This week, our In Focus section reviews the Pathways HUB model, an approach designed to help coordinate outreach by specialized community health workers who are incentivized to engage high-need populations. An HMA webinar, held May 9, 2019, with Mark Redding, co-developer of the Pathways HUB model, and Heidi Arthur, HMA can be viewed here.
1814 Results found.

HMA Analysis of Modernizing Part D and Medicare Advantage to Lower Drug Prices and Reduce Out-of-Pocket Expenses Final Rule
On May 16, 2019, the Centers for Medicare & Medicaid Services (CMS) issued its final rule, Modernizing Part D and Medicare Advantage to Lower Drug Prices and Reduce Out-of-Pocket Expenses (Final Rule). The proposed rule, which was issued in November 2018, included a number of provisions intended to improve drug price transparency and expand use of utilization management tools to further Medicare Advantage and Part D cost-cutting efforts. However, in response to significant pushback from beneficiary advocates, physician groups, insurers, and pharmaceutical stakeholders, CMS elected not to implement key provisions. These include proposals to allow Part D plans to exclude protected class drugs from formularies as a result of price increases or if the drug is a new formulation of an existing single-source drug as well as proposed reforms to pharmacy price concessions that would require discounts be passed on to beneficiaries at the point of sale. Commenters in opposition to the pharmacy price concession proposal contend that these reforms would result in higher Part D premiums. While CMS has postponed addressing this provision in this Final Rule, the recently issued Department of Health and Human Services (HHS) Office of Inspector General (OIG) proposed rule, if finalized, may include fundamental changes to these pricing arrangements and other federal safe harbors to the anti-kickback statute.

Kentucky Releases Medicaid MCO RFP
This week, our In Focus section reviews the Kentucky Medicaid managed care organizations (MCOs) request for proposals (RFP), issued by the Kentucky Finance and Administration Cabinet on May 16, 2019. The Kentucky Cabinet for Health and Family Services (CHFS), Department for Medicaid Services (DMS) will select up to five Medicaid MCOs to manage health care services for more than 1.2 million people, starting July 2020. Contracts are estimated at more than $7 billion.

Webinar Replay: Creating Effective Health and Law Enforcement Partnerships to Combat the Opioid Epidemic
This webinar was held on June 5, 2019, and was the sixth webinar in a series about addressing the opioid crisis in America.
Multi-sector collaboration is a key strategy for reversing the upward trend in opioid-related deaths, and there are tremendous opportunities to develop solutions through health and law enforcement partnerships. Historically, these sectors held divergent viewpoints and practices to best address opioid use. But today, successful collaborations involving health and public safety leaders are emerging across the country in response to the opioid crisis.
During this webinar, experts from HMA and the New York City Police Department explored key elements in a multi-sector approach to address opioid use, built on a foundation of shared ownership of policies, system response, and programmatic interventions.
Learning Objectives
- Understand the key challenges to partnerships between health systems and law enforcement.
- Learn strategies for strengthening partnerships in which law enforcement, health professionals and community members work together to respond to the opioid crisis.
- Obtain examples of successful collaboration from around the country.
- Uncover current funding opportunities to support your health and law enforcement partnerships.
Speakers
- Laquisha Grant, Senior Consultant, New York City
- Ashley Restaino, Managing Director, Staten Island PPS
- Theresa Tobin, Deputy Chief, New York City Police Department
- John Volpe, Principal, New York City
Who Should Listen
Officials of state and local government, law enforcement, fire departments, emergency response, crisis hotlines and crisis centers; executives of hospitals, health systems, mobile crisis units, and affiliated community providers and payers of crisis services, including Medicaid payers.

Webinar Replay: Advancing and Codifying Health Equity and Wellness for Medicaid Populations
This webinar was held on June 4, 2019.
It’s widely recognized that social determinants of health (SDOH) have a significant impact on mortality and morbidity. Community-Based Organizations (CBOs) play a significant role in addressing SDOH factors that drive health disparities and poor health outcomes. CBOs are directly connected to the populations they serve and commonly address an array of overlapping clinical and social service needs. However, CBOs face many challenges creating meaningful partnerships with health care organizations (HCOs) and health plans. Addressing these challenges is important so CBO contributions can be scaled through a more integrative and inclusive approach within the healthcare system.
During this webinar, experts from the Disability Policy Consortium (DPC) and the Arthur Ashe Institute of Urban Health (AAIUH) joined HMA to discuss the recent issue brief, published by Academy Health, which detailed lessons learned from CBOs in New York and Massachusetts.
Learning Objectives
- How CBOs can advance health equity and wellness goals for the individuals and communities that are the focus of Medicaid payment and care delivery system reform.
- How New York supported CBO engagement in its Delivery System Reform Incentive Payment (DSRIP) plan.
- What the challenges CBOs have experienced in healthcare reform.
- Why we need a National Blueprint for Advancing Health Equity by leveraging the nation’s CBOs to facilitate greater cross-sector collaboration between CBOs and HCOs.
Speakers
Dennis Heaphy, Health Policy Advocate, Disability Policy Consortium, Boston
Humberto Brown, The Arthur Ashe Institute of Urban Health (AAIUH), NYC
Ellen Breslin, HMA, Principal, Boston
Heidi Arthur, HMA, Principal, NYC
Who Should Listen
Executives of Medicaid and Medicaid-Medicare health plans; community, state and federal policy makers and program administrator; CBO and Accountable Care Organization leaders); advocates; and members of the community working to remove barriers to advance health equity and wellness for Medicaid populations.

Medicaid Plan Profit Margin Dips to 0.5 Percent in 2018, Continuing Multi-Year Decline, HMAIS Analysis Shows
This week, our In Focus summarizes the findings of an HMA Information Services analysis of Medicaid managed care plan profitabilty, based on data from annual statutory filings made with the National Association of Insurance Commissioners (NAIC). For information on how to subscribe to HMA Information Resources, contact Carl Mercurio.
Underwriting Margin
An analysis by HMA Information Services, a division of Health Management Associates, shows that Medicaid managed care plans in 34 states and Washington, DC, posted a net underwriting margin of 0.5 percent in 2018, down 10 basis points from 0.6 percent in 2017. For-profit plans posted higher underwriting margins than not-for-profit plans.
Overall, margins have fallen consistently since hitting a four-year high of 2.4 percent in 2015. The data include financial information for about 210 Medicaid managed care plans, with total membership of 37 million in 2018 and revenues of about $188 billion. Net underwriting profit in 2018 was about $911 million, compared to more than $990 million in 2017.
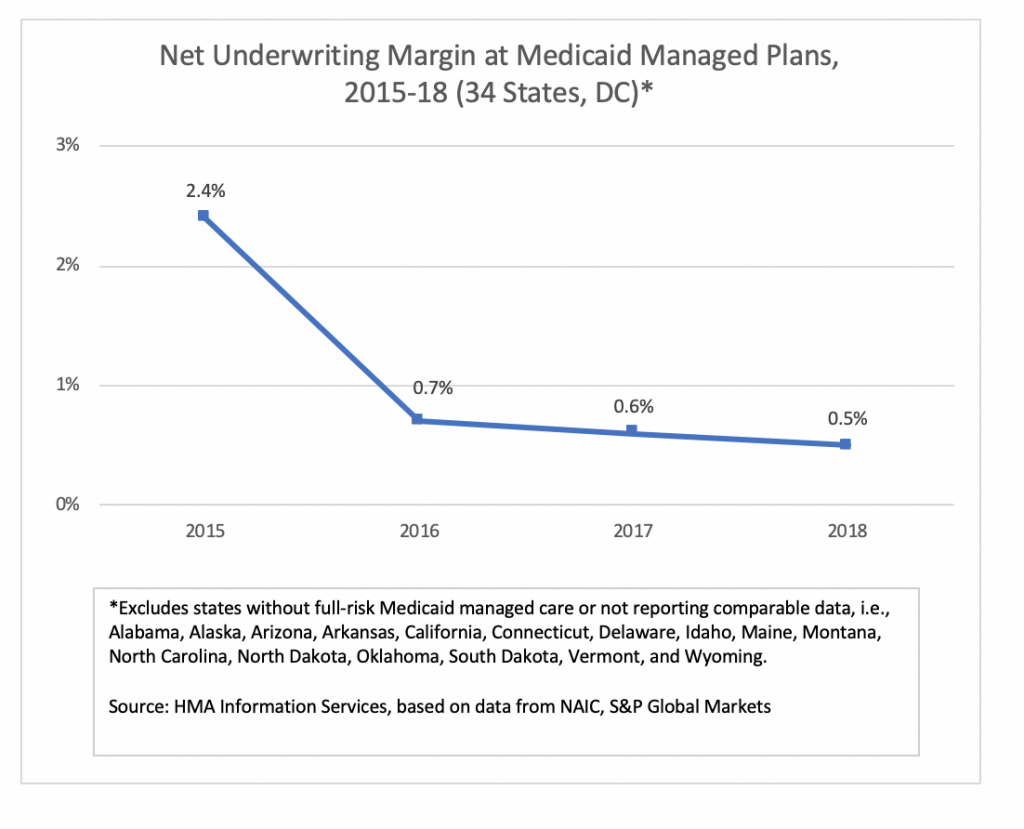
States in which the aggregate Medicaid managed care margin was below the national average in 2018 (based on plans reporting NAIC statutory filings) included Florida, Hawaii, Louisiana, Massachusetts, Mississippi, New Jersey, New Mexico, Rhode Island, Texas, and Virginia.
Not included in the tally are most Medicaid plans in California and Arizona, which don’t report financial information through NAIC. In addition, some of the largest plans in New York don’t report financial information through NAIC.
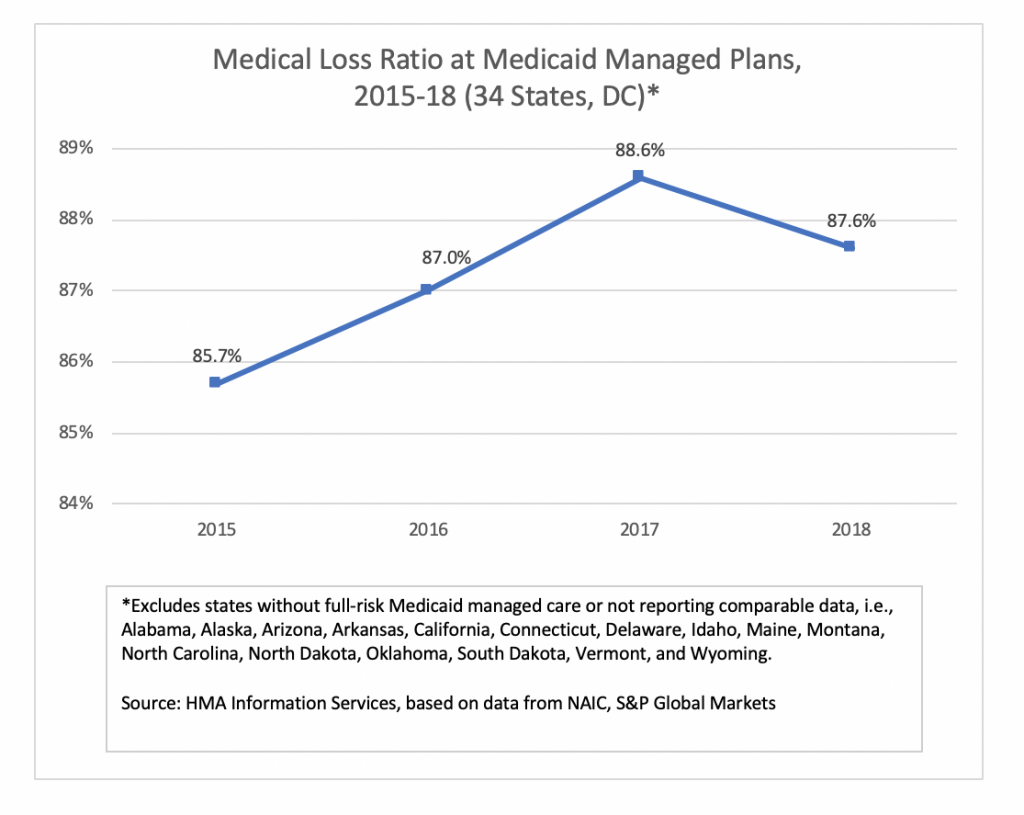
Medical Loss Ratio
Medical loss ratio (MLR) among Medicaid managed care plans in 34 states and Washington, DC, was 87.6 percent in 2018, down about 100 basis points from 2017. The MLRs calculated by HMAIS are blended and may include traditional Medicaid, expansion, and aged, blind and disabled populations, depending on the state. The improvement in average MLR was offset by an increase in administrative costs, resulting in the drop in underwriting margin.

Medicaid and Exchange Enrollment Update – January 2019
This week, our In Focus section reviews updated information issued by the Department of Health & Human Services (HHS) Centers for Medicare & Medicaid Services (CMS) on Medicaid expansion enrollment from the “January 2019 Medicaid and CHIP Applications, Eligibility Determination, and Enrollment Report,” published on April 25, 2019. Additionally, we review 2019 Exchange enrollment data from the “Health Insurance Exchanges 2019 Open Enrollment Period: Final State-Level Public Use File,” published by CMS on March 25, 2019. Combined, these reports present a picture of Medicaid and Exchange enrollment in 2019, representing 72.4 million Medicaid and CHIP enrollees and 11.4 million Exchange enrollees.

HMA MACPAC report, care coordination in integrated care programs serving dually eligible beneficiaries
A team of HMA colleagues including Sarah Barth, Sharon Silow-Carroll, Esther Reagan, Mary Russell and Taylor Simmons completed a study for the Medicaid and Children’s Health Insurance Program (CHIP) Payment and Access Commission (MACPAC) to examine care coordination requirements for several Medicare-Medicaid integrated care models.
The study’s final report, Care Coordination in Integrated Care Programs Serving Dually Eligible Beneficiaries – Health Plan Standards, Challenges and Evolving Approaches, is posted to the MACPAC website.
