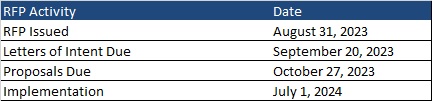
This week, our In Focus section reviews the request for proposals (RFP) for the Virginia Cardinal Care Medicaid managed care program, released by the Department of Medical Assistance Services (DMAS) on August 31, 2023. The RFP includes a new foster care specialty plan. Implementation is scheduled to begin July 1, 2024.
Cardinal Care
Cardinal Care launched in January 2023 as a rebranding of the state’s Medicaid program and Children’s Health Insurance Program—Family Access to Medical Insurance Security Plan (FAMIS). Cardinal Care Managed Care (CCMC) will combine the state’s existing Medallion 4.0 managed care program for traditional Medicaid and the Commonwealth Coordinated Care Plus (CCC Plus) managed long-term services and supports (MLTSS) program to serve 1.9 million Medicaid managed care members.
RFP
The state will award statewide fully capitated, risk-based contracts to a maximum of five health plans. A separate foster care specialty plan contract will also be awarded to one of the winners. If none of the plans win the separate foster care specialty program, all plans awarded a CCMC contract will be required to cover all services.
Selected plans will provide acute care, behavioral health, and MLTSS services to all Virginians who are eligible for Medicaid, including children, adults, and pregnant women in low-income households; children and adults with disabilities; low-income older adults; and individuals receiving LTSS, including dual-eligible populations. The foster care plan will cover children in foster care, individuals younger than 26 years old who were formerly in foster care, and children eligible for adoption assistance.
The RFP contains several targeted focus areas and changes to the managed care program. For example, it emphasizes improvements to the state’s behavioral health care system and improved health outcomes through a focus on health-related social needs such as housing stability and food insecurity for CCMC members.
Contracted plans will be required to operate a dual-eligible special needs plan (DSNP) in Virginia.
Market
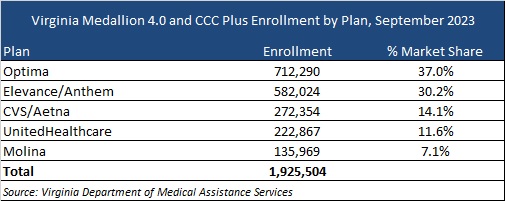
CVS/Aetna, Elevance/Anthem, Sentara/Optima Health, Molina, and UnitedHealthcare are the current incumbents. Effective with the new RFP, DMAS intends to reassign most CCMC members as part of an enrollment process. At present, Optima holds the largest market share of enrollment at 37 percent, followed by Anthem at 30 percent.
Timeline
Letters of intent are due by September 20 and proposals are due on October 27. As previously mentioned, new contracts will begin July 1, 2024. Contracts will have a six-year initial term, with two two-year renewal options. Award dates have not been announced.
Evaluation
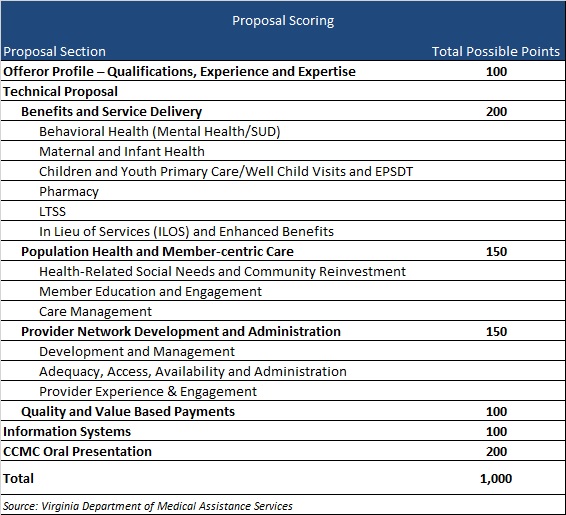
Plans will be awarded up to 1,000 points during the evaluation process based on the categories shown below.