HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- Indiana Releases MLTSS RFP

- California Legislature Considers Bill Allowing Medi-Cal Reimbursement for Eyeglasses from Retail Labs

- Delaware Awards Medicaid Managed Care Contracts to 3 Plans

- Florida Governor Issues Order Increasing Audits of PBMs, Preventing Clawbacks in Future Contracts

- Maine Expands Medicaid, CHIP Coverage to Individuals Under 21, Pregnant Women Regardless of Immigration Status

- Massachusetts Selects 25 Community Behavioral Health Centers to Expand Treatment for Mental Health Conditions

- Minnesota Releases RFP for Medicaid, MinnesotaCare Accountable Care Model

- Montana Receives Approval for 1115 HEART Demonstration

- Nebraska Receives Five Bids for Medicaid Managed Care Contracts

- New Hampshire Releases Adult Medicaid Dental Benefit RFI

- Oklahoma Proposes 25 Percent Rate Increase for Medically Fragile Medicaid Services

- Pennsylvania Governor Approves Nursing Home Medicaid Reimbursement Rate Increase

- South Dakota Medicaid Expansion Ballot Campaigns to Join Forces

- Texas Health Plan Awards $2.1 Million in Grants to Address Social Determinants of Health

- Insurers Propose Exchange Plan Premium Rate Hike of 10 Percent in 2023, Says ACASignups.net

- Molina to Acquire My Choice Wisconsin

- Ensign Group Acquires Skilled Nursing Facilities in Texas, Nevada, California

In Focus
Indiana Releases MLTSS RFP
This week, our In Focus section reviews the Indiana Medicaid managed long-term services and supports (MLTSS) request for proposals, released by the Indiana Department of Administration on behalf of the Family and Social Services Administration on June 30, 2022. Indiana is seeking three managed care organizations (MCOs) that will serve an estimated 106,000 enrollees, beginning January 1, 2024, for a period of four years, with two one-year renewal options.
MLTSS Program
Indiana began forming a plan to reform the state’s Medicaid LTSS services in 2019 by holding stakeholder meetings. The state estimated that from 2010 to 2030 the proportion of Hoosiers over age 65 will grow from 13 percent to 20 percent, and that the state’s system would need to be reformed to meet the growing demand. The state set an objective to shift the LTSS program to a managed care model and to move a higher percentage of new LTSS members into home and community-based settings.
The new statewide, risk-based MLTSS program will serve Medicaid beneficiaries who are aged 60 years and older and are classified as aged, blind, or disabled. These beneficiaries will include individuals who are dually eligible for Medicare and Medicaid, those in a nursing facility, and those who are receiving LTSS in a home or community-based setting.
Beneficiaries in this program will receive all traditional Medicaid services, delivered through a capitated managed care arrangement. Those who meet a specified level of care will be eligible to receive home and community-based services (HCBS) waiver services. The Medicaid Rehabilitation Option (MRO), Adult Mental Health Habilitation Services Program (AMHH), and Behavioral and Primary Care Coordination (BPHC) will be carved out of the capitated arrangement. For dually eligible beneficiaries, Medicare will be the first payer for all Medicare covered services, including services that are covered by both Medicare and Medicaid.
Indiana seeks to contract with MCOs that can address complex and chronic health conditions of the program population and integrate care along the continuum and settings of LTSS in the state. Program goals include simplifying access to HCBS and expanding the HCBS provider network, especially in rural areas; using a person-centered approach; improving quality outcomes and consistency of care across the delivery system; promoting caregiver support and skill development; in addition to others.
Timeline
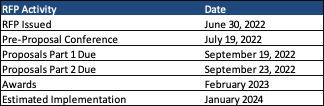
The first part of the proposals is due September 19, with the second part due September 23. Awards are expected in February 2023.
Evaluation
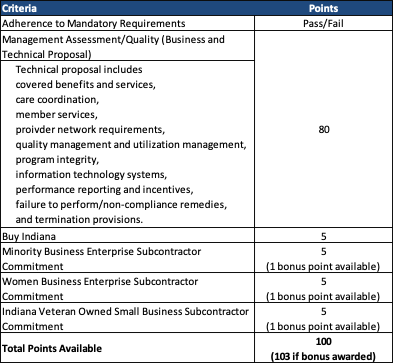
After ensuring proposals meet the mandatory requirement, proposals will be scored out of a total possible 103 points, as shown in the table below.
Preliminary Capitation Rate Summary
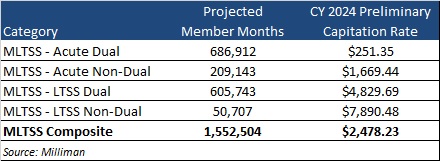
Based on the preliminary calendar year 2024 capitation rate development, contracts are estimated to be worth $3.8 billion annually.
HMA Roundup
California
Legislature Considers Bill Allowing Medi-Cal Reimbursement for Eyeglasses from Retail Labs. Kaiser Health News reported on July 11, 2022, that the California legislature is considering a bill (SB 1089) that would allow clinics to order eyeglasses for Medi-Cal beneficiaries from retail labs in addition to from the California Prison Industry Authority (CALPIA). For more than 30 years, CALPIA has been the sole manufacturer of eyeglasses for Medi-Cal beneficiaries; however, long wait times have lawmakers considering a change. Costs for a pair of glasses from a retail lab would be 141 percent higher than from CALPIA, according to the California Department of Health Care Services. Clinics ordered 880,400 glasses for Medi-Cal beneficiaries in 2021. Read More
California Health System’s Social Determinants of Health Program Savings Cover Less Than a Quarter of Cost, Study Finds. Fierce Healthcare reported on July 6, 2022, that California-based Contra Costa Health Services’ case management program generated $3.4 million in savings from hospitalizations and emergency department visits in one year, according to a study in Annals of Internal Medicine. The savings represent only 17 percent of the $22 million per year costs of the program, which addresses social needs of high-risk patients. Read More
Delaware
Delaware Awards Medicaid Managed Care Contracts to 3 Plans. The Delaware Department of Health and Social Services announced on July 12, 2022, its intent to award contracts to incumbents AmeriHealth Caritas and Highmark Health Options Blue Cross Blue Shield, in addition to new entrant Centene/Delaware First Health, for the state’s Medicaid managed care program, which includes Diamond State Health Plan and Diamond State Health Plan Plus. The plans will provide integrated coverage of physical health, behavioral health, and long-term services and supports. Contracts are anticipated to begin on January 1, 2023, and will run for five years with three optional one-year extensions. Read More
Florida
Governor Issues Order Increasing Audits of PBMs, Preventing Clawbacks in Future Contracts. The News Service of Florida reported on July 8, 2022, that Florida Governor Ron DeSantis issued an executive order requiring audits of Medicaid managed care pharmacy benefit managers (PBMs) and requiring future contracts with PBMs to prevent clawbacks of overpayments to pharmacies. DeSantis also signed legislation to increase oversight of PBMs. Read More
Hawaii
Hawaii Extends Postpartum Medicaid Coverage from 60 Days to 12 Months. Hawaii News Now reported on July 11, 2022, that Hawaii lawmakers passed a funding initiative that extends postpartum Medicaid coverage from 60 days to 12 months. Medicaid covers one in three births in Hawaii. Lawmakers passed another funding initiative this session that restores full Medicaid dental benefits for adults over 21. Read More
Maine
Maine Expands Medicaid, CHIP Coverage to Individuals Under 21, Pregnant Women Regardless of Immigration Status. Beacon reported on July 11, 2022, that Maine extended Medicaid and the Children’s Health Insurance Program (CHIP) to individuals under 21 and pregnant women regardless of immigration status effective July 1. State lawmakers agreed to the coverage extension last year. Read More
Massachusetts
Massachusetts Announces New Recommendations for Reporting, Accountability to Reduce Health Inequities. The Massachusetts Executive Office of Health and Human Services announced on July 6, 2022, health equity data standards and accountability recommendations developed by two health equity technical advisory groups, including standardizing data collection related to social risk factors and introducing health equity accountability in accountable care organization contracts. The public comment period for the recommendations is open until July 15. Read More
Massachusetts Selects 25 Community Behavioral Health Centers to Expand Treatment for Mental Health Conditions. The Massachusetts Executive Office of Health and Human Services announced on July 8, 2022, the selection of 25 Community Behavioral Health Centers (CBHCs) to receive enhanced state funding as part of the state’s “Roadmap for Behavioral Health Reform.” The CBHCs will expand access to behavioral health evaluation and treatment for mental health conditions and substance use disorders, including routine appointments, urgent visits, and crisis intervention. The funding will come through alternative payment models beginning in January 2023. Read More
Minnesota
Minnesota Releases RFP for Medicaid, MinnesotaCare Accountable Care Model. The Minnesota Department of Human Services (DHS) released on July 11, 2022, a request for proposals (RFP) for providers interested in participating in the state’s Integrated Health Partnerships (IHP) Demonstration, an accountable care model that serves Medicaid and MinnesotaCare enrollees under a total cost of care and risk/gain sharing payment arrangement. Letters of intent are due on August 19 and proposals must be submitted by August 26. The contract is anticipated to run from January 1, 2023, to December 31, 2026, with the option to extend up to five years. Minnesota currently has 27 IHPs providing care to over 445,000 Minnesotans. Read More
Montana
Montana Receives Approval for 1115 HEART Demonstration. The Independent Record reported on July 6, 2022, that Montana received approval from the Centers for Medicare & Medicaid Services (CMS) for its Section 1115 Healing and Ending Addiction through Recovery Treatment (HEART) demonstration waiver. The waiver will increase access to treatment by allowing substance use disorder treatment providers with 17 or more beds to bill Medicaid. The state is still negotiating with CMS for approval on some aspects of the waiver, including Medicaid coverage for additional community-based treatment and recovery services, housing supports, and pre-release care management for individuals in the 30 days prior to their release from a correctional setting. The waiver is effective July 1, 2022, through June 30, 2027. Read More
Nebraska
Nebraska Receives Five Bids for Medicaid Managed Care Contracts. The Nebraska Department of Health and Human Services (DHHS) announced on July 8, 2022, the receipt of bids from incumbents Centene/Nebraska Total Care, Anthem/Healthy Blue, and UnitedHealthcare, as well as nonincumbents Medica Community Health Plan and Molina Healthcare of Nebraska to provide Medicaid managed care services through the state’s Heritage Health program. Awards will be announced in late August 2022. Read More
New Hampshire
New Hampshire Releases Adult Medicaid Dental Benefit RFI. The New Hampshire Department of Health and Human Services released on July 11, 2022, a request for information (RFI) on a comprehensive, value-based dental benefit for approximately 88,000 Medicaid adults. The program will be implemented on April 1, 2023. The state is considering options for implementation including carving dental benefits into existing Medicaid managed care contracts, carving out dental benefits to be administered by a separate entity, and other solutions for delivery of value-based dental services. RFI responses, due August 8, 2022, will be utilized to develop a request for proposals. Read More
New Hampshire Methadone Programs Failed to Comply With Medicaid Requirements, Federal Audit Finds. KPVI/The Center Square reported on July 12, 2022, that a federal audit of 100 methadone treatment cases paid for by Medicaid found that more than 90 percent failed to comply with program requirements, including necessary follow-up counseling and long-term recovery plans. The audit, from the Office of the Inspector General, also found that state officials did not provide enough guidance to providers on treatment requirements. The state has agreed to pay back $7.94 million to the federal government to cover the estimated cost of more than 350,000 Medicaid claims from 2016 to 2019.
New York
New York Allocates $71 Million to Establish Crisis Stabilization Centers. Crain’s New York reported on July 13, 2022, that New York has allocated $71 million in COVID relief and American Rescue Plan Act funds to develop crisis stabilization centers for individuals experiencing mental health or substance use crises. The centers will link individuals to services like emergency housing, healthcare, and food. A request for proposals was released on June 30, 2022. Responses are due by October 5, 2022, and contracts will be implemented February 1, 2023. Read More
New York Faces ‘Alarming Lack’ of Mental Health Resources, Testimony Finds. New York Attorney General Letitia James released on July 11, 2022, written testimony concerning the state’s mental health crisis, which reflected an “alarming lack of mental health resources,” including a lack of psychiatric care beds, inadequate Medicaid reimbursement rates, a lack of long-term care options, long wait times, stigmatized perceptions of mental illness, and criminalization of mental health issues. The testimony, submitted to the Office of the Attorney General (OAG), came from government officials, health care providers, community organizations, and New Yorkers affected by the mental health system. Read More
New York Exchange Plan Enrollment Approaches 6.6 Million. The New York State Department of Health reported on July 11, 2022, that Exchange plan enrollment was nearly 6.6 million as of May 2022. The report also found that approximately 140,000 New Yorkers are benefiting from enhanced subsidies through the American Rescue Plan Act. Read More
North Carolina
Lawmakers Pass Fiscal 2023 Budget With Funding for Opioid Use Disorder Treatment. North Carolina Health News reported on July 7, 2022, that North Carolina lawmakers passed a fiscal 2023 budget, including $6 million for state-funded behavioral health management agencies to help expand access to opioid use disorder (OUD) treatment. The budget also includes $1 million for additional housing for a residential recovery program in Durham. The funding comes from a multi-state opioid settlement with drug companies. Read More
Rhode Island
Rhode Island Audit Uncovers Control Deficiencies in State Administration of Medicaid. The Newport Buzz reported on July 12, 2022, that the Rhode Island Medicaid program has internal control deficiencies, according to the state Auditor General. Issues included the need for improved controls over managed care financial activity, Medicaid eligibility for deceased individuals, program integrity safeguards, identifying third-party liability, monitoring of COVID relief funds, and Children’s Health Insurance Program eligibility requirements. Read More
Oklahoma
Oklahoma Proposes 25 Percent Rate Increase for Medically Fragile Medicaid Services. The Oklahoma Health Care Authority announced on July 8, 2022, a proposed 25 percent rate increase for Medically Fragile Waiver services including care management, skilled nursing, hospice, and other services for individuals aged 19 and older with a medically fragile condition. The proposed 1915(c) home and community-based services waiver amendment is open for comment through August 7. Funding for the rate increase was appropriated by the state legislature for year five of the waiver. Read More
Oregon
Oregon Medicaid Mental Health Network Adequacy Falls Short, Study Finds. Healthcare Dive reported on July 6, 2022, that Oregon Medicaid beneficiaries may have limited access to timely mental health care due to inaccurate listings of providers who will take Medicaid coverage, according to a recent Health Affairs study. The study found that 58 percent of network directory listings were providers who did not see Medicaid patients, including 67 percent of mental health prescribers, 59 percent of mental health nonprescribers, and 54 percent of primary care providers. The study used data from administrative claims among members under the age of 64 who were enrolled in Oregon’s Medicaid managed care organizations in 2018. Read More
Pennsylvania
Governor Approves Nursing Home Medicaid Reimbursement Rate Increase. Skilled Nursing News reported on July 11, 2022, that Pennsylvania Governor Tom Wolf approved a 17.5 percent Medicaid reimbursement rate increase for nursing homes, effective January 2023. The rate increase translates to an increase of $35 per resident per day. Read More
South Dakota
South Dakota Medicaid Expansion Ballot Campaigns to Join Forces. The Associated Press reported on July 11, 2022, that the two South Dakota Medicaid expansion ballot campaigns will join forces to back Constitutional Amendment D, which will be voted on in November. Dakotans for Health will join the South Dakotans Decide Healthcare coalition to support the one ballot measure. Read More
Texas
Texas Health Plan Awards $2.1 Million in Grants to Address Social Determinants of Health. Blue Cross Blue Shield of Texas announced on July 7, 2022, $2.1 million in Healthy Kids, Healthy Families grants to 54 community-based organizations statewide to address social determinants of health. The funding also includes $200,000 for economic opportunity. Read More
Virginia
Virginia Increases Medicaid Reimbursements for Primary Care Providers by $82 Million. The Virginia Mercury reported on July 8, 2022, that Virginia primary care providers will receive an $82 million increase to Medicaid reimbursements through the recently signed 2022-24 budget. The increase pushes Medicaid reimbursements from 70 percent of the rate offered under the federal Medicare program for primary care services to 80 percent. Read More
Wisconsin
Wisconsin Medicaid Program to End 2021-23 Biennium with $414.5 Million Surplus. Wisconsin Health News reported on July 12, 2022, that the Wisconsin Medicaid program is expected to have a $414.5 million surplus at the end of the 2021-23 biennium, according to a state Department of Health Services projection. The continuation of enhanced federal Medicaid matching funds because of the public health emergency, partially offset by rising membership, accounted for part of the surplus. Read More
National
Insurers Propose Exchange Plan Premium Rate Hike of 10 Percent in 2023, Says ACASignups.net. CQ reported on July 11, 2022, that insurers have proposed an average Exchange plan premium price increase of 10 percent for 2023, according to Charles Gaba’s ACASignups.net. Insurers in Maine and the District of Columbia proposed increases of 14.7 and 20.7 percent, respectively. The proposed increases, which require state approval, are expected to be finalized by August 17. Read More
10 Percent of Seniors, Disabled Medicaid Enrollees to Lose Coverage After PHE Ends, Study Finds. Kaiser Family Foundation (KFF) reported on July 11, 2022, that 10 percent of Medicaid beneficiaries who are seniors or disabled are expected to lose coverage after the public health emergency ends, based on responses from 14 states in a KFF survey of 50 states and the District of Columbia. States said that staffing shortages and enrollee confusion are the issues most likely to impact enrollment. Read More
Exchange Plans Denied 18 Percent of Claims in 2020, Study Finds. Health Payer Intelligence reported on July 8, 2022, that Exchange plans denied an average of 18 percent of in-network claims in 2020, according to a Kaiser Family Foundation study. Of the denied claims, 72 percent listed “all other reasons” as the explanation for the denial, compared to just two percent for lack of medical necessity. The study, which was based on data from 144 plans, calls for increased transparency of claims denials. Read More
Dental Groups Seek Meeting with CMS to Address Dental Surgery Access Concerns. The American Dental Association announced on July 7, 2022, the submission of a letter to the Centers for Medicare & Medicaid Services (CMS) seeking improved access to dental surgical services for individuals with special needs and disabilities, along with the American Academy of Pediatric Dentistry and American Association of Oral and Maxillofacial Surgeons. The groups noted in the June 30 letter that high-risk Medicaid and commercially insured patients are primarily affected by limited access to dental rehabilitation surgery in hospital outpatient and ambulatory surgical centers. Read More
CMS Proposes Increased Payments for Eligible Medicare ACOs, Decreased Physician Payments in 2023 Fee Schedule. Modern Healthcare reported on July 7, 2022, that the Centers for Medicare & Medicaid Services (CMS) proposed advanced Medicare shared savings payments to low-revenue accountable care organizations (ACOs) that take on increased risk in the draft 2023 Medicare Physician Fee Schedule. Under the proposed changes, eligible ACOs would receive one-time payments of $250,000 and quarterly payments adjusted for enrollee risk factors that would only be clawed back if the ACO begins earning shared savings. The rule also proposes pay decreases for Medicare physicians and fewer supervision requirements for behavioral health practitioners. Read More
U.S. Senators Introduce Medicare Prescription Drug Pricing Reform Legislation. Kaiser Health News reported on July 7, 2022, that U.S. Democratic Senators released Medicare prescription drug pricing reform legislation that would establish a bargaining agreement between the U.S. Department of Health and Human Services and drug manufacturers to reign in prices of up to 20 drugs by 2029. Additionally, the proposed legislation would cap annual out-of-pocket costs at $2,000 for Medicare beneficiaries, ensure free vaccines, and aid low-income seniors in affording prescriptions. Senate Majority Leader Chuck Schumer (D-NY) aims to pass the legislation before August 2022. Read More
Industry News
Molina to Acquire My Choice Wisconsin. Molina Healthcare announced on July 13, 2022, a $150 million agreement to acquire My Choice Wisconsin, a Medicaid managed care organization serving more than 44,000 managed long-term services and supports and other Medicaid members. The acquisition is expected to be finalized in 2022. Read More
West Coast Dental Gets Investment from Court Square Capital Partners. West Coast Dental (WCD) announced on July 11, 2022, an investment from private equity firm Court Square Capital Partners. Payam Sohrab will remain chief executive and president of WCD, which provides dental and orthodontic care in 40 offices in California. Read More
Magellan Health Names Derrick Duke CEO. Modern Healthcare reported on July 8, 2022, that Magellan Health promoted Derrick Duke to chief executive. Duke previously served as chief operating officer and chief financial officer. Duke replaces Ken Fasola, who will lead the healthcare enterprises non-insurance business of Centene, which acquired Magellan in January 2021. Read More
Acute Behavioral Health Acquires Hallmark Youthcare. Acute Behavioral Health announced on July 5, 2022, the acquisition of Hallmark Youthcare, a residential treatment program for youth with behavioral health needs consisting of 82 psychiatric residential treatment facility (PRTF) inpatient beds. Acute Behavioral Health administers inpatient PRTFs and outpatient behavioral health programs to young people. Read More
The Ensign Group Acquires Skilled Nursing Facilities in Texas, Nevada, California; Healthcare Campus in Arizona. The Ensign Group announced on July 6, 2022, the acquisition of Henderson Health and Rehabilitation, a Nevada-based skilled nursing facility (SNF), and Texas SNFs The Eden of Las Colinas; Pleasant Valley Healthcare and Rehabilitation Center; Millbrook Healthcare and Rehabilitation Center; McKinney Healthcare and Rehabilitation Center; and Park Manor Bee Cave. Ensign Group also acquired real estate assets of SNFs Premier Care Center of Palm Springs, Brookside Healthcare Center, and Broadway Villa Post Acute in California. Additionally, the Ensign Group acquired the real estate assets and operations of SNF Villa Maria Post Acute and Rehabilitation, assisted living facility Villa Maria Wellness Living, and behavioral health unit Tucson Recovery at Villa Maria in Arizona. All the acquisitions are effective July 1, 2022. Read More
Evergreen Nephrology Partners With Nephrology Associates of Michigan. Evergreen Nephrology announced on July 5, 2022, a partnership with Nephrology Associates of Michigan, a specialty nephrology practice caring for patients in Southeast Michigan. Evergreen works with nephrologists in local markets to transform kidney care. Read More
ONCAP Invests in Ideal Dental Management Partners. ONCAP announced on July 5, 2022, a significant investment in Ideal Dental Management Partners, in partnership with its affiliated doctors. Ideal Dental provides business and administrative services to specialty dental service providers. The investment was made by ONCAP IV, Onex Corporation’s $1.1 billion private equity fund. The terms of the transaction were not disclosed. Read More
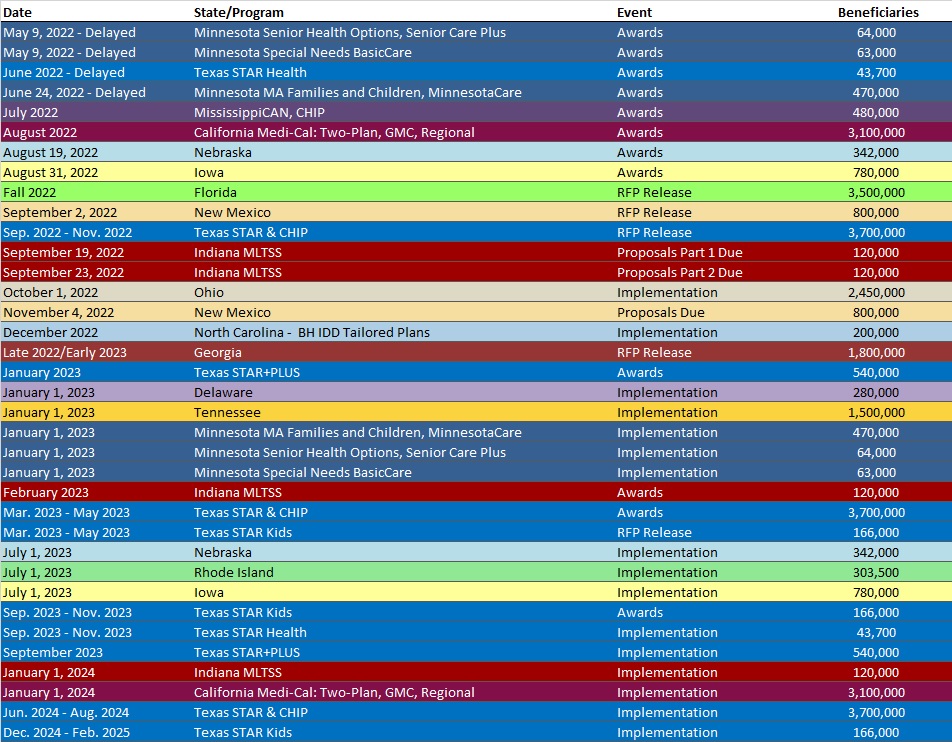
RFP Calendar
HMA News & Events
HMA and the National Council for Mental Wellbeing recently released an issue brief on diversity in the behavioral health workforce. The third issue brief, examines the workforce crisis facing the country’s behavioral health system, highlights the access and service delivery challenges presented and exacerbated by health disparities and inequities. Read more
Join Leavitt Partners tomorrow, July 14 at 11 am ET for the LinkedIn Live “Rural Healthcare Transformation.” Innovative tools, partnerships, and resources are critical for building trust and supporting a rural population. Ada Bair, CEO, Memorial Hospital, Carol Brockmiller, CEO, Quincy Medical Group, and Health Management Associates’ Roxane A. Townsend, MD will join Jennifer Colamonico to discuss their experiences leading health care systems in rural communities and address the importance of collaboration; how transformation in rural health means creatively using and repurposing existing resources; and proven tools providers can use to address community needs.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
- District of Columbia Medicaid Managed Care Enrollment is Up 1.4%, Mar-22 Data
- District of Columbia Medicaid Managed Care Enrollment is Up 1.9%, Apr-22 Data
- Louisiana Medicaid Managed Care Enrollment is Up 2.5%, Apr-22 Data
- New Jersey Medicaid Managed Care Enrollment is Up 1.9%, Apr-22 Data
- Rhode Island Medicaid Managed Care Enrollment is Up 6.9%, 2021 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Delaware Medicaid Managed Care RFP and Awards, 2021-22
- Minnesota Medical Assistance, MinnesotaCare Integrated Health Partnerships RFP, Jul-22
- New Hampshire Medicaid Care Management Dental Benefit RFI, Jul-22
- New Mexico Third Party Assessor/Utilization Review RFP, Jul-22
Medicaid Program Reports, Data and Updates:
- Georgia Department of Community Health Annual Reports, 2014-21
- Pennsylvania Physical HealthChoices Databooks, CY 2018-23
- Rhode Island Medicaid Annual Expenditure Reports, SFY 2013-20
- Wyoming Medicaid Expansion Enrollment and Cost Projections Report, Jan-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
