CSG Government Solution IV&V Contract

- Connecticut Submits Section 1115 Substance Use Disorder Demonstration Amendment

- Kansas Delays KanCare, CHIP Medicaid Managed Care RFP Awards

- Florida Announces Awards for Statewide Medicaid Managed Care Procurement

- Mississippi Study to Test Food is Medicine Pilot Program

- Nevada Proposes New Behavioral HCBS Program for Children

- New York Governor Announces Fiscal 2025 State Budget Agreement with Legislature

- Ohio MCOs Fund Community-based Programs Under NextGen Model

- CMS Proposes Transforming Episode Accountability Model to Improve Care During Surgery, Recovery for Medicare Beneficiaries

- Medicare Telehealth Utilization Decreased in 2022; Does Not Limit Access to In-person Care, MedPAC Finds

- Accenture Federal Services to Acquire Cognosante

- Elevance, Clayton, Dubilier & Rice Invest in Primary Care Access Partnership

In Focus
Health Management Associates’ CEO Douglas Elwell Retiring; COO Charles (Chuck) Milligan to Lead Firm
On April 17, 2024, Jay Rosen, founder, president, and chairman of Health Management Associates (HMA), announced Chief Executive Officer (CEO) Douglas L. Elwell is retiring. Chief Operating Officer (COO) Charles (Chuck) Milligan will succeed him as CEO effective May 17.
Elwell assumed the role of HMA’s CEO in November 2020. He had rejoined the firm as COO in February of that year after serving as the Illinois Medicaid director. During his first tenure with HMA, Elwell was a principal and managing principal in the Indianapolis office from July 2003 through October 2014. Much of his career, prior to joining HMA, was dedicated to leading hospital systems in roles as CEO, COO, and CFO. Elwell was deputy chief executive officer for finance and strategy for the Cook County Health and Hospitals System from November 2014 until early 2019.
“Doug has been an exceptional leader, expertly guiding the expansion of HMA’s breadth and depth of expertise so we continue to meet our clients’ needs and exceed their expectations well into the future,” Rosen said. “His passion for serving our clients, supporting our colleagues, and improving the lives of others has made an indelible impact on not only our company but communities across the country.
Elwell will continue to provide consulting services as Senior Advisor to the firm.
Milligan joined HMA as COO in November 2020. A seasoned healthcare leader and consulting executive who has worked with health plans, states, and policy organizations, his contributions span both the public and private sectors.
The United States Government Accountability Office (GAO) appointed Milligan a commissioner to the Medicaid and CHIP Payment and Access Commission (MACPAC) in January 2015, and appointed him vice chairman in May 2019. He has served as the Medicaid director for two states, New Mexico and Maryland.
“Chuck has played an integral role in growing and shaping the multitude of ways we can serve clients by leveraging the varied expertise across all of the organizations within HMA,” Rosen said. “He is a trusted leader, who will spur innovation and propel our partnerships to develop solutions for the toughest healthcare and human services challenges.”
Prior to joining HMA, Milligan served as CEO for UnitedHealthcare’s Community Plan in New Mexico, with accountability for the Medicaid and DSNP lines of business in the state. He also served as interim CEO for UnitedHealthcare’s Community Plan in Maryland, and as national vice president for UnitedHealthcare’s Dual Special Needs Plans. Milligan’s career includes having been senior vice president of Enterprise Government Programs at Presbyterian Healthcare Services and executive director of The Hilltop Institute at University of Maryland, Baltimore County. He began his career as an attorney practicing healthcare law in California.
Meggan Christman Schilkie, currently senior vice president of HMA’s Practice Groups, will assume the role of COO at HMA. She joined HMA in 2014 and has held leadership roles in the firm’s Northeast Region and its New York office.
During her time at HMA, Schilkie has supported clients across the country including providers, associations, state and local governments, payers, large delivery systems and other stakeholders to expand the quality of and access to healthcare with a particular focus on developing new and innovative models of behavioral healthcare.
Prior to joining HMA, Schilkie served as chief program officer for Mental Health at the New York City Department of Health and Mental Hygiene where she oversaw a portfolio of behavioral health services. During her career she has been interim CEO for three health homes in New York serving individuals with serious behavioral health needs, chronic health conditions, intellectual and developmental disabilities and substance use disorders. Schilkie was the founding executive director of the Coalition of New York State Health Homes providing leadership for this statewide provider association.
Medicaid Managed Care Enrollment Update—Q4 2023
This week, our In Focus section reviews recent Medicaid enrollment trends in capitated, risk-based managed care in 30 states.1 Many state Medicaid agencies post monthly enrollment figures by health plan for their Medicaid managed care population on their websites. These data allow for timely analysis of enrollment trends across states and managed care organizations. All 30 states highlighted in this review have released monthly Medicaid managed care enrollment data into quarter four (Q4) of 2023. The analysis that follows reflects the most recent data posted. HMA continues tracking enrollment as states work towards concluding their Public Health Emergency (PHE) unwinding-related redeterminations and resuming normal eligibility operations.
Health Management Associates, Inc., (HMA) has reviewed the Q4 enrollment data (see Table 1) and offers the following observations:
- Across the 30 states tracked in this report, Medicaid managed care enrollment declined by 7.3 percent year-over-year as of December 2023.
- Of the 30 states, 26 experienced decreased enrollment in December 2023, compared with the previous year, as the result of Medicaid redeterminations.
- A total of 23 of the states—Arizona, California, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maryland, Michigan, Minnesota, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, North Carolina, Ohio, Oregon, Pennsylvania, Virginia, Washington, and West Virginia—saw net Medicaid managed care enrollment decrease by 469,000 (0.9%) to 51.5 million members at the end of Q4 2023. (Note: North Carolina expanded Medicaid in December 2023 and was added to the expansion group, in part inflating the change).
- The seven states that had yet to expand Medicaid as of December 2022—Florida, Georgia, Mississippi, South Carolina, Tennessee, Texas, and Wisconsin—have seen Medicaid managed care enrollment decrease 25.2 percent to 13.9 million members at the end of Q4 2023.
Table 1. Monthly MCO Enrollment by State, October 2023−December 2023
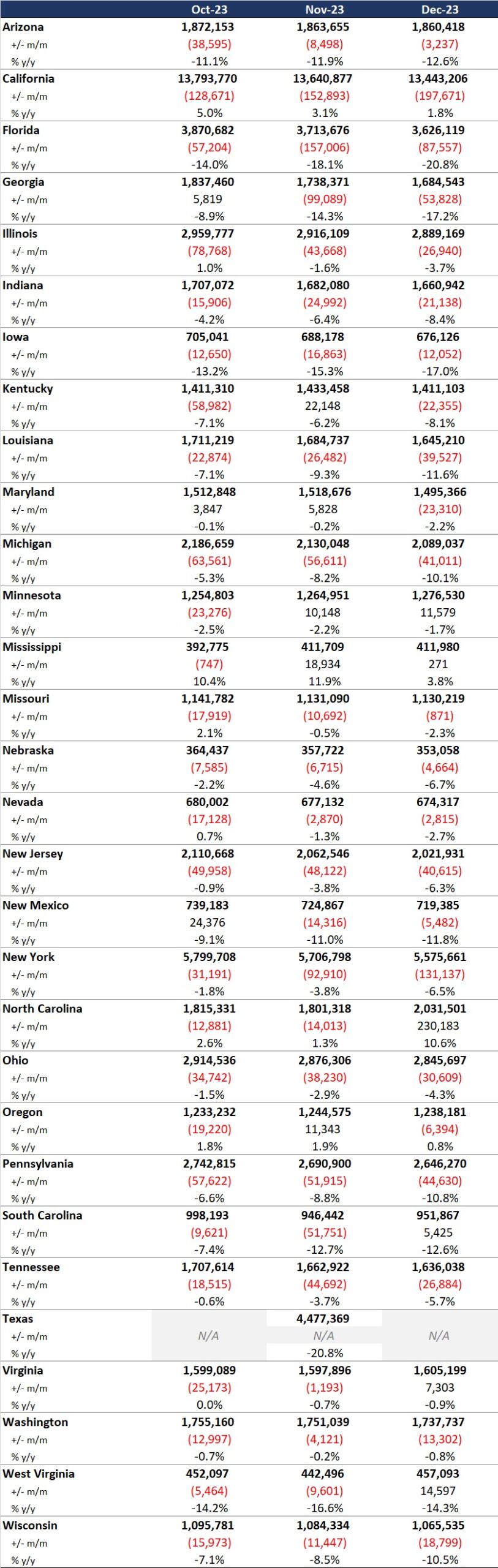
It is important to note the limitations of the data presented. First, not all states report the data at the same time during the month. Some of these figures reflect beginning of the month totals, whereas others provide an end of the month snapshot. Second, in some cases the data are comprehensive in that they cover all state-sponsored health programs offering managed care; in other cases, the data reflect only a subset of the broader managed Medicaid population, making it the key limitation to comparing the data described below and figures that publicly traded Medicaid MCOs report. Consequently, the data in Table 1 should be viewed as a sampling of enrollment trends across these states rather than a comprehensive comparison, which cannot be developed based on publicly available monthly enrollment information.
Expand Your Awareness about Medicaid and Medicare Advantage via HMAIS
If you are interested in gaining access to detailed information on the Medicaid managed care landscape, an HMAIS subscription is the key to unlock important data. The HMA Information Services (HMAIS) collects Medicaid and Medicare Advantage Special Needs Plan (SNP) enrollment data, health plan financials, as well as developments on expansions, waivers, and demonstrations. Your HMAIS login also provides access to a library of public documents all in one place, including Medicaid RFPs, responses, model contracts, scoring sheets and other procurement related materials. HMAIS combines this publicly available information along with HMA expert insights on the structure of Medicaid in each state, as well as a proprietary HMA Medicaid Managed Care Opportunity Assessment.
For information on how to subscribe to HMA Information Services, contact Andrea Maresca [email protected].
Policy and Operational Implications of the Change Healthcare Cyberattack
This week, our second In Focus explores a new Issue Brief published by Leavitt Partners, a Health Management Associates, Inc. (HMA) Company, which addresses the February 21, 2024, cyberattack on Change Healthcare. The cyberattack is one of the most significant on the healthcare industry and has had short-term effects on the entire healthcare sector, with potential for longer-term impacts across the industry.
Because of the ransomware attack, more than 100 applications were taken offline, preventing medical professionals from conducting out many patient-facing activities, including filling prescriptions, managing care plans, and performing prior authorization checks. Six weeks after the crippling cyberattack on Change Healthcare, some systems are still only partially operational and many claims remain unpaid. This situation has disrupted patient access to care and placed significant financial strain on providers.
Change Healthcare is maintaining a daily status report on operations here: https://support.changehealthcare.com/customer-resources/payer-lists In addition, the Department of Health and Human Services (HHS) provided the following resources for providers to work with payers directly: https://healthsectorcouncil.org/wp-content/uploads/2024/03/HHS-Letter-and-Appendix-to-HC-Providers-1.pdf
With billions of dollars in loans and advance payments already disbursed and ongoing investigations into Health Insurance Portability and Accountability Act (HIPAA) violations, the healthcare industry is bracing for long-term impact, while the Administration and Congress are just beginning to act. Leavitt Partners experts, an HMA Company, is monitoring and analyzing the impacts on payers and providers, as well as current and future policy implications.
For more information and to obtain in-depth issue briefs, including “Cyberattacks: Health Care Industry Impacts and the Federal Response,” contact Mark Marciante at [email protected] and Ryan Howells at [email protected].
HMA Roundup
Alabama
Alabama Releases External Quality Review Organization RFP. The Alabama Medicaid Agency released on April 9, 2024, a request for proposals (RFP) seeking a vendor to provide external quality review for the state’s seven Primary Care Case Management entities serving Medicaid beneficiaries. The selected vendor will be required to conduct a systems performance review for the Alabama Coordinated Health Network (ACHN) and evaluate ACHN’s performance measures and performance improvement projects. Proposals are due May 24, 2024, with intent to award on July 12, 2024. The one-year contract will run from November 1, 2024 through October 31, 2025 and have four one-year renewal options. The incumbent is IPRO. Read More
Alabama Disenrolls 17,887 Medicaid Beneficiaries During February Redeterminations. The Alabama Daily News announced on April 16, 2024, that Alabama disenrolled 17,887 individuals during February eligibility redeterminations. The state did not specify the reasons for disenrollment. The state has disenrolled nearly 186,000 beneficiaries since redeterminations began in June 2023. Read More
Arkansas
Arkansas Awards CSG Government Solution IV&V Contract. The Arkansas Department of Human Services announced on April 11, 2024, its intent to award the Independent Verification and Validation (IV&V) Services for the Arkansas Medicaid Enterprise Systems to CSG Government Solution Inc. The contract is set to begin on July 1, 2024, and will run for three years with up to four one-year renewal options. Read More
Connecticut
Connecticut Submits Section 1115 Substance Use Disorder Demonstration Amendment. The Centers for Medicare & Medicaid Services announced on April 12, 2024, that Connecticut has submitted an amendment for its Substance Use Disorder Section 1115 demonstration, which aims to address health-related social needs for the state’s justice-involved individuals. The state is requesting to provide Medicaid services for certain individuals 90 days prior to release from the correctional system and a 30-day supply of medications upon release along with other supportive services. The amendment also includes Medicaid coverage for inmates who have behavioral health disorders or are incarcerated youth. The federal public comment period is open through May 13. Read More
Delaware
Delaware Supreme Court Overturns Rule Preventing State Retirees From Joining MA Plans. The Associated Press reported on April 12, 2024, that Delaware’s Supreme Court has overturned a prior court ruling that prevented the state from moving government retirees from a Medicare supplement plan to a Medicare Advantage plan. The justices cited that the selection of a particular Medicare plan is not a regulation subject to Administrative Procedures Act (APA) notice and public hearing requirements, and the judge therefore had no jurisdiction under the APA to halt the plan. Read More
Florida
Florida Announces Awards for Statewide Medicaid Managed Care Procurement. The Florida Agency of Health Care Administration announced on April 12, 2024, its intention to award Statewide Medicaid Managed Care program contracts to five incumbent plans: Florida Community Care, Humana, Elevance/Simply Healthcare Plans, South Florida Community Care Network/Community Care Plan, and Centene/Sunshine State Health Plan, down from the current nine plans. As part of this procurement, the state consolidated the number of regions from eleven to nine. Florida Community Care will serve Regions A, B, C, D, and I while South Florida Community Care Network will serve Regions E, F, G, H, and I. The other three plans were awarded statewide contracts. All plans also received at least one specialty plan award (see data package below). The program serves approximately 3.4 million individuals, and the consolidation of regions will impact the enrollment opportunity for successful bidders. The contracts are set to run from October 1, 2024, through December 31, 2030. Current contractors CVS/Aetna, Molina Healthcare, UnitedHealthcare, and AmeriHealth Caritas did not secure contracts nor did new bidders Sentara Care Alliance and ImagineCare, a joint venture between CareSource and Spark Pediatrics. Read More
Florida Medicaid Redeterminations Lawsuit Trial Scheduled for May. NBC 6 South Florida reported on April 16, 2024, that a federal judge has scheduled a trial date of May 13 for a class action lawsuit, filed by Florida residents, that alleges the state did not provide sufficient notice prior to terminating Medicaid coverage during redeterminations. The suit claims Florida violated federal Medicaid law and Medicaid beneficiaries’ due-process rights. The lawsuit, previously filed in August, added two additional plaintiffs in January. Read More
Florida Disenrolls 1.4 Million Medicaid Beneficiaries Since Redeterminations Began. The Florida Agency for Health Care Administration reported that the state has disenrolled approximately 1.4 million Medicaid enrollees from April 2023 through February 2024. Of those, 614,119 lost coverage due to ineligibility and 813,493 lost coverage due to procedural reasons.
Idaho
Idaho Legislature Adjourns Without Amending Medicaid Waiver Bill. Spokane Public Radio reported on April 12, 2024, that the Idaho Legislature adjourned without amending a bill that requires legislative approval for Medicaid Section 1115 and Section 1915 waivers. Governor Brad Little previously asked the legislature to amend the bill to avoid disruption in funding for related services. Read More
Kansas
Kansas Delays KanCare, CHIP Medicaid Managed Care RFP Awards. Health Payer Specialist reported on April 15, 2024, that Kansas has delayed announcing awards for its KanCare Medicaid & CHIP capitated managed care contracts, originally scheduled for April 12. The state did not provide a new date for announcing the awards. Incumbents UnitedHealthcare, Centene, and CVS/Aetna filed bids along with non-incumbents CareSource, Molina Healthcare, UCare, and Blue Cross and Blue Shield of Kansas. Read More
Mississippi
Mississippi Study to Test Food is Medicine Pilot Program. Modern Healthcare reported on April 17, 2024, that researchers will evaluate a food prescription program launched in the rural Mississippi Delta region. The pilot, slated to run for one year, focuses on regional farmers who can supply fresh fruit and vegetables to patients with diabetes via the Delta Health Center. Dubbed Delta GREENS (Growing a Resilient, Enriching, Equitable, Nourishing food System), the program is designed to address food insecurity and assess the impact of integrating food into healthcare programs. Results from the program may help inform future reimbursement policies for similar food as medicine programs offered by public healthcare programs such as Medicaid. Read More
Mississippi Receives Federal Approval for Medicaid Reimbursement Reform Plan. The Magnolia Tribune reported on April 11, 2024, that Mississippi Governor Tate Reeves announced that the Centers for Medicare & Medicaid Services approved a second component of the state’s Medicaid reimbursement reform plan. Under the approved proposal, Medicaid base payment rates for hospitals will be supplemented by reimbursing inpatient and outpatient hospital services in the fee-for-service system up to the Medicare upper payment limit, which is estimated to result in an additional $160 million for hospitals annually. The two approved initiatives are estimated to generate over $700 million in new revenue for hospitals in Mississippi. Read More
Nevada
Nevada Proposes New Behavioral HCBS Program for Children. The Nevada Department of Health and Human Services announced on April 9, 2024, a proposal that seeks to prevent unnecessary institutionalization of children in foster care and children with significant behavioral health needs. The program would connect approximately 10,000 to 15,000 beneficiaries to a new Medicaid-funded home-and-community based services program. The first stage of implementation is slated for April 2024, the second for June 2024, and the third between 2024 and 2026. Nearly $200 million in state and federal Medicaid funds would be invested in the program by the end of the third year.
New York
New York Governor Announces Fiscal 2025 State Budget Agreement with Legislature. New York Governor Kathy Hochul announced on April 15, 2024, a conceptual agreement with legislators on the fiscal 2025 state budget, which is currently estimated at $237 billion. The budget includes an investment of $7.5 billion in the health care system over the next three years via an amendment to the state’s Medicaid Section 1115 demonstration; a $20 billion multi-year investment to build new healthcare infrastructure, expand Medicare coverage, and increase wages for home care workers; and Medicaid savings from reform to fiscal intermediaries and stricter regulation of the Consumer Directed Personal Assistance Program. Additionally, the proposed agreement allots $19 million for mental health services for school-aged children, $55 million to establish 200 new inpatient psychiatric beds at state-run facilities, and $31 million to expand mental health services for first responders and justice-involved individuals. Other key highlights include authority for the state to request and implement a managed care organization tax, Medicaid rate increases for hospitals and nursing homes, and additional cuts totaling an estimated $800 million. The conceptual agreement will guide the work of the legislative bodies to pass bills advancing these priorities. Read More
New York CDPAP Program May Transition to Single Fiscal Intermediary. CBS 6 Albany reported on April 16, 2024, that New York’s Consumer Directed Personal Assistance Program (CDPAP), which allows representatives for individuals with cognitive disabilities to select their own home health providers, may transition to utilizing a single fiscal intermediary under the New York budget agreement. Currently, the state has more than 300 fiscal intermediaries that handle billing and human resource concerns. Read More
New York Disenrolls 1.4 Million Medicaid Beneficiaries Since Redeterminations Began. The New York Department of Health reported that the state has disenrolled approximately 1.4 million Medicaid enrollees from June 2023 through February 2024. Of those, 749,342 lost coverage due to ineligibility and 619,072 lost coverage due to procedural reasons.
North Carolina
North Carolina Backs Lawsuit to Block Novant Health’s Acquisition of Two Community Health Systems Hospitals. Rueters reported on April 16, 2024, that North Carolina filed a “friend of the court” brief backing the Federal Trade Commission’s (FTC) lawsuit to block Novant Health’s $320 million acquisition of two hospitals in North Carolina from Community Health Systems. An administrative hearing before the FTC to determine the legality of the proposed transaction is scheduled for June 26. Read More
Ohio
Ohio Submits Extension for Section 1115 Substance Use Disorder Demonstration. The Ohio Department of Medicaid submitted on April 1, 2024, a request to the Centers for Medicare & Medicaid Services to extend its Section 1115 Substance Use Disorder demonstration program for an additional five years. The demonstration allows the state to enhance residential treatment services via federal funding for treatment in Institutions for Mental Diseases and increases support for individuals in the community and home outside of institutions. The current demonstration expires September 30, 2024. The federal public comment period is open through May 11. Read More
MCOs Fund Community-based Programs Under NextGen Model. The Courier announced on April 9, 2024, that Ohio’s Medicaid managed care organizations (MCOs) are investing in several programs throughout southeast Ohio as a part of the Ohio Department of Medicaid’s Next Generation of Managed Care (NextGen) model, designed to provide person-centered care. MCOs will reinvest a portion of their contract proceeds to community-based programs that address social determinants of health. Each plan consulted with population health and health equity teams to choose projects to invest in, which include food pantries, school-based clinics, rural health programs, and programs supporting disadvantaged or uninsured individuals. Read More
Texas
Texas Disenrolls More Than 2 Million Medicaid Beneficiaries During Redeterminations Through March. The Texas Health and Human Services Commission reported that state has disenrolled nearly 2.1 million Medicaid beneficiaries between April 2023 and March 2024 during Medicaid redeterminations. Of those disenrolled, 1.4 million were due to procedural reasons. Over 1.3 million children were disenrolled. The state has renewed coverage for more than 2.1 million beneficiaries, and has 202,467 pending eligibility cases. Read More
West Virginia
West Virginia Medicaid Program Will Face Funding Cuts Beginning in July. The Mountain State Spotlight reported on April 11, 2024, that West Virginia officials will cut the state’s Medicaid budget beginning in July after lawmakers allotted the program approximately $394 million for fiscal 2025, $150 million less than what was needed. Services that could be cut include hospice care, dental care, physical therapy, speech therapy, and in-home care for people with disabilities and prescription drugs. Read More
Wisconsin
Wisconsin Committee Blocks $258 Million HCBS Funding Proposal. The Wisconsin Examiner reported on April 11, 2024, that the Wisconsin Joint Finance Committee has blocked a $258 million plan which would set a minimum Medicaid fee schedule for long-term home health care providers serving individuals with intellectual disabilities, physical disabilities, or over age 65 needing a nursing home level of care. The proposal would also cover services for people enrolled in Medicaid-funded home and community-based long-term care programs. The committee cited that the proposal would create a $500 million increase in next year’s budget for long-term care Medicaid funding. Read More
National
CMS Proposed IPPS, LTCH Rule to Increase Certain Acute Care Hospitals’ Payments by 2.6 Percent in 2025. The Centers for Medicare & Medicaid Services (CMS) announced on April 10, 2024, a proposed rule which would increase certain acute care hospitals’ payment rates by 2.6 percent in fiscal 2025. Qualifying hospitals include those that receive CMS payments under the IPPS (Inpatient Prospective Payment System); successfully participate in the Hospital Inpatient Quality Reporting program; and are “meaningful” electronic health record users. It is projected that hospitals would receive an increase in payments of $3.2 billion. CMS is also proposing a 1.6 percent rate increase for long-term care hospitals (LTCHs) in 2025. Read More
CMS Proposes Transforming Episode Accountability Model to Improve Care During Surgery, Recovery for Medicare Beneficiaries. The Centers for Medicare & Medicaid Services (CMS) announced on April 10, 2024, the proposed Transforming Episode Accountability Model (TEAM), a five-year mandatory model that seeks to incentivize care coordination between care providers during surgery as well as the services provided in the 30 days following a procedure. The model aims to improve quality of care, reduce rehospitalization and recovery time, and lower spending. Participating hospitals would receive a target price to cover costs associated with a month-long episode of care. TEAM would run from January 1, 2026, through December 31, 2030. TEAM is a part of the Fiscal Year 2025 Inpatient and Long-Term Care Hospital Prospective Payment Systems Rule, which has a 60-day public comment period through June 10. Read More
CMS Anticipates Additional Prior Authorization Rules in the Future. Modern Healthcare reported on April 15, 2024, that the Centers for Medicare & Medicaid Services (CMS) is considering taking further action on relaxing prior authorization requirements. The actions were previewed by CMS Administrator Chiquita Brooks-LaSure at the American Hospital Association’s annual conference. Read More
CMS Releases Resources to Promote Quality Improvement in Medicaid HCBS. The Centers for Medicare & Medicaid Services (CMS) released on April 11, 2024, three resources to promote quality improvement within Medicaid-funded home and community-based services (HCBS). These include the 2024 HCBS Quality Measure Set, as well as the HCBS Quality Measure Set Reporting Requirements for Money Follows the Person Demonstration Grant Recipients to address requirements and expectations for relevant populations, timeframes, and more. CMS additionally released the 2024 Long-Term Services and Supports Quality Measures Technical Specifications and Resource Manual, which provides measures for Medicaid fee-for-service delivery systems that correspond with measures for managed care programs. Read More
Medicare Telehealth Utilization Decreased in 2022; Does Not Limit Access to In-person Care, MedPAC Finds. Health Payer Specialist reported on April 15, 2024, that the Medicare Payment Advisory Commission (MedPAC) released a report that found that telehealth usage decreased in 2022 and has not limited access to in-person care for Medicare beneficiaries. In 2022, one percent of non-behavioral providers offered telehealth-only services, while 90 percent offered exclusively in-person appointments. Behavioral health providers were most likely to provide telehealth services. Read More
Congress Holds Hearing on Expiring Medicare Telehealth Policies. CQ News reported on April 10, 2023, that Congress held a hearing to address pandemic-era Medicare telehealth policies that are set to expire December 31, 2025. The provisions that several lawmakers seek to extend include Medicare coverage of audio-only telehealth services and expanding the types of providers who can bill Medicare for telehealth services. It is estimated that the cost of expanding telehealth coverage will be around $3 billion per year. Read More
More Than 20 Percent of Medicaid Beneficiaries Disenrolled During Redeterminations Are Uninsured, KFF Survey Finds. KFF released on April 12, 2024, a survey showing that nearly 23 percent of adults who were disenrolled from Medicaid during redeterminations are now uninsured and about 70 percent were left temporarily uninsured. Approximately 28 percent of those disenrolled have enrolled in another form of health coverage, and about half have re-enrolled in Medicaid. Additionally, more than half of individuals who tried to re-enroll experienced at least one problem during the process. Read More
HUD Proposes to Reduce Barriers to Public Housing for Justice-involved Tenants. The Department of Housing and Urban Development (HUD) proposed on April 9, 2024, a rule which would ban public housing agencies and owners of HUD-assisted multifamily housing from denying access to or terminating someone from housing for having a criminal record. Under the Reducing Barriers to HUD-assisted Housing rule, agencies and owners will need to use an individualized assessment that only considers criminal records relevant to endangering health and safety of staff and residents. The public comment period will be open through June 10. Read More
Eight Governors Urge Biden Administration to Reconsider Changes to Medicaid Provider Tax Policy. Newsweek reported on April 12, 2024, that eight governors have sent a letter to President Joe Biden urging his Administration to reconsider its plans to change the approaches states may use to fund the non-federal share of Medicaid payments and increase oversight of how provider taxes are used. The governors argue that the change will result in a costly administrative burden and could reduce Medicaid funding by $48 billion each year for states relying on provider taxes. Read More
Industry News
Accenture Federal Services to Acquire Cognosante. Accenture Federal Services announced on April 16, 2024, that it has entered into an agreement to acquire Cognosante, a provider of technology solutions for federal agencies. Terms of the acquisition were not disclosed. Read More
Elevance Health to Acquire New York Managed Long Term Care Plan. Empire Center reported on April 11, 2024, that Elevance Health reached a deal to purchase New York-based Medicaid managed long-term care plan Centers Plan for Health Living, and affiliate Centers for Specialty Care Group. The deal is expected to close in the third quarter of 2024. A sale price has not been disclosed. Read More
Elevance, Clayton, Dubilier & Rice Invest in Primary Care Access Partnership. Elevance Health announced on April 15, 2024, that it has made an investment with private equity firm Clayton, Dubilier & Rice (CD&R) in a partnership aiming to expand access to advanced primary care for consumers with coverage across commercial, individual Marketplace, Medicaid, and Medicare health plans. The effort will utilize certain care delivery and enablement assets of Elevance Health’s Carelon Health and CD&R portfolio companies, Apree health and Millennium Physician Group. The investment will be through cash and equity interest. Financial terms were not disclosed. Read More
Kaiser Permanente Launches Food Is Medicine Center. Modern Healthcare reported on April 11, 2024, that Kaiser Permanente launched the Food is Medicine Center of Excellence, which will expand food and nutrition scanning methods, partnerships, and clinical training, and will serve as a research hub to analyze food-is-medicine programs. Kaiser has recently launched several food-is-medicine initiatives, including a partnership with food delivery service Instacart. Read More
Prime Healthcare Finalizes Acquisition of Five Medical Properties Trust New Jersey, California Hospitals. Modern Healthcare reported on April 10, 2024, that Prime Healthcare finalized its $350 million acquisition of five New Jersey and California hospitals from Medical Properties Trust. The transaction consists of $250 million in cash and a $100 million interest-bearing mortgage note due to the real estate investment trust in nine months. Prime Healthcare currently operates 44 hospitals across 14 states. Read More
Clinicians from Telehealth Provider Bicycle Health Vote to Unionize. Behavioral Health Business reported on April 15, 2024, that clinicians at Massachusetts-based Bicycle Health, a digital substance use disorder provider, voted to unionize with the Union of American Physicians and Dentists. Read More
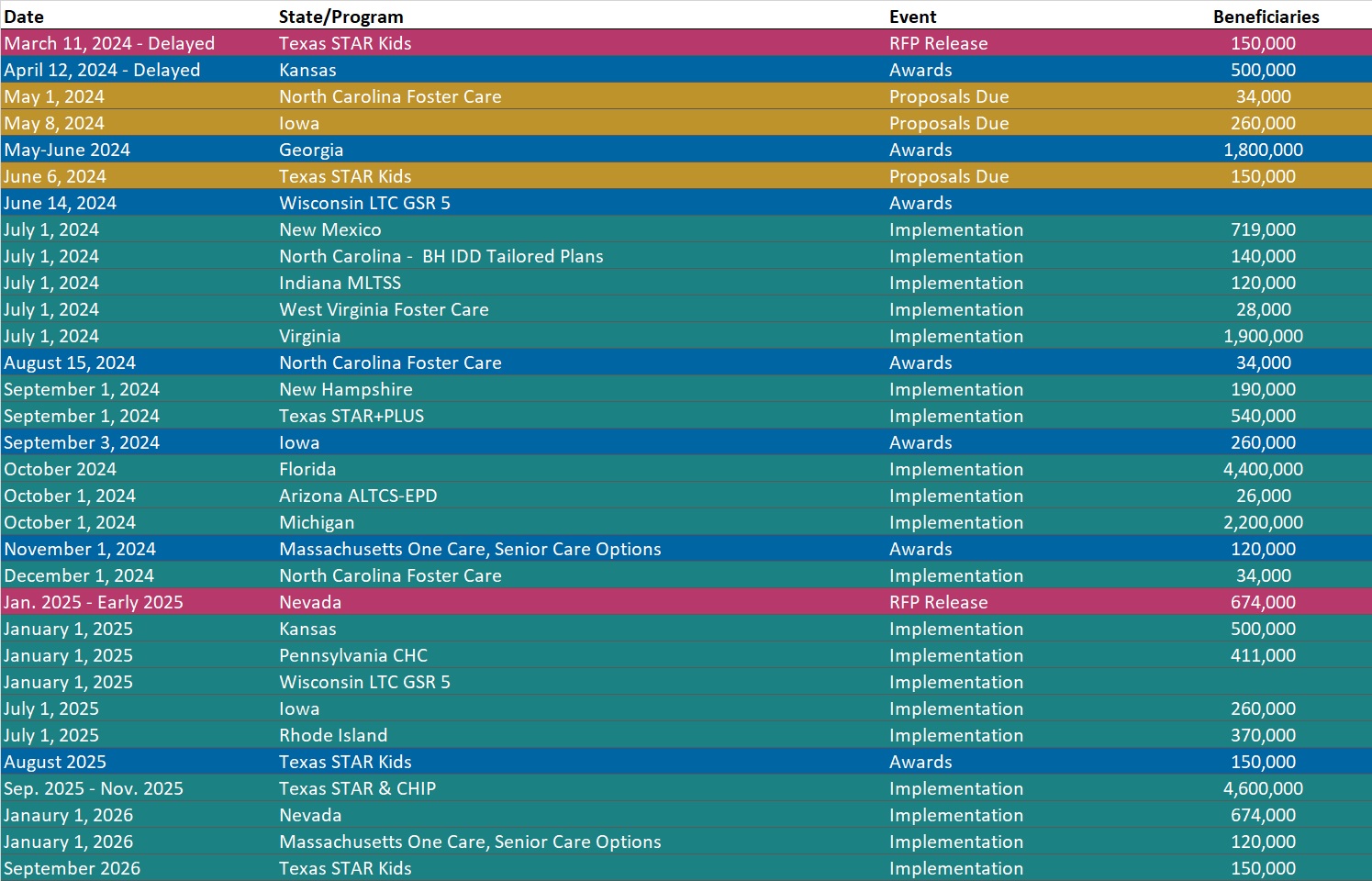
RFP Calendar
HMA News & Events
HMA Webinars:
Equity Considerations for Addressing Opiate Use Disorder. Tuesday, April 23, 2024, 1 PM ET. Nationally, we are seeing trending disparities in opioid use disorder prevalence and overdose deaths—whether it be brown and black communities or pregnant and parenting people. We will overview 3 projects that demonstrate how HMA has partnered with States and Counties to address opioid use disorder with an equity focus. Register Here
Substance Use Disorder (SUD) Ecosystem of Care: Building Systems-Thinking in the SUD Ecosystem. Wednesday, May 1, 2024, 12 PM ET. The final webinar of this three-part series emphasizes the importance of a comprehensive and interconnected spectrum of engagement and treatment strategies. To truly build and maintain an SUD ecosystem with accountability across the system and ‘no wrong door,’ best practices must embrace a systems-thinking approach. An interconnected system requires building strong partnerships across the SUD ecosystem and engagement and treatment strategies will focus on leveraging those partnerships to facilitate engagement of individuals throughout the system. Register Here
Wakely, an HMA company, Webinars and White Papers:
How the New MA/PD Risk Models & Post-IRA Part D Benefit are Changing the View of Medicare Profitability. Monday, April 22, 2024, 3 PM ET. Medicare risk scores continue to evolve, with increasing weight given to the MA’s 2024 v28 HCC risk score model and the introduction of a new post-IRA RxHCC risk score model for payment year 2025. In addition, basic Part D benefit costs are expected to change dramatically due to the overhaul of the Part D defined standard benefit in 2025 as part of the Inflation Reduction Act. These key changes to the Medicare Advantage and Part D programs have the potential to cause material shifts in the revenue, claims, and the drivers of profit/loss for MA/PD plans. This raises the question: how will the profiles for historically profitable/unprofitable members change in 2025 & beyond? Wakely has conducted in-depth analyses to explore the impact of risk score model changes and 2025 Part D defined standard benefit changes has on the overall profitability of certain MA-PD cohorts. In this webinar, we will share an overview of some of the results and discuss how plans can potentially use this analysis to inform strategies. Register Here
Summary of CY2025 Medicare Advantage Final Rate Announcement. Wakely has summarized how the CMS CY2025 Final Rate Announcement will impact Medicare Advantage plans in 2025, including analysis of the average revenue impact.
- Understand what proposals from the CY2025 Medicare Advantage Advance Notice have and have not changed in the Final Announcement.
- Get Wakely’s estimate of national average MA revenue impact for 2025. Read More
ICHRA/QSEHRA Consideration for Pricing Actuaries. ICHRAs and QSEHRAs present both challenges and opportunities for health plans. Given the potential advantages such ICHRAs could have for employers, the Departments of Labor, Health and Human Services, and Treasury estimated that by 2029 around 800,000 employers will offer ICHRAs and approximately 11.4 million individuals will receive ICHRAs. Understanding their impact on the I&SG market is crucial for actuaries to develop effective product strategies and pricing models in the evolving healthcare landscape. This whitepaper discusses pricing implications of the rising popularity of Individual Coverage Health Reimbursement Arrangements (ICHRAs) and Qualified Small Employer Health Reimbursement Arrangements (QSEHRAs). Read More
The Importance of Care Management and Quantifying Savings. Care management programs coordinate healthcare delivery, improve patient outcomes, and optimize utilization of care. Health insurers and benefit vendors alike are implementing these programs with goals to optimize outcomes and achieve savings. Savings can be achieved through the reduction of bottom-line costs using tailored services and reducing waste, or through increased top-line revenue by capturing a more accurate representation of risk in the underlying population. The challenge lies in isolating and quantifying the savings specific to implementation of these programs. There are a variety of analyses and studies that can be utilized to demonstrate their impact. Performing these studies is critical for evaluating these programs and continuing to improve healthcare and outcomes. Read More
Medicaid Profitability During the Public Health Emergency. The pandemic is widely viewed as a windfall for insurers because of the decrease in the utilization of healthcare. It is less well understood how profitability trended in Medicaid managed care. The purpose of this report is to see how managed Medicaid health plans fared financially in 2020-2022 compared to prior years. Our findings show that while margin did increase, the Medicaid margin levels were explainable, and not abnormal relative to other lines of business experience. Read More
