Utilization of value-based payment (VBP) strategies continues to expand, with states and health plans recognizing the benefits of rewarding outcomes over volume. This includes population based VBP initiatives intended to address disparities. Health Management Associates (HMA) is at the center of these initiatives, supporting payers with development and implementation, as well as supporting providers through the transition from a traditional FFS model to maximizing reimbursement through effective care delivery, supported by the necessary administrative infrastructure and resources. As our clients in health care communities move forward with alternative payment models, we have developed tools and strategies to achieve the essential milestones to successful implementation.
Milestone 1: Provider Readiness Assessment
Successful planning for the transition to VBP begins with an understanding of where your organization is starting from, informing the targeted milestones associated with each providers’ unique strengths and challenges.
Understanding that success under VBP models requires adjustment of both clinical and administrative practices, HMA has created an assessment tool that considers the programmatic, financial, and technology resources necessary for VBP implementation. In addition to the ability to leverage these resources, organizations must have the capacity for VBP components such as cost reporting, revenue cycle management, and real time risk monitoring through the collection and analysis of data.

“With VBP on the horizon for our organization, HMA helped us to determine our readiness and to devise a strategy to remediate gaps in operations in order to be successful with the new payment model.”
– Tamara Player, CEO; Polara Health, AZ
Milestone 2: Strategy Development and Change Management
A change in reimbursement methodology requires organizational realignment of administrative and programmatic approaches. Assessing and supporting staff through these changes is a key milestone for success. Activities in which HMA have supported our clients include:
Creating leadership and governance buy-in
Preparing the Board and Staff for VBP
Aligning mission and vision with payment models and accountability metrics
Project Management, including development and monitoring of implementation plans
Cross functional team support
Milestone 3: Data Collection and Reporting Capabilities
The ability to collect and report meaningful outcomes is at the core of successful engagement in VBP. Following an assessment of current capabilities, HMA has supported provider organizations in maximizing electronic health record and other data system capabilities to capture data essential for reimbursement, as well as increasing analytic capabilities that are essential for monitoring outcomes to ensure programs can pivot when data indicates outcome achievement may be at risk. Activities include:
Technology and Data Enterprise configuration to support analytics and reporting
Creating real-time access to data
Benchmarking current outcomes against proposed VBP metrics
Alignment of current framework to payer metrics
Creation of internal clinical leadership infrastructure to support proactive monitoring and action in response to data
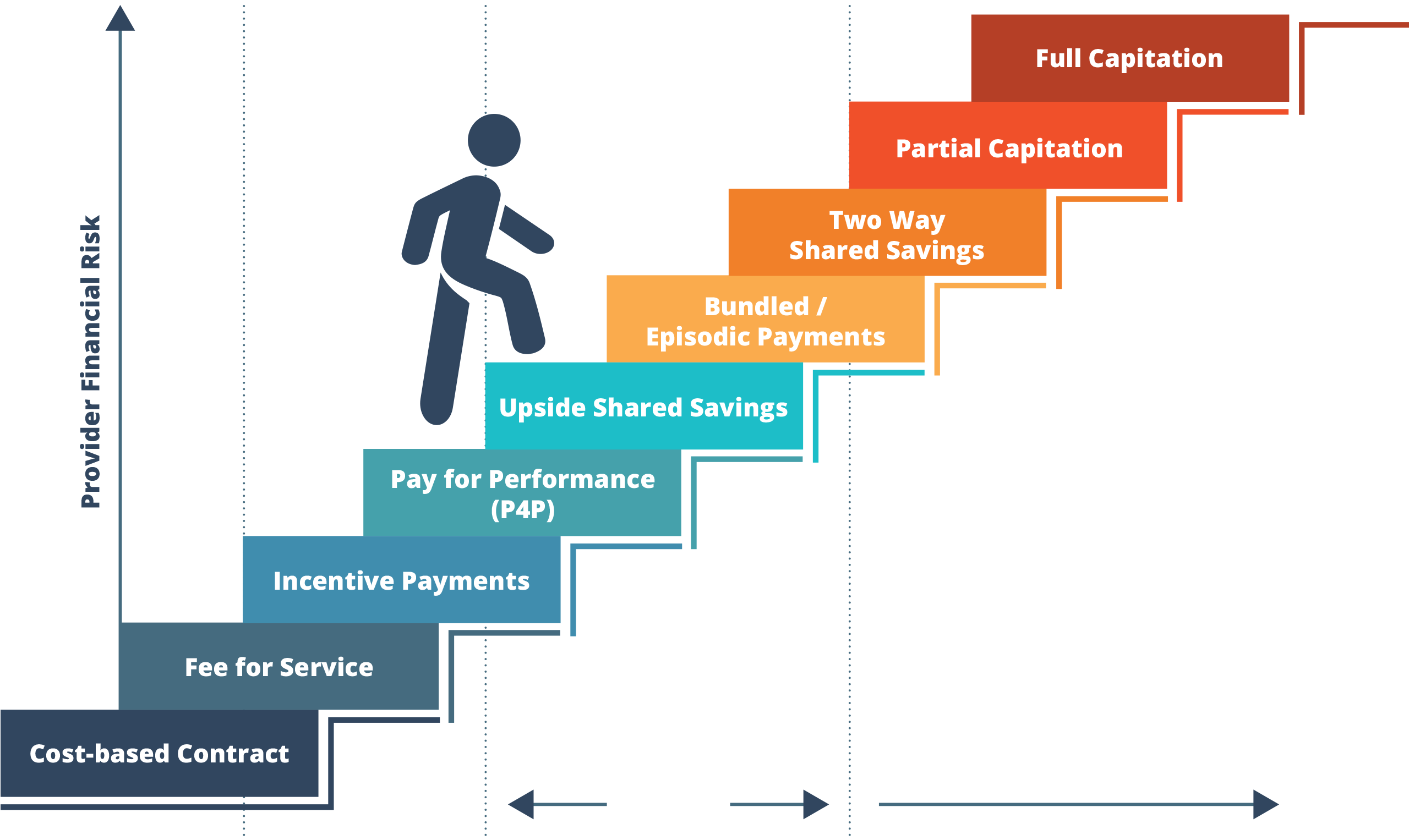
Milestone 4: Business Office and Finance
All aspects of an organization’s financing can be impacted by transitions in payment methodology, including cash flow, impacting cash on hand for capital and other expenses. Anticipating these changes and adjusting accordingly are key to readiness for VBP and importantly, mitigating risk during the transition. HMA can assist with:
Assessing organizational ability to accept risk
Developing a risk corridor based on organizational readiness
Negotiating alternative payment arrangements with payers
Milestone 5: Clinical Programmatic Approaches under VBP
VBP arrangements provide opportunities for organizations to move closer to the goal of achieving outcomes for their clients, rather than productivity targets and units of service. This includes incorporating approaches that could not receive reimbursement under an FFS model. With this flexibility comes the opportunity to review and adapt clinical approaches and programming, including population specific strategies. HMA is ready to support these efforts through:
Workforce analysis
Re/design of clinical workflows
Implementation of measurement-based care
Optimization of clinical templates within the EHR to support data collection and reporting
Understanding the opportunities of value-based payment across the continuum of payment models
While these activities may seem overwhelming, HMA is ready to support your organization to receive reimbursement based on meaningful improvement for your clients through technical assistance and training on each of the core elements outlined above.
Contact our experts:

Rachel Bembas
Principal

Roxanne Kennedy
Principal