HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: CMS Releases the Enhancing Oncology Model

- In Focus: CMS Proposes Regulation for Rural Emergency Hospitals

- Delaware Delays Medicaid Managed Care Contract Awards

- Florida Awards Unified Operations Center Contract to Automated Health Systems

- Florida Releases RFI for Children’s Medical Services Managed Care Plan

- Indiana Releases MLTSS RFP

- Maine Extends Dental Coverage to Medicaid Beneficiaries

- Missouri Governor Signs Fiscal 2023 Budget with Funding for Medicaid Expansion

- Nevada Requests 1115 Waiver to Expand Access to Behavioral Health Services

- New Hampshire Governor Signs Legislation to Provide Adult Medicaid Dental Coverage

- North Carolina House Committee Considers Medicaid Managed Care Plan for Foster Children

- Tennessee Advised by CMS to Make Changes to Medicaid Block Grant Program

- Washington State Plan Aimed at Lowering Medicaid Pharmacy Payments Is Rescinded

- HHS Releases Resources to Improve Oversight of Medicaid, CHIP Managed Care Programs

- CMS Releases 2021 Open Payments Data

- Medicaid, CHIP Enrollment Nears 87.9 Million; Medicare Nears 64.4 million

- Francisco Partners Completes Acquisition of IBM Watson Healthcare Data, Analytics Assets

In Focus
CMS Releases the Enhancing Oncology Model
This week, our In Focus section reviews the new Center for Medicare and Medicaid Innovation (CMMI) model named the Enhancing Oncology Model (EOM), released on June 27, 2022, by the Centers for Medicare & Medicaid Services (CMS). This new physician specialty model builds off the previously implemented Oncology Care Model (OCM). The EOM incentivizes the coordination of care and the improvement of care quality for Medicare patients undergoing cancer treatment. The model also seeks to reduce Medicare fee-for-service spending for oncology services, because oncology services are an area of high spending within the Medicare program. As a part of the EOM model participating physician practices will be held accountable for financial and performance targets during six-month episodes of care for systemic chemotherapy administration to patients with common cancer types. The EOM will run for five years beginning on July 1, 2023. Applications to EOM are currently open and will close on September 30, 2022.
CMS indicated that EOM supports President Biden’s Cancer Moonshot initiative to improve the experience of people and their families living with and surviving cancer. EOM aligns with the Cancer Moonshot pillars and priorities of supporting patients, caregivers, and survivors, learning from all patients, targeting the right treatments for the right patients, and addressing inequities.
Consistent with CMS priorities, EOM also has a strong health equity focus and oncology practices who care for underserved beneficiaries are encouraged to apply.
Design of EOM
EOM is built off the foundation of OCM which ran from July 1, 2016, through June 30, 2022. CMS previously solicited feedback from the oncology community and other interested stakeholders on an OCM successor model. Those lessons plus an alignment with CMMI’s strategy refresh priorities of moving to total cost of care accountable models and making cancer care more affordable and accessible created the foundations for the design of the model.
Under EOM, participating Physician Group Practices (PGPs) will take on accountability for their patients’ health care quality and for total Medicare Parts A and B and certain Part D spending during six-month episodes of care. Eligible Medicare patients are those with certain cancers (breast cancer, chronic leukemia, small intestine/colorectal cancer, lung cancer, lymphoma, multiple myeloma, and prostate cancer) receiving chemotherapy treatment.
- Participating practices may bill for a Monthly Enhanced Oncology Services (MEOS) ($70 per month) payment for Enhanced Services provided to eligible beneficiaries. The MEOS payment will be higher ($100 per month) for beneficiaries dually eligible for Medicare and Medicaid.
- Enhanced services are
- Provide EOM beneficiaries 24/7 access to an appropriate clinician who has real-time access to the EOM participant’s medical records.
- Provide patient navigation, as appropriate, to EOM beneficiaries
- Document a care plan for each EOM beneficiary that contains the 13 components in the Institute of Medicine (IOM) Care Management Plan applicable to the EOM beneficiary
- Treat EOM beneficiaries with therapies in a manner consistent with nationally recognized guidelines
- Identify EOM beneficiary social needs using a health-related social needs screening tool
- Gradual implementation of electronic Patient Reported Outcomes (ePROs)
- Participants will be required to take on downside financial risk from the start of the model (with the potential to owe CMS a performance-based recoupment). If participants successfully meet quality and savings targets, they will have the opportunity to earn a retrospective performance-based payment (PBP). These amounts will be based on actual practice performance.
- CMS has not yet specified the quality measures for this model. Instead, the application says the EOM quality strategy will focus on the following domains: patient experience, avoidable acute care utilization, management of symptoms toxicity, management of psychosocial health, and management of end-of-life care. CMS will prioritize measures that; reflect national priorities for quality improvement and patient-centered care, are outcomes-based measures (including those collected from patients), minimize EOM participant burden where possible, and align with CMS and Innovation Center quality strategy.
- Health equity provisions of the EOM include requiring oncology practices to screen for health-related social needs (HRSNs), CMS providing data reports on patient expenditures and utilization for to help health care professionals identify and address health disparities, and CMS increasing reimbursement for the provision of Enhanced Services to patients who are dually eligible for Medicare and Medicaid.
- CMS also will issue payment waivers and benefit enhancements to provide additional flexibility to practices in the way they deliver care to patients. Expected enhancements include telehealth, post-discharge enhancements, and care management home visits.
CMS has designed EOM as a multi-payer model. Medicare Advantage plans, state Medicaid plans and other payers are invited to apply to enter into a Memorandum of Understanding with CMS to align on incentives for oncologists to improve care to their patients and increase participation in value-based care arrangements.
What’s Next
CMS intends to release additional information about EOM payment methodologies later this summer. CMS also will be hosting several upcoming webinars regarding the payment methodology, quality strategy and general application support office hours before the application due date of September 30, 2022. CMS intends to select participants later this year or early next year and will implement the EOM on July 1, 2023.
For more information about this new model and how providers and payers can apply to it, please contact our Medicare team who have knowledge in CMS and its value-based payment programs, Amy Bassano (HMA Managing Director, Medicare) ([email protected]), Julie Faulhaber (HMA Managing Director, Medicare) ( [email protected]) Andrea Maresca (HMA Principal) ([email protected]), or Zach Gaumer (HMA Principal) ([email protected]). To access the EOM application and other model materials, you may visit https://innovation.cms.gov/innovation-models/enhancing-oncology-model.
CMS Proposes Regulation for Rural Emergency Hospitals
On June 30, 2022, the Centers for Medicare & Medicaid Services (CMS) released a proposed regulation establishing the Conditions of Participation (CoPs) for a new hospital provider type, Rural Emergency Hospitals (REHs). The REH concept was first developed by the Medicare Payment Advisory Commission (MedPAC) and subsequently mandated by Congress through the Consolidated Appropriations Act (CAA) of 2021 to address the growing concern over closures of rural hospitals.
REHs provide an opportunity for Critical Access Hospitals (CAHs) and rural hospitals to improve the way care is delivered in their communities, maintain access, and avert potential closure by choosing to focus on the service offerings that are most essential to their communities, such as emergency services, observation care, and additional medical, behavioral, and maternal outpatient services. Importantly, the REH concept enables facilities to maintain a hospital designation absent inpatient capacity thereby ensuring that rural communities retain access to services. This proposed regulation is a significant milestone in CMS’ work to implement the REH designation and their novel payment methodology by their mandated start date of January 1, 2023.
The REH concept is expected to help address the observed health inequities that arise when rural communities lack access to hospitals and other providers. Obtaining an REH designation could be an opportunity for many independent hospitals and delivery systems to strategically reshape themselves in line with their community’s needs while receiving payments from Medicare for doing so.
Within CMS’ proposed regulation, the agency proposes to establish a novel set of REH CoPs which will define the parameters of the REH designation. The REH CoPs closely align with the current CAH CoPs in most cases, while considering the uniqueness of REHs and the statutory requirements. In some instances, the proposed REH policies closely align to the current hospital and ambulatory surgical center standards, such as the polices for outpatient services’ requirements and life safety code, respectively.
As a part of this proposed regulation, CMS seeks input from the rural community on a few key aspects of the REH designation, including:
- The specific proposed REH standards, including the ability of an REH to provide low-risk childbirth-related labor and delivery services and whether the agency should require REHs to provide outpatient surgical services in the event that surgical labor and delivery intervention is necessary.
- Whether it is appropriate for an REH to allow a physician, physician assistant, nurse practitioner, or clinical nurse specialist, with training or experience in emergency medicine, to be on call and immediately available by telephone or radio contact and available on site within specified timeframes.
Updates to CoPs for Critical Access Hospitals
Also within this draft regulation CMS proposes to update the CoPs for CAHs by: (1) adding a definition of primary roads to the location and distance requirements; (2) establishing a patient’s rights CoP; and (3) allowing CAHs that are a part of a larger health system (containing other hospitals and/or CAHs) to unify and integrate their infection control and prevention and antibiotic stewardship programs, medical staff, and quality assessment and performance improvement programs (known as QAPI) to ensure consistent and safe care.
What’s Next
CMS is accepting comments on this rule until August 29, 2022. CMS intends to propose additional policies related to Medicare enrollment, payment, and quality reporting in the upcoming Calendar Year 2023 Outpatient Prospective Payment System/Ambulatory Surgery Center proposed rule. CMS will develop final policies for this program later this year.
For more information about this proposed regulation including how to submit comments and how the REH concept may impact the hospital industry and patients in rural communities please contact our Medicare team who have knowledge in Congressional, MedPAC and CMS policy and operations – Zach Gaumer (HMA Principal) ([email protected]), Amy Bassano (HMA Managing Director, lMedicare) ([email protected]), or Andrea Maresca (HMA Principal) ([email protected]). To access CMS’s proposed Rural Emergency Hospital and Critical Access Hospital Conditions of Participation, visit: https://www.federalregister.gov/public-inspection/current.
HMA Roundup
Arizona
Arizona Requests Federal Funds to Expand Medicaid Housing Supports. Healthcare Innovation reported on June 29, 2022, that Arizona is requesting federal Medicaid funds to expand the state’s housing supports program. The request, which is part of the state’s Section 1115 Medicaid waiver renewal proposal, would include funds to help pay for up to 18 months of transitional housing. Over the past 11 years, Arizona has received about $27 million in state funding annually in rental subsidies for 2,500 Medicaid beneficiaries. Read More
Connecticut
Connecticut Adding Coverage for All Undocumented Residents Would Cost 3 Percent of Medicaid Budget, Study Says. The Connecticut Mirror reported on June 30, 2022, that extending HUSKY health coverage to all undocumented residents in Connecticut would cost the equivalent of three percent of the state’s annual Medicaid budget, according to a study from the RAND Corporation. The coverage would reach an additional 21,000 individuals. The state currently covers children eight years old and younger, regardless of immigration status, and a feasibility study on expanding coverage to all undocumented residents is expected by July 1. Read More
Delaware
Delaware Delays Medicaid Managed Care Contract Awards. Health Payer Specialist reported on July 6, 2022, that Delaware has again delayed awards for its Medicaid managed care procurement. Awards were originally supposed to be announced in May, but they were delayed to June 1 and then to July 1. The state is, “still in negotiations,” according to a Division of Medicaid and Medical Assistance executive, and no new timeline has been announced. Incumbent plans are AmeriHealth Caritas Delaware and Highmark Health Options. Both incumbents submitted proposals, as did Centene and UPMC Health Plan. Read More
Delaware Exchange to Increase With Two More Plans Offering Options. Health Payer Specialist reported on June 29, 2022, that competition on the Delaware health insurance Exchange will increase in 2023, with AmeriHealth Caritas and CVS Health/Aetna planning to offer options. Highmark Blue Cross Blue Shield Delaware is currently the only plan offering options. The state also recently received approval for a reinsurance program. As of 2021, there were 25,320 individuals enrolled in Delaware Exchange plans. Read More
Florida
Florida Awards Unified Operations Center Contract to Automated Health Systems. Florida Politics reported on July 1, 2022, that the Florida Agency for Health Care Administration (AHCA) awarded Automated Health Systems a $140 million contract for Unified Operations Center services. The contract, which will run for seven years with a three-year option to renew, is a part of the state’s modular Medicaid management information systems replacement project. AHCA also announced that the awards for the provider services module contract have been delayed until Fall 2022. Read More
Florida Releases RFI for Children’s Medical Services Managed Care Plan. The Florida Department of Health (DOH) released on June 30, 2022, a request for information (RFI) regarding for the state’s Children’s Medical Services Managed Care Plan, which covers approximately 91,000 children and youth with special health care needs. Centene/Sunshine Health is the current contract holder through January 31, 2024. DOH will begin procuring new contracts in early 2023. Responses are to the RFI due by August 2, 2022.
Illinois
Illinois Has Duty to Ensure Prompt Medicaid Reimbursement by MCOs, Federal Judges Rule. Bloomberg Law reported on July 5, 2022, that Saint Anthony Hospital can sue the Illinois Department of Healthcare and Family Services under the Medicaid Act for allegedly failing to ensure Medicaid managed care organizations (MCOs) promptly reimburse providers for services, according to a federal appeals court. The judges overturned a district court ruling on this matter but affirmed the lower court’s dismissal of the hospital’s claim that the state must also provide financial relief under the Medicaid Act. Read More
Indiana
Indiana Releases MLTSS RFP. The Indiana Department of Administration released on June 30, 2022, a request for proposals (RFP) for managed care plans to serve 106,000 individuals enrolled in the state’s risk-based Medicaid managed long-term services and supports (MLTSS) program. The program will serve Medicaid enrollees aged 60 years and older who are classified as aged, blind, or disabled with limited resources and incomes, including Medicare and Medicaid dual-eligibles, individuals in a nursing facility, and individuals receiving LTSS in a home or community-based setting. The state intends to award contracts to three managed care plans for a period of four years, with two one-year renewal options. The first part of the proposals is due September 19, with the second part due September 23. Awards are expected in February 2023.
Massachusetts
Massachusetts Made DSRIP Payments Before Receiving Approval of ACO Budgets, Audit Finds. The Massachusetts Office of the State Auditor (OSA) released on June 29, 2022, an audit of the MassHealth delivery system reform incentive payment (DSRIP) program, which found that MassHealth made DSRIP program payments to accountable care organizations (ACOs) before receiving approval from the program’s independent assessor for each ACO’s budget. OSA recommends MassHealth establish a monitoring system to ensure that every ACO submits its budget proposal before the beginning of each budget period. The audit examined the time period of January 1, 2018, through December 31, 2020. Read More
Maine
Maine Extends Dental Coverage to Medicaid Beneficiaries. The Associated Press reported on June 29, 2022, that dental coverage will be included in the state’s MaineCare Medicaid program for more than 200,000 beneficiaries, effective July 1. The coverage includes preventative, restorative, and diagnostic care. Read More
Michigan
Michigan Legislature Approves $16.5 Billion in Medicaid Funding for Fiscal 2023. MLive reported on July 1, 2022, that the Michigan legislature approved a fiscal 2023 budget, which includes $16.5 billion in Medicaid funding. The broader state Department of Health and Human Services budget of $33.4 billion also includes $223.1 million to fund a variety of mental health facilities across the state, $34.5 million for behavioral health initiatives, and a $1.7 million general rate increase to direct care workers in private residential facilities. The budget now goes to Governor Gretchen Whitmer for her signature. Read More
Missouri
Missouri Governor Signs Fiscal 2023 Budget with Funding for Medicaid Expansion. The Springfield News-Leader reported on July 1, 2022, that Missouri Governor Mike Parson signed a fiscal 2023 budget, which includes $955 million for the state’s Medicaid MO HealthNet program, including funding for Medicaid expansion. The budget also includes almost $149 million for community health providers to expand services to underserved populations, $2.5 million for the prescription drug monitoring program, and $8.5 million for rural teleheath access. Read More
Nevada
Nevada Requests 1115 Waiver to Expand Access to Behavioral Health Services. The Centers for Medicare & Medicaid Services announced on July 5, 2022, that the Nevada Department of Health and Human Services is requesting a new five-year Section 1115 waiver to expand statewide access to comprehensive behavioral health services for those with opioid use disorders and other substance use disorders. The state is seeking a limited waiver of the federal Medicaid Institutions for Mental Diseases exclusion. The federal public comment period will be open until August 4. Read More
New Hampshire
New Hampshire Governor Signs Legislation to Provide Adult Medicaid Dental Coverage. The New Hampshire Bulletin reported on July 2, 2022, that New Hampshire Governor Chris Sununu signed legislation to provide Medicaid dental coverage to 85,000 adults in the state. Previously, only dental emergencies were covered by Medicaid, not basic oral health care. Funding for the first three years will come from a $21 million settlement the state reached with Centene over Medicaid pharmacy benefit management costs. Read More
North Carolina
North Carolina House Committee Considers Legislation to Create Statewide Medicaid Managed Care Plan for Foster Children. North Carolina Health News reported on June 30, 2022, that the North Carolina House Rules committee is considering legislation (HB 144) to establish a statewide Medicaid managed care plan for children in foster care. Under the bill, which already passed the Senate, the state would release a request for proposals in summer 2022 for a Medicaid managed care plan to cover physical and behavioral health for foster kids. Program implementation would be in December 2023. An earlier, separate initiative to implement a specialty plan for children in foster care in July 2022 was delayed to incorporate stakeholder feedback. Children in foster care in North Carolina currently receive physical health coverage from fee-for-service Medicaid and mental health coverage from local mental health management entities called LME-MCOs. Read More
Oklahoma
Oklahoma Uninsured Rate Falls Below 10 Percent Following Medicaid Expansion, Report Finds. The Tulsa World reported on June 30, 2022, that the uninsured rate in Oklahoma decreased by 4.8 percentage points to 9.6 percent following implementation of Medicaid expansion in July 2021, according to a report from the Oklahoma Policy Institute. Oklahoma has 300,000 Medicaid expansion members. Read More
Tennessee
Tennessee Advised by CMS to Make Changes to Medicaid Block Grant Program. Healthcare Dive reported on July 1, 2022, that the Centers for Medicare & Medicaid Services (CMS) is requesting that Tennessee make changes to its proposed TennCare Section 1115 waiver, which would authorize the state’s Medicaid block grant program, according to a letter sent by CMS following the federal public comment period. The letter advises Tennessee to submit a new budget based on a traditional per member per month cap, adjust the waiver’s pharmacy expenditure authority, and modify its Medicaid terms and conditions to ensure benefits and coverage will not be cut. Read More
Virginia
Virginia Postpartum Medicaid Coverage Extension Will Take Effect July 22. WDBJ reported on July 5, 2022, that Virginia’s Medicaid coverage extension for postpartum women will be effective July 22. The state is extending coverage for people enrolled in FAMIS MOMS and Medicaid for Pregnant Women from 60 days to 12 months of continuous enrollment including breastfeeding support, behavioral health services, and dental. Read More
Washington
Washington State Plan Aimed at Lowering Medicaid Pharmacy Payments Is Rescinded. Health Payer Specialist reported on June 29, 2022, that the Centers for Medicare & Medicaid Services (CMS) rescinded approval of a Washington Medicaid state plan amendment (SPA) aimed at dramatically lowering pharmacy reimbursement rates. The SPA was initially approved in the final days of the Trump administration. Read More
National
HHS Releases New Resources to Improve Oversight of Medicaid, CHIP Managed Care Programs. The U.S. Department of Health and Human Services (HHS) announced on July 6, 2022, new resources to improve the Centers for Medicare & Medicaid Services (CMS) and state oversight of Medicaid and Children’s Health Insurance Program (CHIP) managed care programs. The resources include managed care reporting templates for states to report medical loss ratios and network adequacy and a toolkit to support program monitoring for Medicaid enrollees in Managed Long-Term Services and Supports. HHS also announced updates to a new web-based portal for state reporting on managed care programs to CMS. Read More
U.S. Lawmakers Ask CMS for 3-Year Phase in of 4.6 Percent SNF Cuts. McKnight’s Long-Term Care News reported on July 6, 2022, that a group of U.S. lawmakers, led by Representative Jose Luis Correa (D-CA), requested that the Centers for Medicare & Medicaid Services (CMS) consider a three-year phase-in of the 4.6 percent skilled nursing facility (SNF) prospective payment system parity adjustment, instead of implementing the full 4.6 percent on October 1. The June 29 letter to CMS also expressed concerns about implementing a minimum staffing mandate. A separate group of U.S. Senators also sent a letter to CMS asking not to implement the cuts at this time. Read More
CMS to Monitor Nursing Home Staffing Through Payroll Data. Modern Healthcare reported on July 1, 2022, that the the Centers for Medicare & Medicaid Services (CMS) announced plans to use payroll data to ensure nursing home compliance with staffing requirements, beginning October 24, 2022. The requirements, including having licensed nursing staff 24 hours a day and a registered nurse on site at least eight hours a day, will be monitored through Payroll Based Journal staffing data reported on a daily basis. The regulation comes as CMS prepares to establish minimum staffing requirements this year. Read More
CMS Releases 2021 Open Payments Data. The Centers for Medicare & Medicaid Services (CMS) released on June 30, 2022, open payments data, indicating that applicable manufacturers and group purchasing organizations collectively reported $10.9 billion in publishable payments and ownership and investment interests to covered recipients in 2021. Data comes from 12.1 million records from 533,056 physicians, 233,471 non-physician practitioners, and 1,237 teaching hospitals. The open payments program, which is designed to foster payment transparency, was put into place under the SUPPORT Act of 2018. Read More
Medicaid, CHIP Enrollment Nears 87.9 Million; Medicare Nears 64.4 million. The Centers for Medicare & Medicaid Services announced on June 29, 2022, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) program was nearly 87.9 million in March 2022. Medicare enrollment was nearly 64.4 million, with Medicare Advantage accounting for 29.5 million. More than 1.9 million individuals are Medicare-Medicaid dual eligibles and are included in both totals. Read More
Number of Children Enrolled in Medicaid, CHIP Rises 4.9 Percent from 2019-21, Study Finds. Health Payer Intelligence reported on June 29, 2022, that the number of children enrolled in Medicaid and the Children’s Health Insurance Program (CHIP) rose 4.9 percent between March 2019 and March 2021, according to a report from Urban Institute. The resumption of eligibility verification at the end of the public health emergency could impact the trend, the study said. Read More
Industry News
Francisco Partners Completes Acquisition of IBM Watson Healthcare Data, Analytics Assets. Francisco Partners announced on June 30, 2022, that it completed acquisition of the healthcare data and analytics assets of IBM Watson Health. The new standalone company will be called Merative and will be headquartered in Ann Arbor, MI. Read More
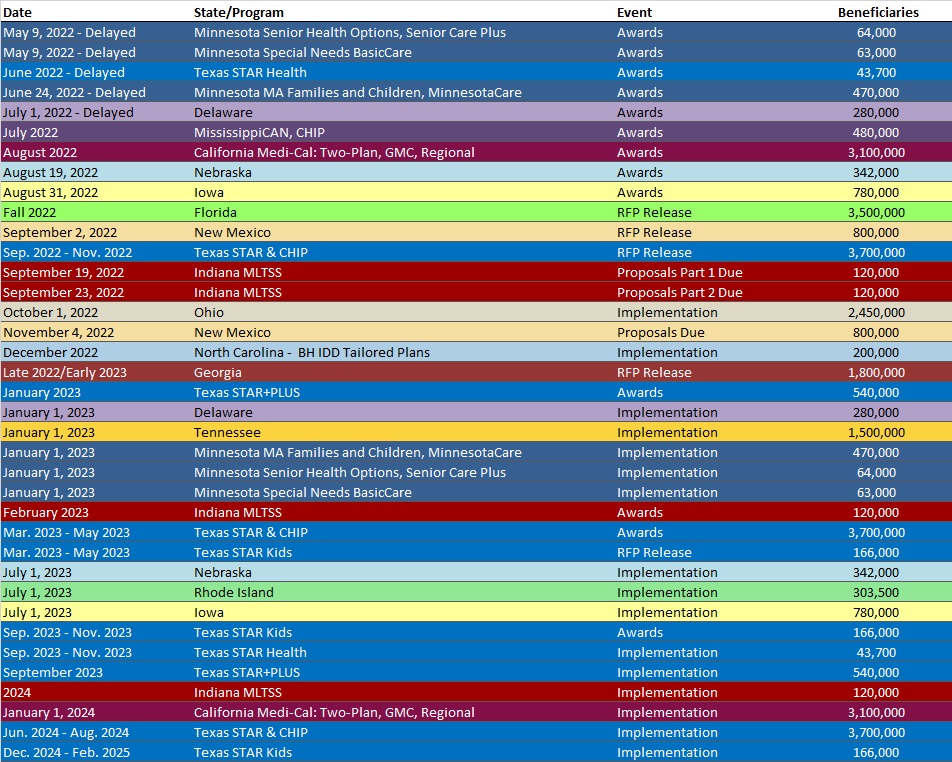
RFP Calendar
HMA News & Events
The Regence Health Policy Center: Moving Cancer Care into the Home with the Huntsman at Home Program – Interview with Dr. Kathi Mooney.
The Regence Health Policy Center: Home-Based Care: What Does the Future Hold?
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
- District of Columbia Medicaid Managed Care Enrollment is Up 0.7%, Feb-22 Data
- New Hampshire Medicaid Managed Care Enrollment is Up 11.3%, 2021 Data
- North Dakota Medicaid Expansion Enrollment is Up 6.7%, Apr-22 Data
- Oklahoma Medicaid Enrollment is Up 3.6%, Mar-22 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 0.8%, Mar-22 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 1.6%, Jun-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Florida Children with Special Health Needs Managed Care RFI, Jun-22
- Indiana Managed Long-Term Services and Supports RFP, Jun-22
- New York IDD Managed Care Assessment RFP, Jun-22
- North Carolina NEMT for New Hanover County RFP, Jun-22
- Ohio Waiver Reimbursement System Modernization RFP, Jun-22
Medicaid Program Reports, Data and Updates:
- Nebraska Medical Care Advisory Committee (MCAC) Meeting Materials, Jun-22
- Pennsylvania MLTSS Subcommittee Meeting Materials, 2021-22
- Texas Behavioral Health Presentations to Legislature, Jun-22
- Texas Long Term Care Presentations to Legislature, Jun-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
