HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Medicaid Managed Care Spending in 2023

- Colorado Receives Feedback on Behavioral Health Administrative Service Organizations; RFP Expected Spring 2024

- Idaho House Committee Advances Bill to Expand Postpartum Medicaid Coverage to 12 Months

- Iowa Releases Health Link Medicaid Managed Care RFP to Reprocure One Contract

- Maryland Faces $236 Million Medicaid Budget Shortfall

- Minnesota Requests Additional Five-year Extension of Substance Use Disorder Reform Demonstration

- Mississippi Legislature Passes Bill that Would Grant Early Medicaid Coverage for Pregnant Women

- Nebraska Waiver Expands HCBS to 850 Children on Developmental Disabilities Registry

- Nevada Holds Workshop on Medicaid Managed Care Procurement

- New York Receives Federal Approval for Section 1332 State Innovation Waiver to Expand Essential Plan Eligibility

- Oregon CCOs to Offer Grant Funding to Support Community Organizations in HRSN Delivery

- Pennsylvania Releases Electronic Visit Verification Module RFP

- Tennessee to Release Pharmacy Benefits Administrator RFP in Fourth Quarter of 2024

- Virginia Announces Awards for Statewide Medicaid Managed Care Procurement

- Biden Administration Takes Steps to Prevent Corporate Overcharging of Consumers, Government Programs

- Federal Regulators Launch Investigation into Private Equity Healthcare Deals

- United Health Group Provides Temporary Funding, Pharmacy System During Cyber Attacks

- The Ensign Group Acquires Skilled Nursing Facilities in Colorado, Kansas

In Focus
Medicaid Managed Care Spending in 2023
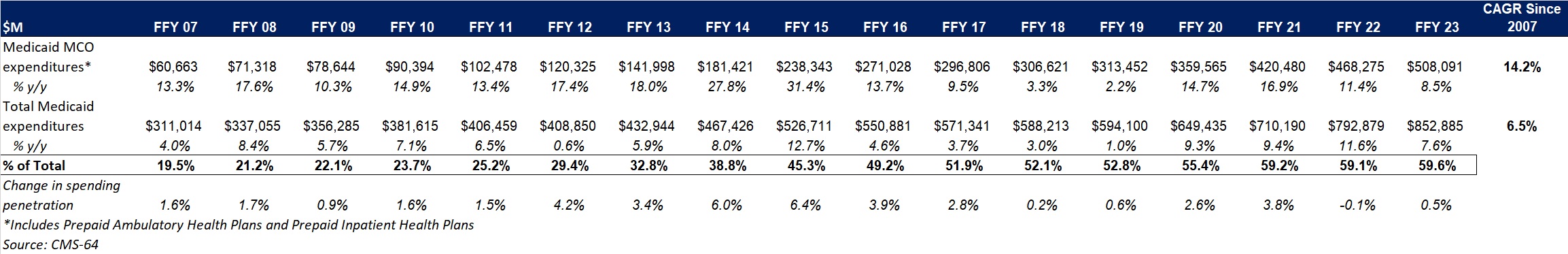
This week, our In Focus section analyzes preliminary 2023 Medicaid spending data collected in the annual CMS-64 Medicaid expenditure report. After submitting a Freedom of Information Act request to the Centers for Medicare & Medicaid Services (CMS), HMA received a draft version of the CMS-64 report that is based on preliminary estimates of Medicaid spending by state for federal fiscal year (FFY) 2023. Based on the preliminary estimates, Medicaid expenditures on medical services across all 50 states and six territories in FFY 2023 totaled nearly $852.9 billion, with 59.6 percent of that amount now flowing through Medicaid managed care programs. In addition, total Medicaid spending on administrative services was $33.8 billion, bringing total program expenditures to $886.7 billion.
Total Medicaid Managed Care Spending
Total Medicaid managed care spending (including the federal and state share) in FFY 2023 across all 50 states and six territories was $508.1 billion, up from $468.3 billion in FFY 2022. This figure includes spending on comprehensive risk-based managed care programs as well as prepaid inpatient health plans (PIHPs) and prepaid ambulatory health plans (PAHPs). PIHPs and PAHPs refer to prepaid health plans that provide only certain services, such as dental or behavioral health care. Fee-based programs such as primary care case management (PCCM) models are not included in this total. Following are some key observations.
- Total Medicaid managed care spending grew 8.5 percent in FFY 2023.
- Managed care spending growth has decreased in since the end of the COVID-19 pandemic, after peaking in FFY 2021.
- In terms of dollars, the increase in Medicaid managed care spending from FFY 2022 to FFY 2023 was $39.8 billion, compared with $47.8 billion from FFY 2021 to FFY 2022.
- Medicaid managed care spending has increased at a compounded annual growth rate (CAGR) of 14.2 percent since FFY 2007, compared with a 6.5 percent growth in total Medicaid spending.
- Compared with FFY 2022, Medicaid managed care spending as a percent of total Medicaid spending in FFY 2023 increased by 0.5 percentage points to 59.6 percent.
Table 1. Medicaid MCO Expenditures as a Percentage of Total Medicaid Expenditures, FFY 2007−2023 ($M)
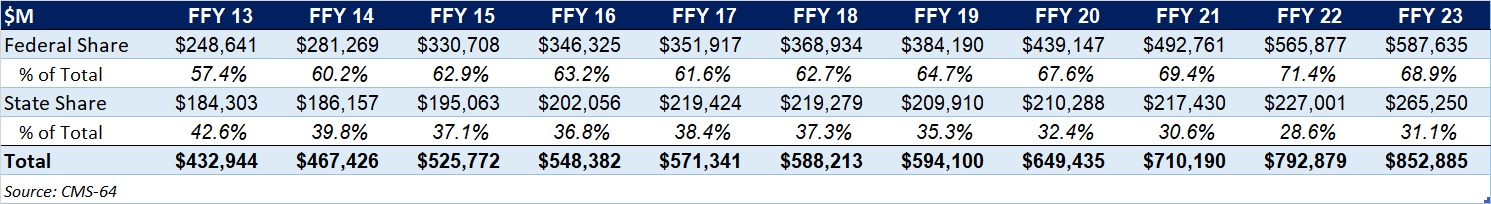
As the table below indicates, 68.9 percent of FFY 2023 spending came from federal sources, which is 11.5 percentage points higher than the pre-Medicaid expansion share in FFY 2013 and 1.3 percentage points higher than FFY 2020.
Table 2. Federal versus State Share of Medicaid Expenditures, FFY 2013−2023 ($M)
State-Specific Growth Trends
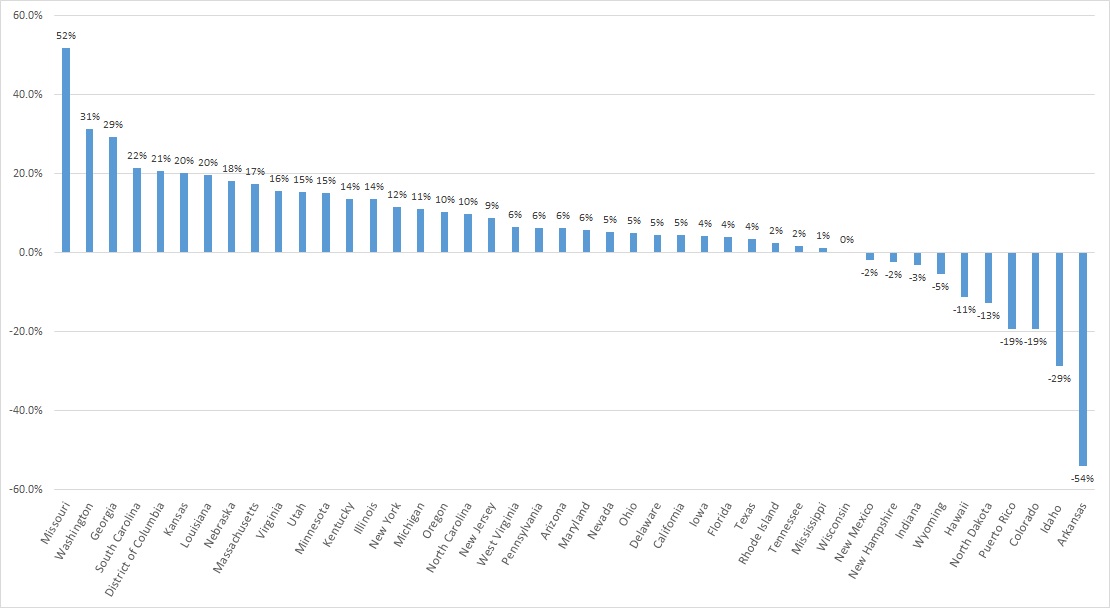
A total of 44 states and territories report managed care organization (MCO) spending in the CMS-64 report. Average MCO spending during FFY 2023 increased 8.5 percent. On a percentage basis, Missouri experienced the highest year-over-year growth in Medicaid managed care spending at 51.7 percent, followed by Washington at 31.4 percent and Georgia at 29.3 percent.
The chart below provides additional detail on Medicaid managed care spending growth in states with risk-based managed care programs in FFY 2023.
Figure 1. Medicaid Managed Care Spending Growth on a Percentage Basis by State, FFY 2022-2023
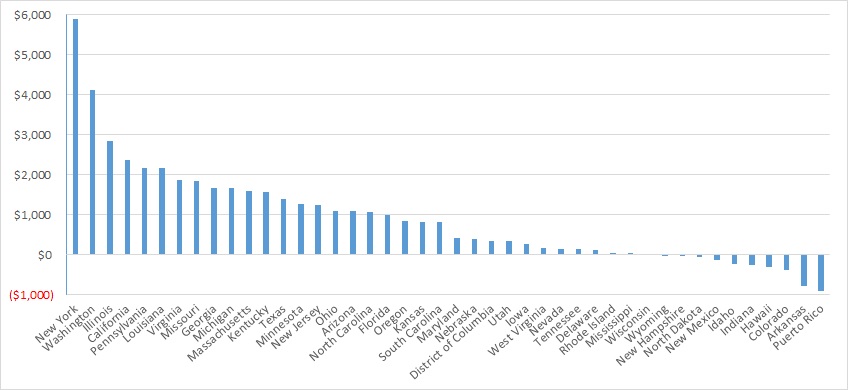
Looking at year-over-year spending growth in terms of dollars, New York experienced the largest increase in Medicaid managed care spending at $5.9 billion. Other states with significant year-over-year spending increases included Washington ($4.1 billion), Illinois ($2.8 billion), and California ($2.4 billion). The chart below illustrates the year-over-year change in spending across the states.
Figure 2. Medicaid Managed Care Spending Growth on a Dollar Basis by State, FFY 2022−2023 ($M)
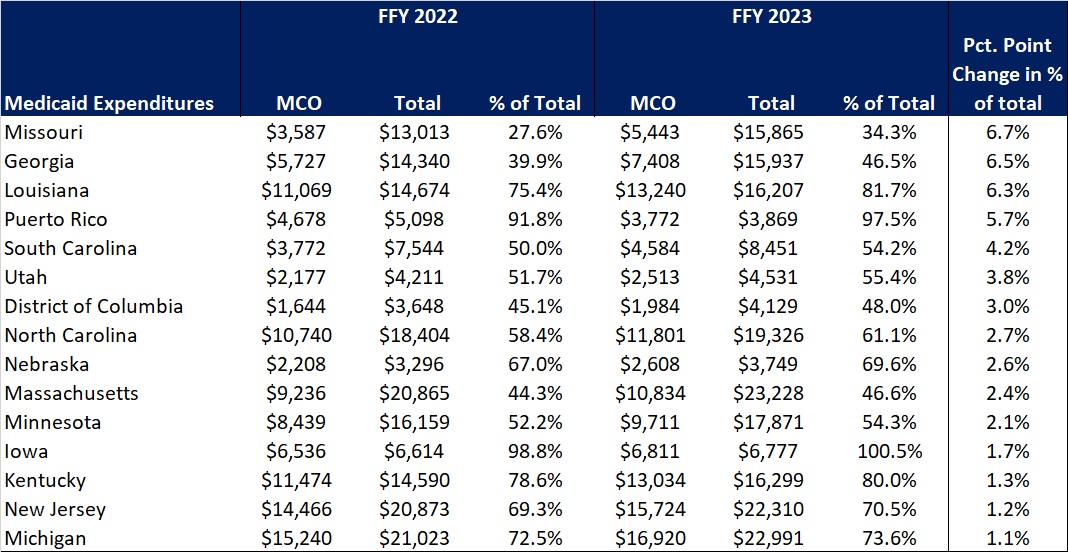
The percentage of Medicaid expenditures directed through risk-based Medicaid MCOs increased by more than one percentage point in 15 states from FFY 2022 to FFY 2023. The managed care spending penetration rate rose 6.7 percentage points in Missouri, 6.5 percentage points in Georgia, 6.3 percentage points in Louisiana, and 5.7 percentage points in Puerto Rico. In all, 22 states saw a decrease in managed care penetration from FFY 2022 to FFY 2023.
Table 3. Medicaid MCO Expenditures as a Percentage of Total Medicaid Expenditures in States with a One percent or Greater Increase from FFY 2022 to FFY 2023 ($M)
The table below ranks the states and territories by the percentage of total Medicaid spending through Medicaid MCOs. Iowa reported the highest percentage at 100 percent, followed by Puerto Rico at 97.5 percent and Kansas at 94.5 percent.
In many states, certain payment mechanisms may never be directed through managed care, such as supplemental funding sources for institutional providers and spending on retroactively eligible beneficiaries. As a result, the maximum achievable penetration rate in each state will vary and may be below the amount achieved in other states. The Medicaid managed care spending penetration rate is greatly influenced by the degree to which states have implemented managed long-term services and supports (MLTSS) programs.
Table 4. Medicaid MCO Expenditures as a Percent of Total Medicaid Expenditures, FFY 2016-2023
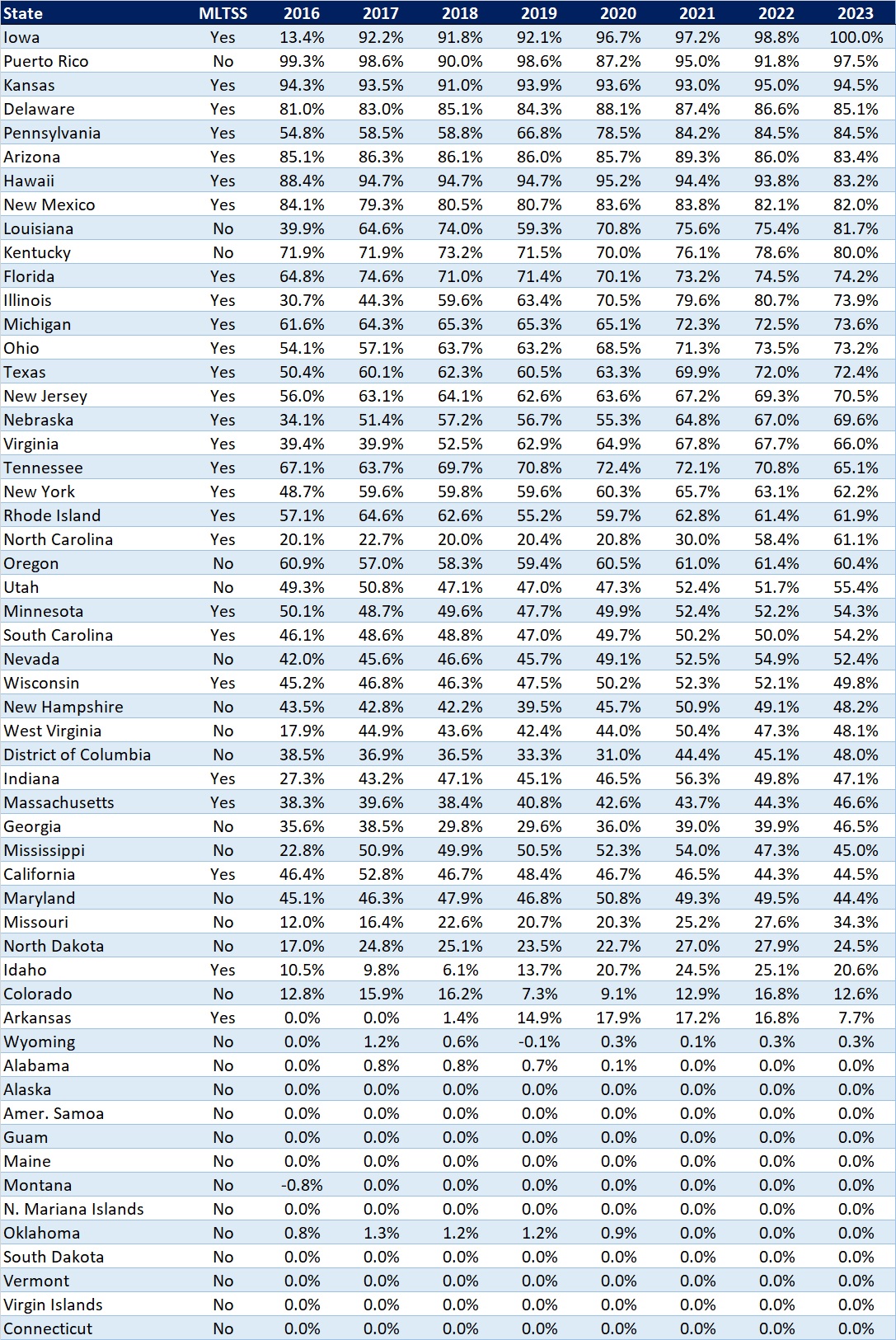
Note: Washington was excluded from the data table.
If you’re interested in becoming an HMAIS subscriber and for access to the CMS-64 data, contact Andrea Maresca at [email protected].
HMA Roundup
Alabama
Alabama Releases Third Party Liability Services RFP. The Alabama Medicaid Agency released on March 5, 2024, a request for proposals (RFP) seeking a vendor to provide Third Party Liability services, including identification of third party insurance leads for cost saving and recovery purposes, recovery of money and benefits, and investigation of cases with liable third party resources. Responses are due April 26, 2024, with intent to award on June 21, 2024. The two-year contract will run from October 1, 2024 through September 30, 2026, and will have three one-year renewal options. The incumbent is Health Management Systems/Gainwell Technologies. Read More
Colorado
Colorado Legislators Consider Bill to Expand Medicaid Funding of Housing, Nutrition Services. Colorado House Democrats reported on March 5, 2024, that Colorado legislators are considering a bill, sponsored by Representative Shannon Bird (D-Westminster) and others, that would direct the Colorado Department of Health Care Policy & Financing to conduct a feasibility study and apply for a Section 1115 demonstration waiver to expand Medicaid funding for housing and nutrition services. Specifically, the bill aims to redirect federal funding to increase access to nutritious food options and secure housing. The bill has been referred to the House Committee on Appropriations. Read More
Colorado Receives Feedback on Behavioral Health Administrative Service Organizations; RFP Expected Spring 2024. The Colorado Behavioral Health Administration (BHA) announced on February 29, 2024, that it has received feedback from behavioral health professionals, advocates, providers, and other partners in response to a request for information released last year in preparation to establish a new behavioral health system, known as Behavioral Health Administrative Service Organizations (BHASOs). BHASOs would consolidate substance use disorder treatment services, crisis services, and would include services offered by Community Mental Health Centers. The feedback included suggestions to emphasize the perspectives of community and underserved populations, focus on early intervention and social determinants of health, promote telehealth, and clearly designate roles, requirements, and quality measurement in the development of BHASOs. A request for proposals seeking vendors for the new system is anticipated to be released Spring 2024 and the system is expected to launch by July 2025. Read More
Colorado Faces Federal Complaint Regarding Disenrollment of Medicaid Beneficiaries with Disabilities. The Colorado Sun reported on February 28, 2024, that the Colorado Center on Law and Policy and the National Health Law Program have filed a complaint against Colorado Medicaid, alleging that the program has violated the rights of beneficiaries with disabilities amid shifts in the program’s case management policies, computer system, and eligibility redeterminations. The complaint asks that the U.S. Department of Health and Human Services Office for Civil Rights and the U.S. Department of Justice intervene to pause the next phase of the state’s three-phase case management transition, slated for March 1, and halt Medicaid termination of beneficiaries with disabilities until case management and technological issues are resolved. Colorado indicated efforts to find solutions, including use of federal aid to help case management agencies retain staff and address data problems as well as a plan to resolve technological issues with its vendor. Read More
Florida
Florida Senate Passes Bill to Establish Rural Emergency Hospitals. Health News Florida reported on February 29, 2024, that the Florida Senate passed a bill, sponsored by Senator Corey Simon (R-Tallahassee), that would establish a category of rural emergency hospitals in the state that could receive Medicare payments to provide emergency services, observation care, and outpatient services. The bill, intended to increase health access in rural areas, awaits House review. Read More
Idaho
Idaho House Committee Advances Bill to Expand Postpartum Medicaid Coverage to 12 Months. The Idaho Capital Sun reported on March 4, 2024, that the Idaho House Health and Welfare Committee has advanced a bill, sponsored by Representative Megan Blanksma (R-Hammett), that would expand postpartum Medicaid coverage from 60 days to 12 months, effective July 1. The bill now heads to the House floor and would also require approval from the Senate and the Governor to become law. Read More
Illinois
Illinois Democrats Call on CMS to Approve Section 1115 Demonstration Waiver. Vermilion County First reported on March 5, 2024, that United States Representative Robin Kelly (D-IL) issued a letter to the Centers for Medicare & Medicaid Services (CMS) to urge the approval of Illinois’s application for a Section 1115 demonstration waiver. Under the waiver, the state’s Medicaid program would be able to expand access to food is medicine interventions, such as medically tailored meals, produce prescriptions, and assistance accessing healthy food options for populations at risk for diet-related diseases. The waiver would also provide resources to address homelessness, opioid addiction, maternal mortality, violence prevention, and mental health. Read More
Indiana
Indiana Legislator Proposes Budget Amendment to Increase Medicaid Transparency. The Indiana Capital Chronicle reported on February 28, 2024, that Indiana House Ways and Means Committee Chair Jeffrey Thompson (R-Lizton) proposed an amendment to the budget bill requiring additional reporting requirements on the Family and Social Services Administration (FSSA), the state’s Medicaid agency. FSSA would need to submit two annual reports to the State Budget Committee, present a plan for monitoring expenses, and analyze the feasibility of a Medicaid dashboard with monthly expenditure and enrollment reports. Legislators did not pass an amendment, proposed by Representative Greg Porter (D-Indianapolis), that would pause the transition of the 1,622 beneficiaries from the attendant care program to Structured Family Caregiving. The bill will next be reviewed by the House floor and will require senatorial approval of proposed changes before it can be signed into law. Read More
Iowa
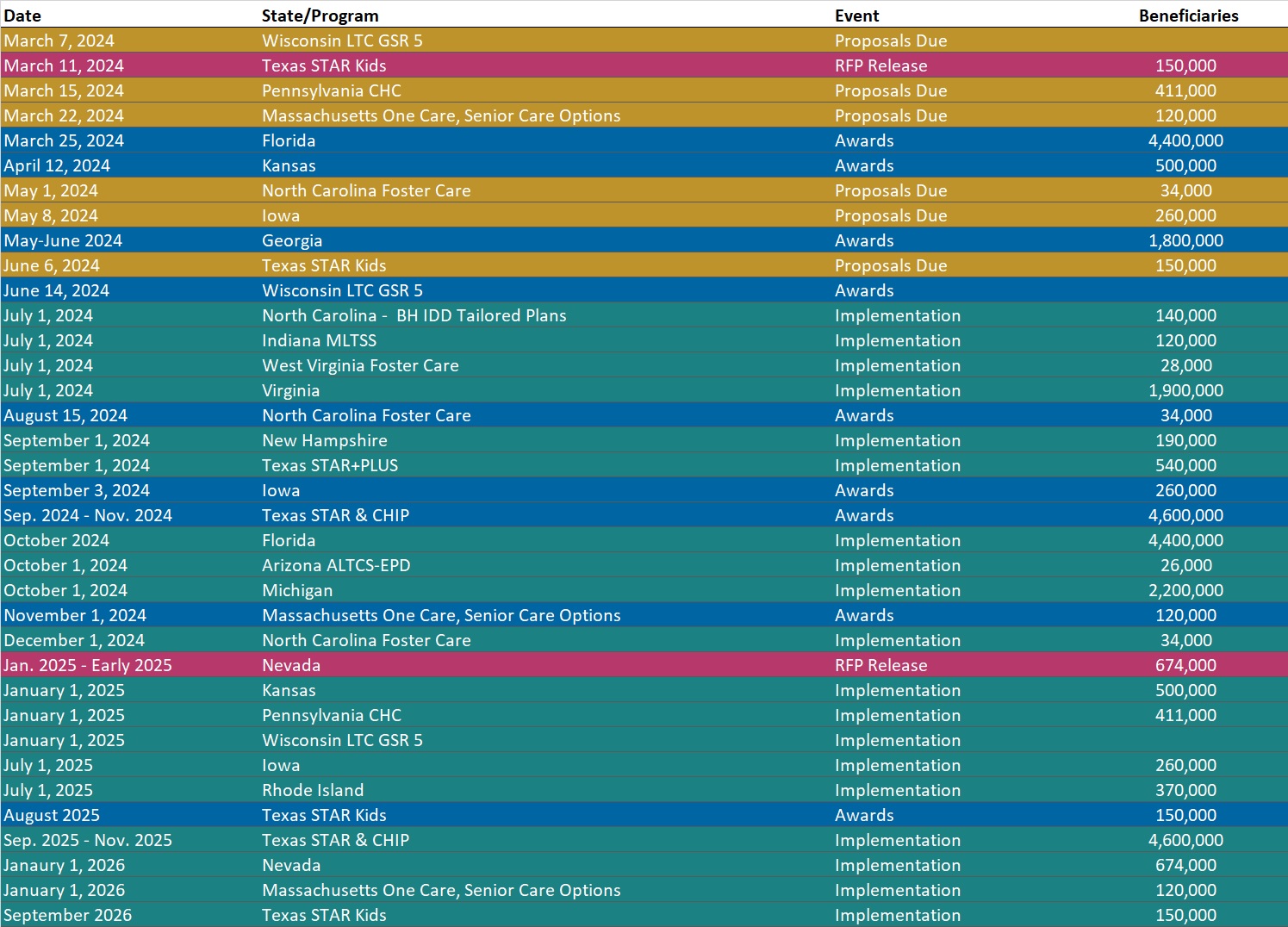
Iowa Releases Health Link Medicaid Managed Care RFP to Reprocure One Contract. The Iowa Department of Human Services (DHS) released on March 1, 2024, a request for proposals (RFP) to provide physical health, behavioral health, pharmacy services, and long-term services and supports (LTSS) for the state’s traditional Medicaid program, the Children’s Health Insurance Program (CHIP) known as Healthy and Well Kids in Iowa (Hawki), and the Iowa Health and Wellness Plan (IHAWP). The state plans to contract with at least one vendor on the new contract. Centene/Iowa Total Care is the incumbent on the current contract which is set to expire on June 30, 2025. Other incumbents are Anthem/Amerigroup and Molina Healthcare, with separate contracts that have options through 2028. The contract term will run for four years, beginning July 1, 2025, with one two-year renewal option. Letters of intent are due March 20, proposals are due May 8, and awards are expected September 3.
The plan will need to have at least 40 percent of the population in a value-based purchasing (VBP) arrangement with the healthcare delivery system by the end of the first year of the managed care contract. This increases to 50 percent VBP enrollment in the second year, and a plan must maintain or exceed 50 percent through the end of the contract period. The VBP arrangement shall recognize population health outcome improvement as measured through state-approved metrics combined with a total cost of care measure for the population in the VBP arrangement. The plan will also be required to support Iowa’s “Quadruple Aim strategy”, including a strategy to advance the amount of payments tied to quality based on the Health Care Payment Learning & Action Network (HCP-LAN) Alternative Payment Model (APM) framework. DHS also plans to implement a withhold arrangement to reward the plan’s efforts to improve quality and outcomes. The pay for performance measures are new to the Iowa Health Link program and focus on operational and process metrics, such as measures related to timeliness and data accuracy, to ensure a successful implementation. Read More
Maryland
Maryland Faces $236 Million Medicaid Budget Shortfall. The Daily Record reported on February 27, 2024, Maryland is facing a $236 million Medicaid budget shortfall due to technical errors and inaccurate projections, according to Budget Secretary Helene Grady’s testimony before state senators. The state will need to account for $115 million for the current fiscal year and $150 million for fiscal 2025, although that value may be lower due to $29 million in budget savings. The shortfall may require the state to draw from its rainy day fund or propose a supplemental budget that could result in cuts to other programs. Read More
Maryland Disenrolls 31,674 Medicaid Beneficiaries During January Redeterminations. The Maryland Department of Health announced that it has disenrolled 31,674 Medicaid beneficiaries, including 28,336 due to procedural reasons and 3,338 due to ineligibility, during January redeterminations. Maryland Matters reported on March 6, 2024, that disenrollments have resulted in an increase in the purchase of individual private health plans on the Exchange. Read More
Michigan
Michigan Disenrolls 12,484 Medicaid Beneficiaries During January Redeterminations. The Michigan Department of Health and Human Services announced on February 5, 2024, that it has disenrolled 12,484 Medicaid beneficiaries during January redeterminations, including 1,698 due to procedural reasons and 10,786 due to ineligibility. Read More
Minnesota
Minnesota Requests Additional Five-year Extension of Substance Use Disorder Reform Demonstration. The Centers for Medicare & Medicaid Services (CMS) announced on February 29, 2024, that Minnesota submitted a request to extend its Section 1115 waiver, titled “Minnesota Substance Use Disorder (SUD) System Reform,” for an additional five years. The demonstration, which expires on June 30, provides Medicaid funding for beneficiaries receiving SUD treatment in an institution for mental disease. The federal public comment period will be open through March 30. Read More
Mississippi
Mississippi Senate Committee Advances Medicaid Expansion Bill with Work Requirement. Mississippi Today announced on March 5, 2024, that the Mississippi Senate Medicaid Committee has advanced the Senate’s Medicaid expansion bill. The Senate bill, like the House plan, would raise the income eligibility for Medicaid coverage to 138 percent of the federal poverty level for working adults, and would likely require Medicaid expansion recipients to pay premiums based on income. Meanwhile, the House Medicaid expansion bill is still awaiting approval in the Senate. Read More
Legislature Passes Bill that Would Grant Early Medicaid Coverage for Pregnant Women. The Associated Press reported on February 29, 2024, that the Mississippi Legislature has passed a bill, sponsored by Representative Missy McGee (R-Hattiesburg) and several co-sponsors, that would allow pregnant women declaring a net income of up to 194 percent of the federal poverty level to receive presumptive Medicaid coverage for 60 days while being considered for Medicaid eligibility. If signed into law, the bill would go into effect July 1. The bill next heads to Governor Tate Reeves for review. Read More
Missouri
Missouri House Approves Bill Blocking Medicaid Payments to Abortion. The Missouri Independent reported on February 28, 2024, that the Missouri House has advanced a bill which would prohibit Medicaid from paying for health care services from any organization that affiliates with abortion providers, or organizations that can help patients go out of state for abortions, including Planned Parenthood. Republican senators have previously vowed to block medical provider taxes unless it is coupled with restrictions on Planned Parenthood funding. The Missouri Supreme Court recently ruled that a similar provision in the 2022 budget bill was unconstitutional. Read More
Nebraska
Nebraska Waiver Expands HCBS to 850 Children on Developmental Disabilities Registry. The Nebraska Department of Health and Human Services announced on March 4, 2024, its Section 1915c home and community-based services (HCBS) Family Support waiver that will provide HCBS to 850 children with intellectual or developmental disabilities. The three-year waiver, effective March 1, aims to provide services to beneficiaries on the Developmental Disabilities Registry and gives each participant an annual budget of $10,000. Read More
Personal Assistance Provider Program Experiences Financial Losses of $1.5 Million Due to Fraudulent Billing, State Audit Finds. KETV ABC 7 reported on February 29, 2024, that Nebraska’s personal assistance provider program was subject to improper billings, resulting in financial losses of up to $1.5 million annually, according to the Nebraska Auditor of Public Accounts. The Nebraska Department of Health and Human Services has agreed to work with the auditor to prevent improper payments and implement improved processes to avoid future cases of fraud. Read More
Nevada
Nevada Holds Workshop on Medicaid Managed Care Procurement Stakeholder Input. The Nevada Department of Health and Human Services held on February 22, 2024, a public workshop regarding the upcoming Medicaid managed care reprocurement slated for January 2025. The state received 30 responses to a request for information that was released in July 2023. During the workshop, the state discussed six key themes from the responses: provider networks, behavioral health, maternal and child health, market and network stability, value-based payment design, social determinants of health and community reinvestments. Stakeholder feedback included ways to improve adequacy in rural areas, such as using telehealth and strengthening telehealth services. The state plans to continue gathering input from rural communities and hospitals and convene workshops. Contract implementation will begin January 1, 2026. Watch Here
New Hampshire
New Hampshire Disenrolls 518 Medicaid Beneficiaries During January Redeterminations. The New Hampshire Department of Health and Human Services reported that it has disenrolled 518 Medicaid beneficiaries during January redeterminations. Of those, 405 were due to procedural reasons. The state renewed coverage for 8,109 Medicaid beneficiaries. The state has 297 pending eligibility cases for individuals whose renewal was due in January.
New York
New York Receives Federal Approval for Section 1332 State Innovation Waiver to Expand Essential Plan Eligibility. New York Governor Kathy Hochul announced on March 4, 2024, that the state has received federal approval for a Section 1332 State Innovation Waiver application which expands the Essential Plan eligibility criteria from its current cutoff of 200 percent of the federal poverty level to up to 250 percent. It is estimated that new eligibility rules will expand Essential Plan coverage to an additional 100,000 New Yorkers. The waiver is approved for five years, starting in April 2024 and continuing through December 2028. Read More
New York Bill to Transition Home Care to FFS Could Save $975 Million in Medicaid Spending, Independent Report Finds. Crain’s New York Business reported on March 5, 2024, that implementation of the Home Care Savings and Reinvestment Act to transition home care from managed care to fee-for-service could save New York $975 million in state and federal Medicaid spending in 2025, according to an independent bipartisan analysis by the Step Two Policy Project. The proposed bill would shift home care management from the state’s 24 managed care plans to Health Homes, which are independent care managers operated by the state. The analysis showed that managed long-term care and personal care spending totaled $8.4 billion during fiscal 2023, accounting for almost a quarter of all Medicaid spending. Read More
Comptroller Finds $50 Million in Improper Medicaid Drug Payments. The Times Union reported on February 27, 2024, that New York’s Medicaid program overpaid $50 million in improper drug claims due to lack of oversight from the state Department of Health, according to an audit between 2017 and 2023 by state Comptroller Thomas P. DiNapoli’s office. The audit recommended that the Health Department attempt to recoup as many of the improper payments as possible, and institute additional protocols to ensure it is only paying managed care organizations for eligible Medicaid-covered drugs. Read More
Oregon
Oregon CCOs to Offer Grant Funding to Support Community Organizations in HRSN Delivery. The Oregon Health Authority announced on February 29, 2024, that coordinated care organizations (CCOs) will administer community capacity building fund grants to allow community organizations to deliver health-related social needs (HRSN) benefits to eligible Medicaid members. These benefits may include climate resources (available in March 2024), housing resources (available in November 2024), and nutrition services (available in January 2025). Applications for grant funding will be open through May 31, and awards will be released in July and September, with funding becoming available between August and October. Read More
Pennsylvania
Pennsylvania Releases Electronic Visit Verification Module RFP. The Pennsylvania Department of Human Services (DHS) released on February 29, 2024, a request for proposals (RFP) seeking a vendor to provide Electronic Visit Verification (EVV) module services to beneficiaries who are authorized to receive personal care and home health care services. Through this procurement, DHS is seeking a vendor to implement an Open Choice Model EVV Module, allowing for submission of information from alternate EVV systems to an aggregator, as a part of its Medicaid Management Information System Modernization Project to replace the current EVV solution. Responses are due April 15. The five-year contract will begin on the effective date and have four one-year renewal options. The current EVV vendor is DXC/Gainwell Technologies, which contracts with Sandata.
Rhode Island
Rhode Island Releases External Quality Review Organization RFP. The Rhode Island Executive Office of Health and Human Services (EOHHS) released on February 29, 2024, a request for proposals (RFP) seeking an External Quality Review Organization (EQRO) to aid EOHHS in improving service delivery and quality of care and implementation of the department’s transition to a full risk-bearing health care delivery system for managed medical services, slated for fiscal 2028. EOHHS is seeking a vendor with expertise relevant to new long-term services and supports, which the state will offer as an in-plan benefit starting July 1, 2025, including for full benefit dually eligible individuals. In addition, the EOHHS expects to work with the EQRO to broaden value-based payment (VBP) models to shift incentives, such as the development of Certified Community Behavioral Health Clinics (CCBHCs), across the delivery system towards maximizing health. Proposals are due March 28. The contracts are anticipated to begin on July 1, 2024, and run for three years with four one-year renewal options. The incumbent is Ipro. Read More
Tennessee
Tennessee to Release Pharmacy Benefits Administrator RFP in Fourth Quarter of 2024. The Tennessee Department of Finance and Administration, Division of TennCare announced that it will release a request for proposals (RFP) for a Pharmacy Benefits Administrator (PBA) to manage prescription drug benefits for the TennCare Pharmacy Programs in the fourth quarter of 2024. These programs consist of the TennCare Pharmacy Medicaid Program and the commercial pharmacy programs CoverRx and CoverKids, which collectively serve approximately 1.5 million beneficiaries. The selected PBA will provide services such as claim adjudications, customer service call centers, prior authorizations, drug utilization reviews, rebate administration, and mail-order pharmacy. The incumbent is OptumRx. Read More
Texas
Texas Extends Postpartum Medicaid Coverage to 12 Months. Texas Governor Greg Abbott announced on February 29, 2024, that Texas is extending postpartum Medicaid coverage from 60 days to 12 months, effective March 1, 2024. The state received approval from the Centers for Medicare & Medicaid Services in January and projects that approximately 137,000 beneficiaries will be served by the extension in fiscal 2025. Read More
Vermont
Vermont Releases Medicaid Permanent Supportive Housing Assistance RFI. The Vermont Agency of Human Services released on February 29, 2024, a request for information (RFI) to inform the design and implementation of a Medicaid Permanent Supportive Housing Assistance Benefit, which aims to reduce homelessness and healthcare costs for adult Medicaid enrollees. The RFI specifically seeks information regarding the design and implementation of Conflict-Free Case Management, the development of prioritization and eligibility criteria for recipients, and input on qualifications for providers. Responses are due March 29, 2024. Read More
Virginia
Virginia Announces Awards for Statewide Medicaid Managed Care Procurement. The Virginia Department of Medical Assistance Services (DMAS) announced on February 28, 2024, its intention to award Cardinal Care Medicaid managed care program contracts to five health plans: incumbents CVS/Aetna, Elevance/Anthem, Sentara/Optima Health, and United Healthcare, and non-incumbent Humana. A separate foster care specialty plan contract was awarded to Elevance/Anthem. Molina, a current incumbent, was not one of the awardees. The contract is set to begin on July 1, 2024, and will run for six-years with two two-year renewal options. Read More
National
Biden Administration Takes Steps to Prevent Corporate Overcharging of Consumers, Government Programs. Health Payer Specialist reported on March 6, 2024, that the Biden Administration has taken steps to curtail healthcare entities’ overcharging of consumers, including the establishment of a “Strike Force on Unfair and Illegal Pricing” to prevent faulty business practices, such as junk fees and onerous late payment charges. The White House additionally held a listening session regarding the business practices of pharmacy benefit managers, which have previously been accused of attempting to improperly increase drug prices. Several Democratic senators also sent a letter to the U.S. Department of Health and Human Services and the Centers for Medicare & Medicaid Services to urge the agencies to ensure that Medicare Advantage funding is directed toward patient care. Read More
Federal Regulators Release RFI to Investigate Private Equity Healthcare Deals. Modern Healthcare reported on March 5, 2024, that federal regulators have released a request for information (RFI) to investigate private equity firms healthcare investments, due to concerns that these deals generate profits for corporate investors at the expense of patients’ health and affordable care. Regulators are seeking information on the effects of private equity and other corporate investor-backed healthcare transactions, specifically those that fall under regulators’ threshold for review. The public comment period will be open through May 6. Read More
HHS Urges Medicare Advantage, Medicaid Plans to Relax Prior Authorization Amid Cyber Attacks. The U.S. Department of Health and Human Services (HHS) announced on March 5, 2024, that it is working to address cash flow and operational concerns as claims processing remains disabled for healthcare providers due to the cyber attacks on Change Healthcare. HHS is issuing federal guidance to Medicare Advantage and Medicaid plans requesting that they remove or relax prior authorization requirements and grant advance funding to highly affected providers. The department is also directing Medicare Administrative Contractors to expedite switching data and claims processors for Medicare providers. Read More
U.S. Fifth Circuit Court to Hear Affordable Care Act Preventive Mandate Appeal Case. Health Payer Specialist reported on March 4, 2024, that the U.S. Fifth Circuit Court of Appeals will hear oral arguments regarding a lawsuit, Braidwood v. Becerra, which stipulates that the preventative care mandate of the Affordable Care Act violated the religious beliefs of plaintiff Braidwood Management as well as the Religious Freedom Restoration Act. The lawsuit was initially filed four years ago in a Texas federal court and maintains that the United States Preventive Services Task Force, which implemented the mandate, was unconstitutional because its members were not appointed by the president or confirmed by the Senate. The Fifth Circuit is expected to release a decision within the next few months. Read More
Legislators Consider 1.68 Percent Medicare Pay Increase for Physicians. Stat News reported on March 3, 2024, that Representative Kay Granger (R-Texas) introduced legislation that would partially mitigate the 3.4 percent Medicare cut to physician reimbursement that took effect January 1. The pending measure includes a 1.68 percent increase beginning March 9, and is one of several Medicare payment policies that will run through December, if enacted. The bill is part of a $450 billion bipartisan legislative package that must be passed by March 8 to circumvent a potential partial government shutdown. Read More
United Health Group Provides Temporary Funding, Pharmacy System During Cyber Attacks. Modern Healthcare reported on March 1, 2024, that UnitedHealth Group has established a temporary funding assistance program, through Optum Financial Services, and created a temporary version of its Rx ePrescribing service for providers affected by the ongoing cybersecurity crisis. The financial assistance lending program will allow for immediate access to funds for short-term cash flow needs. The breached Change Healthcare systems will remain disabled until further notice. Read More
CMS Releases CY 2025 Medicare Advantage Value-based Insurance Design Model Application. The Centers for Medicare & Medicaid Services (CMS) announced on February 29, 2024, that it has released the calendar Year (CY) 2025 Medicare Advantage (MA) Value-based Insurance Design (VBID) model application. The VBID model will be extended through 2030 and will include changes that address health-related social needs of patients, advance health equity, and improve care coordination for patients with serious illness. Applications are due April 12, 2024. The VBID model tests new model components to improve health and lower costs for MA enrollees. This includes innovations designed to reduce Medicare expenditures; enhance the quality of care for Medicare beneficiaries, including dual-eligibles; and improve the coordination and efficiency of health care service delivery. Read More
CMS Releases Final Part One Guidance for Medicare Prescription Payment Plan. The Centers for Medicare & Medicaid Services released on February 29, 2024, the final part one guidance for the new Medicare Prescription Payment Plan, which will give Medicare Part D beneficiaries the option of paying out-of-pocket costs in monthly installments over a year, beginning in 2025. The guidance specifically focuses on outlining the necessary operational requirements for Medicare Part D plan sponsors in preparation for the program, such as identification of eligible enrollees, the opt-in process for enrollees, protections, and evaluation of the program. The guidance additionally requires sponsors to notify pharmacies to provide program information to anyone meeting a $600 out-of-pocket threshold on a single prescription and to process election requests within 24 hours during the plan year. An Information Collection Request, which includes communication materials for sponsors, will be open for public comment until April 29 and public comment for the draft part two guidance is open for comment until March 16. Read More
Medicaid, CHIP Enrollment Drops 1.5 Million in November 2023, CMS Reports. The Centers for Medicare & Medicaid Services (CMS) reported on February 29, 2024, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) was approximately 85.8 million in November 2023, a decrease of 1.5 million from October 2023. Medicare enrollment was 66.8 million, up 154,255 from October 2023, including 32.6 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
Congress Reaches Fiscal 2024 Stopgap Funding Deal, Preventing Government Shutdown. Modern Healthcare reported on February 28, 2024, that Congress has agreed on six out of 12 appropriation bills that will fund the government for the remainder of fiscal 2024, seeking to prevent a partial government shutdown. The full-year spending bills have a newly set deadline for March 8, while the remaining six bills have until March 22. The bills include legislation to delay $16 billion in Medicaid disproportionate share hospital payment cuts, partially roll back a Medicare pay cut for physicians, and extend funding for community health centers in the short-term bills. Read More
Large Portion of Health Care Quality Measures Worsened During Pandemic, CMS Finds. Axios reported on February 29, 2024, that a large portion of health care quality measures worsened during 2020 and 2021, the initial years of the COVID-19 pandemic, compared to baseline data from 2016 to 2019, according to a report by the Centers for Medicare & Medicaid Services (CMS). Key priority measures that were worse during the pandemic included wellness and prevention, behavioral health, safety, chronic conditions, and seamless care coordination. In total, 38 percent of measures analyzed in 2020 were worse, and 47 percent were worse in 2021. Read More
MACPAC Meeting Is Scheduled for March 7-8. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on March 1, 2024, that its next meeting will be held on March 7-8. Among the topics for discussion will be Medicaid coverage of health-related social needs, improved transparency of Medicaid financing, and streamlining home and community-based services. Read More
Industry News
The Ensign Group Acquires Skilled Nursing Facilities in Colorado, Kansas. The Ensign Group, a senior living and skilled nursing home operator, announced on March 4, 2024, that it has acquired Oakwood Care and Rehabilitation, a 170-bed skilled nursing facility, and Park Post Acute, a 135-bed skilled nursing facility, in Colorado. Ensign also acquired Atchison Senior Village Rehabilitation and Nursing Center, a 45-bed skilled nursing facility in Kansas. These acquisitions became effective March 1, 2024. Ensign now operates 302 healthcare operations across 14 states. Read More
InnovAge Launches Florida PACE Program. InnovAge announced on March 4, 2024, that it has launched its first Program of All-inclusive Care for the Elderly (PACE) program in Florida. The center will serve approximately 1,300 individuals and provide integrated healthcare and support services at no cost to seniors with Medicare and Medicaid coverage. InnovAge also operates PACE centers in California, Colorado, New Mexico, Pennsylvania, Virginia, and Florida. Read More
The Pennant Group Acquires Two UT Senior Living Communities. The Pennant Group announced on March 1, 2024, that it has acquired two Utah-based senior living facilities, Capitol Hill Senior Living and Southgate Senior Living, effective March 1. Both facilities offer assisted living and memory care and have 113 and 75 units, respectively. Subsidiaries of the Pennant Group operate 104 home health and hospice agencies and 53 senior living communities nationwide. Read More
WindRose Health Investors Completes Acquisition of CardioOne. New York-based Private equity firm WindRose Health Investors announced on March 4, 2024, that it has acquired CardioOne, a delivery enablement company that serves independent cardiologists. WindRose will provide up to $100 million in additional capital to support the company’s ongoing growth. Read More
Geisinger Health Names Terry Gilliland as President, CEO. Modern Healthcare reported on March 4, 2024, that Terry Gilliland has been named the president and chief executive of Geisinger Health. Gilliland will assume his role once the current president and chief executive, Jaewon Ryu, begins leading Risant Health. Kaiser Permanente is set to acquire Geisinger Health, which would be rolled into a new, not-for-profit entity called Risant Health. Read More
Northwell Health to Acquire Nuvance Health. Modern Healthcare reported on February 28, 2024, that Northwell Health plans to acquire Nuvance Health in a no-cash deal that would create a combined system with 28 hospitals, approximately 100,000 employees, and more than 1,000 care sites throughout New York and Connecticut. The transaction is intended to increase Nuvance’s ambulatory footprint, increase access to technology, and permit additional risk-bearing arrangements with payers. While an exact sum was not released, the transaction is expected to close by the end of the year, pending regulatory approval. Read More
RFP Calendar
Company Announcements
MCG Press Release:
MCG Experts to Speak at HIMSS 2024 on Prior Auth Automation and CMS Final Rule Compliance. MCG Health, part of the Hearst Health network and an industry leader in technology-enabled evidence-based guidance, will host two presentations at the HIMSS Global Health Conference & Exhibition (March 11-15, 2024) in Orlando, Florida. These sessions will focus on MCG’s successful efforts in implementing the nation’s first, scalable prior authorization automation workflow between health plans and hospitals. MCG experts will also discuss how this new technology can support compliance efforts with the Interoperability and Prior Authorization Final Rule (CMS-0057-F) which was announced by the Centers for Medicare & Medicaid Services (CMS) on January 17, 2024. Read More
HMA News & Events
HMA Webinars:
Substance Use Disorder (SUD) Ecosystem of Care: Pivoting to Save Lives Part 1–Overview, and The Role of Health Promotion and Harm Reduction Strategies. Thursday, March 14, 2024, 12 PM ET. Join us for part 1 of our 4-part webinar series, ‘Substance Use Disorder Ecosystem of Care: Pivoting to Save Lives”. In this session we will provide an overview of the series and take a look at the services and support that comprise a system of care for people who are not yet in treatment. Register Here
The New Technology Add-on Payment (NTAP) Program: What Life Sciences Companies Should Know About Medicare’s Time-Limited Program in 2024. Wednesday, March 6, 2024, 12:30 PM. For biopharmaceutical, medical device, and diagnostic manufacturers, navigating market access and reimbursement in the inpatient hospital setting is a challenge in the Medicare program, where most technologies are bundled into an existing payment rate. This bundled payment methodology means that providers often lack incentives to adopt new medical technologies not already reflected in their costs. Since 2001, the Centers for Medicare & Medicaid Services have offered manufacturers of new, groundbreaking technologies the ability to apply for a New Technology Add-on Payment (NTAP) designation for their drug, device, or diagnostic that will provide hospitals with extra payments when they use the product for the 2-3 year period after market entry of product. These add-on payments are often critical in a hospital’s decision to adopt new technologies. Join Foley Hoag and The Moran Company, an HMA Company, on March 6 for a webinar dissecting the upcoming NTAP application process in 2024 and the frequently asked questions surrounding this time-limited program. Register Here
