This week, our In Focus section reviews Medicaid spending data collected in the annual CMS-64 Medicaid expenditure report. After submitting a Freedom of Information Act request to the Centers for Medicare & Medicaid Services (CMS), we have received a draft version of the CMS-64 report that is based on preliminary estimates of Medicaid spending by state for federal fiscal year (FFY) 2019. We expect the final version of the report will be completed by the end of 2020 and posted to the CMS website at that time. Based on the preliminary estimates, Medicaid expenditures on medical services across all 50 states and six territories in FFY 2019 exceeded $594 billion, with over half of all spending now flowing through Medicaid managed care programs. In addition, total Medicaid spending on administrative services was $29.5 billion, bringing total program expenditures to $623.5 billion.
376 Results found.

HMA experts publish 50-state Medicaid pharmacy study with Kaiser Family Foundation
In conjunction with the Kaiser Family Foundation (KFF), a team of HMA experts have published survey results and analysis examining administration of the Medicaid pharmacy benefit. HMA contributing colleagues were Kathleen Gifford, Anne Winter and Linda Wiant. Rachel Dolan, Marina Tian, and Rachel Garfield from KFF also contributed.
The report, How State Medicaid Programs are Managing Prescription Drug Costs: Results from a State Medicaid Pharmacy Survey for State Fiscal Years 2019 and 2020, summarized the survey conducted in all 50 states and the District of Columbia.
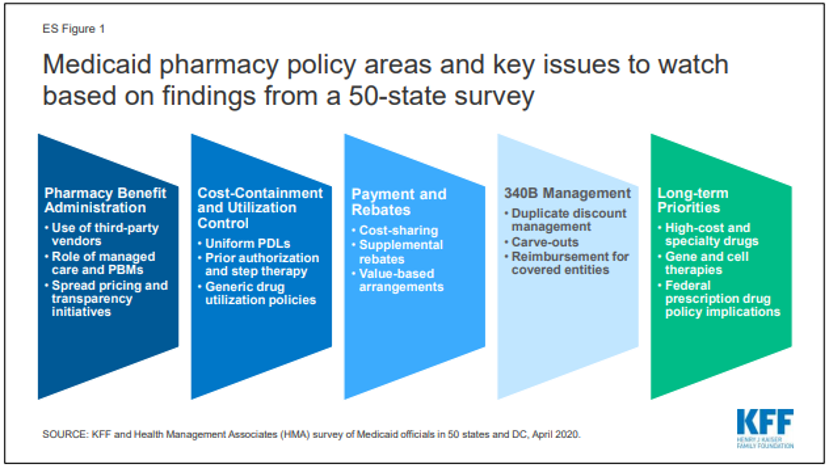
The survey outlines Medicaid pharmacy policy areas and key issues to watch based on feedback from the states in several categories including pharmacy benefit administration, cost-containment and utilization controls, payment and rebates, 340B management and long-term priorities.

50-State Survey of Medicaid Pharmacy Directors
This week, our In Focus section reviews key takeaways from the report, How State Medicaid Programs are Managing Prescription Drug Costs: Results from a State Medicaid Pharmacy Survey for State Fiscal Years 2019 and 2020, prepared by Kaiser Family Foundation (KFF) and Health Management Associates (HMA). The report was written by HMA Managing Principal Anne Winter and Principals Kathleen Gifford and Linda Wiant with Rachel Dolan, Marina Tian, and Rachel Garfield from KFF.

Majority Of Full Benefit Dual Eligibiles Are Not Enrolled In Integrated Program
This week, our In Focus section reviews an issue brief written by HMA consultants examining Medicare-Medicaid integration. In 2019, 7.7 million people in the United States were eligible to receive access to full benefits under Medicare and individual state Medicaid programs. This group of people is known as the Full Benefit Dual Eligible (FBDE) population. While FBDE enrollment in integrated programs nearly quadrupled over the past five years, the number of people enrolled in an integrated program never rose above one in 10 FBDE people.

Examining Key Considerations for Implementing Group Prenatal Care
A team of HMA consultants have authored a peer-reviewed journal article drawing on data from the recently completed five-year evaluation of the Strong Start for Mothers and Newborns II Initiative to discuss key considerations for implementing a group prenatal care model, including barriers to implementation and sustainability as well as strategies for overcoming barriers and sustaining the model.

Dual Eligible Financial Alignment Demonstration Enrollment Update
This week, our In Focus section reviews publicly available data on enrollment in capitated financial and administrative alignment demonstrations (“Duals Demonstrations”) for beneficiaries dually eligible for Medicare and Medicaid (duals) in nine states: California, Illinois, Massachusetts, Michigan, New York, Ohio, Rhode Island, South Carolina, and Texas. Each of these states has begun either voluntary or passive enrollment of duals into fully integrated plans providing both Medicaid and Medicare benefits (“Medicare-Medicaid Plans,” or “MMPs”) under three-way contracts between the state, the Centers for Medicare & Medicaid Services (CMS), and the MMP. As of February 2020, approximately 371, 200 duals were enrolled in an MMP. Enrollment fell 1.2 percent from February of the previous year.

HMA Experts Examine Medicare-Medicaid Integration
In 2019, 7.7 million people in the United States were eligible to receive access to full benefits under Medicare and individual state Medicaid programs. This group of people is known as the Full Benefit Dual Eligible (FBDE) population. While FBDE enrollment in integrated programs nearly quadrupled over the past five years, the number of people enrolled in an integrated program never rose above one in 10 FBDE people.

Medicare-Medicaid integration: integrated model enrollment rates show majority of Medicare-Medicaid dual eligible population not enrolled
Working in conjunction with Arnold Ventures, a team of HMA consultants has written an issue brief, Medicare-Medicaid Integration: Integrated Model Enrollment Rates Show Majority of Medicare-Medicaid Dual Eligible Population Not Enrolled. This brief presents key findings on their examination of the availability of integrated programs in states, the growth in enrollment rates, and differences in enrollment and programs across the country.
The HMA team cited several reasons why Medicare-Medicaid integrated program options are not equally available nationwide and why enrollment is limited in places where programs exist. The result is that millions of people are not enrolled in whole-person, integrated program options – a reality that is inefficient, and worse yet, inequitable.
The HMA team, led by Managing Principal Jon Blum and Principal Sarah Barth, includes Narda Ipakchi, Ellen Breslin, Mindy Cohen, Sharon Silow-Carroll and other HMA subject matter experts.

Medicare and Medicaid Telehealth Coverage in Response to COVID-19
Telehealth service expansions by Medicare and most Medicaid programs aim to rapidly increase access to care and reduce transmission, but also provide a natural experiment for policymakers.
This week, our In Focus section examines the extensive scope of flexibilities Federal and State governments have made to Medicare and Medicaid telehealth coverage in response to the COVID-19 national emergency. In March and April 2020, federal and state policymakers responded to the COVID-19 emergency by temporarily and aggressively expanding the definition of and reimbursement for telehealth services—moves intended to improve access to care and reduce virus transmission. Under the Medicare and Medicaid programs, these temporary expansions have been rapid and historic in scope, and will have substantial implications for patients, providers, payers, and federal/state financing. For policymakers, this temporary expansion may serve as a natural experiment for assessing which forms of telehealth services successfully expand access to care and should become permanent healthcare policy.

HMA Model Provides Forecast of COVID-19 Impact on Medicaid, Marketplace, Uninsured
A model developed by Health Management Associates (HMA) assesses COVID-19’s potential impact on health insurance coverage for each state and forecasts Medicaid enrollment could increase by 11 to 23 million across all states over the next several months.

HMA Review of State Appendix K Waivers in Response to COVID-19
This week, our In Focus section comes from HMA Principals Ellen Breslin (MA) and Sharon Lewis (OR). In direct response to COVID-19, the Centers for Medicare & Medicaid Services (CMS) has encouraged states to maximize Medicaid flexibilities to protect people during the pandemic emergency. This includes state flexibilities for people receiving home and community-based services. States may temporarily amend their Home and Community-Based Services (HCBS) 1915(c) waivers through an expedited process by submitting an Appendix K request. As of March 31, 2020, CMS had approved Appendix K submissions for thirteen states with effective periods ranging from four months to one year.[1] The thirteen states are: Alaska, Connecticut, Colorado, Hawaii, Iowa, Kentucky, Minnesota, New Mexico, Pennsylvania, Rhode Island, Washington, West Virginia and Wyoming.

D-SNP 2021 Hospital and Skilled Nursing Facility Admission Data Sharing Requirements: States and Health Plan Opportunity to Support Care Transitions
This week, our In Focus section provides an overview of new requirements and opportunities for states and Medicare Advantage (MA) Dual Eligible Special Needs Plans (D-SNPs) to increase Medicare and Medicaid coordination in plan year 2021. Specifically, states and health plans will need to partner for compliance with calendar year (CY) 2021 Medicare Advantage Dual Eligible Special Needs Plan (D-SNP) data sharing requirements for D-SNPs that are not designated as a fully integrated D-SNP (FIDE SNP) or a highly integrated D-SNP (HIDE SNP)[1]. CY 2021 State Medicaid Agency Contracts (SMACs) with these D-SNPs must document the notification process for sharing hospital and skilled nursing facility (SNF) admissions for at least one group of high-risk enrollees.[2]