This episode of Vital Viewpoints on Healthcare features Dr. Gina Lasky, managing director at Health Management Associates, offering her unique perspective on the persistent challenges surrounding behavioral healthcare. Drawing from her extensive experience and research, Dr. Lasky delves into the complex reasons behind the fragmentation of our behavioral health system and the role incentives play in exacerbating this issue. This episode is for anyone exploring innovative strategies to reform the current reimbursement framework to align incentives for patient-centered outcomes to foster collaboration across disciplines to promote whole-person well-being.
1056 Results found.

Webinar replay: Leavitt Partners – The future of Medicare Advantage supplemental benefits
This webinar was held on April 4, 2024.
This webinar was offered by Leavitt Partners, an HMA company.
More than 30 million Americans are enrolled in MA plans and more than half of Medicare-eligible beneficiaries participate in the program—a number that was less than 30 percent just a decade ago. One reason Medicare beneficiaries opt to participate in MA plans is the ability to offer supplemental benefits, including dental, vision, hearing, transportation services, OTC items, an in-home support services. Initially limited to a core set of offerings, over the years, MA supplemental benefits have undergone significant changes that have led to a broader range of allowable benefits, an expansion of how benefits can be targeted, and, growth in the number of plans offering such benefits.
This webinar covered how to understand MA supplemental benefit growth and the current regulatory environment, including opportunities and threats; discovered the opportunities and challenges MA plans face in offering supplemental benefits; and learned about the issues supplemental benefit providers face in administering supplemental benefits.
Read the Leavitt Partners white paper discussed in the webinar: A Vision for the Future of Medicare Advantage Supplemental Benefits: Advancing Value, But Validating Results
Speakers:
Matt Gallivan, Director, Leavitt Partners, an HMA Company
Andrew Friedell, COO, The Helper Bees
Michael Bagel, Associate Vice President, Public Policy, Alliance of Community Health Plans

Webinar replay: Substance Use Disorder (SUD) Ecosystem of Care-Pivoting to Save Lives Part 2: Empowering Change in the SUD Ecosystem
This webinar was held on April 10, 2024.
As covered in the first webinar of this series, we have an imperative to think and act differently to change the trajectory of not just the long-standing opioid epidemic, but other existing and emerging harmful substance use and addiction. Grounded in equity, empowering change in the SUD ecosystem requires person-centered and community driven approaches to respond to individual wants and needs. We must meet each person where they are as well as consider how the ecosystem of each community can be leveraged to drive change.
In this webinar, we shared examples of best practices that could be improved upon by integrating a person-centered approach; explained how “meeting people where they are” applies to equitable practices, individualized care, and community solutions; and discussed “equity grounded” in the context of the SUD ecosystem including addressing structural barriers, dominant narratives, and incorporating community voices and partnerships.
Below is a report referenced during the webinar:
You may also be interested in the upcoming webinar, “Equity Considerations for Addressing Opioid Use Disorder”. Register now.
Watch previous webinars and register now for upcoming webinars in the series.

HMA 2024 Spring Workshop summary and key takeaways
On March 6, HMA convened a spring workshop of 100 healthcare stakeholders interested in making value-based care delivery and payment work better. This event was designed for those engaging in value-based care and payment transformation, but who are looking to learn from peers to overcome challenges; participants included insurers, health systems, data and tech innovators, service providers, and trade associations.
The event’s name implored people to “Get Real” about the challenges we all face, while reminding ourselves of the imperative of making this transition to ensure the sustainability of our uniquely American healthcare system. In between plenary panels, participants were engaged in cohort discussions exploring the opportunities for progress in areas critical to making value-based care work. While a summary cannot recreate the real-time discussions and simulations from the event, our discussions delivered insights on several critical themes that we believe are important to track.
EMPLOYERS ARE LEANING IN: For all employers pay, they are getting less value over the past decade; the changes made to ERISA that hold the C-suite accountable for paying fair prices for healthcare benefits is a seismic shift in making healthcare purchasing a more strategic priority for employers.
- Elizabeth Mitchell of the Purchaser Business Group on Health illustrated the shift in employers’ awareness – due to data transparency rules – that they aren’t getting the quality they thought they were getting for all that they pay. Transparency, plus a recent change to the Employee Retirement Income Security Act of 1974 (ERISA), is bringing employers back to the table with very specific requests for better outcomes, which they are increasingly pursuing through direct contracting and specific quality frameworks for primary care, maternal care, and behavioral health. Participants continued to reflect on this dynamic in all subsequent discussions, underscoring that this could be a really big deal.
- Cheryl Larson of the Midwestern Business Group on Health talked about the cost pressure on her members leading them to partner in new and different ways, expressing optimism about all payer solutions and other innovative approaches to leverage the cost data that are now available. In her closing plenary session, she said “this issue of accountability on employers…I am excited and optimistic that there are things we can do to get there faster now.”
Data & Technology HAVE TO IMPACT DECISION MAKING: Patients are using the system the way it is designed today, so we can’t just blame them for poor outcomes…we have to actually stop doing things that don’t work and start measuring things the right way.
- Dr. Katie Kaney opened with a dinner keynote discussing her efforts to create metrics that give purchasers a better measurement of whole person care, including clinical, genetic, behavioral, and social factors. Audience members remarked that this was a novel approach to quantify what has become accepted correlation in adverse health outcomes.
- Ryan Howells, Dave Lee, and Stuart Venzke led discussions on Data & Technology, diving into updated federal regulations that present both opportunities and challenges for stakeholders, as well as ways to create corporate strategies that include data and technology, as these issues are no longer optional for anyone in this business. The breakout discussions talked about where we are today vs where we need to be – bridging the gap between data and decision making.
Payment & Risk TOOLS ARE ALIGNING INFORMATION TO ACTION: Achieving meaningful risk-based contracts is possible but the details matter…mismatched data and information leads to unequal buying power, which cannot be the case in value-based care.
- Kelsey Stevens, Scott Malan, Hunter Schouweiler, and Kate de Lisle led discussions on Payment & Risk, including an exciting hands-on simulation exercise that helped participants understand ways to increase premium scores by implementing risk-based payment approaches within the care delivery system; this session provided very concrete takeaways for those who attended by combining a simulation with a discussion on measures of success to improve risk-based contracting strategies.
- Amy Bassano and Kate de Lisle discussed their recent publication on the expanded ecosystem of value-based care entities, looking at the “enablers” who are working with providers and payers to manage risk. This groundbreaking landscape of this market segment highlighted a set of Guiding Principles to ensure these entities are aligned with CMS, provider, and patient goals. Participants had lots of questions for the presenters and were anxious to read the HMA full report.
CARE DELIVERY MEASURES MUST BE TANGIBLE TO PROVIDERS AND PATIENTS: Value-based care requires aligning the right metrics with the right incentives, ensuring providers understand not only WHY but HOW they help improve patient outcomes.
- Rachel Bembas, Dr. Jean Glossa, and Dr. Elizabeth Wolff led discussions on Care Delivery Measures, underscoring the importance of involving clinicians in the establishment of outcomes measures, as well as ensuring that the diversity of patient experiences are included. Participants remarked that we have a lot of “messy” data today, so we now have to ask the next set of questions on how we best use the messy data to make an impact?
- Former Congresswoman Allyson Schwartz talked about the continuing promise of Medicare Advantage, and the opportunity to convene a new alliance around Medicare quality metrics as well as the increasing pressure to align these metrics across payers. In the closing plenary, she said “We need to define what we want healthcare in America to look like and then go out and get it…. We have to align the measurements and the standards we use so that providers understand what’s needed and it benefits government, taxpayers, and beneficiaries…we should require plans to have risk-based contracting with providers.”
Policy & Strategy HAVE TO STAY THE COURSE TO ALIGN INCENTIVES: Policymakers can help or hinder movement forward to ensure success…value-based care has to be more than a section in an RFP, but part of the entire scope of paying for outcomes-based care delivery.
- Governor and former HHS Secretary Mike Leavitt reminded us of the political and policy journey that got value to where it is today, and the unique moment we are in right now that gives us hope as we enter this post-pandemic phase of healthcare spending and policy. He reflected, “We are beginning to see regulations and mechanisms to hold people accountable for healthcare costs…we have to integrate value and caregiving or we will never get to value.”
- Theresa Eagelson, former Illinois Director of Healthcare and Family Services, talked about the opportunity for states to expand value-based care by setting strong expectations through contracting and by thinking differently about policy choices. She reflected on the role of state administrators, “When we sit here and talk about value-based care, do we know what our north star is? Have we mastered what we want to see in RFPs (for Medicaid)? We’re working on a good FQHC model in Illinois, but should it be just for FQHCs? We need to spend more time together, across payers, across plans and providers and consumers to figure out what success looks like.”
- Caprice Knapp and Teresa Garate led a discussion on state and local Policy & Strategy to support integrated care and services that are required to achieve better outcomes. There is a need for services to better coordinate and manage care across social and health services, bringing contracting and payment expertise to more efficiently serve patients. The highly anticipated Medicaid managed care rule can help guide states in updating their approach. Federal analysis of Medicaid data is needed to set benchmarks before we can get to total cost of care approaches.
- Amy Bassano and AnneMarie Lauterbach led a discussion on federal policy alignment of Medicare FFS and Medicare Advantage, particularly looking at drug spending and the very real burden of medical debt as a driver of policy change. Participants reflected that half the country is indirectly covered through some public insurance. It’s just being done hyper-inefficiently.
HMA is leading the way on value-based care and is committed to continuing these dialogues to drive local, state, and national change. HMA’s value-based care expertise draws from our acquisition of Leavitt Partners and Wakely Consulting Group, two firms with deep ties and expertise on policy, strategy and risk-based pricing strategies, as well as recruitment of clinicians and operational experts who have led organizations through this transition. We will continue to advance the dialogue – and the work – to drive value as a critical way to ensure that our systems of health and healthcare are more affordable, equitable, and sustainable.
Let’s keep the conversation going! Learn more about how HMA can help you succeed with value-based payments and check out the newly released value-based payment readiness assessment tool for behavioral health providers.

State teams convene to strengthen collaboration across child welfare, behavioral health, and Medicaid
This week, our In Focus section highlights the Children’s Behavioral Health (CBH) State Policy Lab, held February 7−9, in Baltimore, MD. Health Management Associates, Inc., (HMA), in partnership with national philanthropies and associations, hosted the Policy Lab, which provided an unprecedented opportunity for state cross-systems teams to conduct in-depth work toward creating an equitable behavioral health system of care for children and youth.
Background
The lack of collaboration and misaligned strategies and policies across state child welfare, behavioral health, and Medicaid has contributed to unsatisfactory outcomes for children and youth in our communities. The COVID-19 public health emergency exacerbated these issues, as the rate of mental health and substance use disorders (SUD) increased and many families experienced traumatic events during this time. Increasingly, states and local jurisdictions are exposed to threats or actual class action lawsuits based on the inadequate care of children and youth involved in the child welfare settings.
Fortunately, federal and state efforts and investments to address the youth systems of care—including schools, community, delivery systems, and community-based child placing agencies—are in motion. Though the diversity of efforts being implemented across local and state agencies are critical, these complex issues require collaboration across multiple systems, including Child Welfare, Behavioral Health authorities, Medicaid, and K-12 Education. A cross-sector strategic approach will enable comprehensive identification of gaps, policy solutions, and best practices, as well as highlight opportunities for cross-sector braided or blended funding to build a system of care that supports the needs of multi-system children, youth, and their families.
Child Behavioral Policy Lab
The current behavioral health crisis presents an opportunity to address long-term challenges and divisions and to build a truly comprehensive approach. This is why HMA sponsored the Children’s Behavioral Health State Policy Lab which convened key partners within a state and across states. The Annie E. Casey Foundation, Casey Family Programs, National Association of State Mental Health Program Directors (NASMHPD), the Child Welfare League of America (CWLA), the American Public Human Services Association (APHSA), National Association of Medicaid Directors (NAMD) and MITRE, a Children’s Behavioral Health (CBH) State Policy Lab, joined HMA in funding, organizing and providing consultation support for the meeting.
The nine participating states—Georgia, Kansas, Kentucky, Maryland, Missouri, Pennsylvania, Texas, Utah, and Wisconsin—were selected through a competitive process based on the goals and commitment of the state and the thorough analysis of gaps and opportunities, demonstration of collaborative state interagency partnerships, and engagement of youth and adults.
The participating states committed their leadership teams to join the Policy Lab in laying the foundational work of development of statewide plans that would advance their collective goal of creating a more united system of care. Participants learned about intergenerational trauma and resilience. The sessions also provided participants with data that helped provide context to the problems we are trying to solve. Presenters included Aliyah Zeien, a national child welfare policy advocate and youth ambassador, with lived experience who highlighted that 25 percent of foster youth will spend time in prison or other enforcement systems within two years of leaving the child welfare system. Her experience and reflections served as call for action to actively engage families and youth in all system planning, advocacy, and policy work.
Key areas of focus
Following these brief educational sessions, each state had substantial “team time” to develop a road map and set of next steps for continuing their work after the Policy Lab. Expert facilitators guided state teams through discussions on three key issues:
- Service array. State teams were challenged to define their array of services and develop collective agreements on how to develop enhanced treatment options for children and their families. With an emphasis on building a full continuum of care with community-based supports and fewer children in residential facilities, each team considered challenges such as eligibility, access, and workforce. Prevention, diversion, and engagement of people with lived experience to help with system development were common commitments in state action teams.
- Financing. The teams considered their statutory authority, funding streams, funding partners, contract vehicles, and financing mechanisms. They also worked on ideas for blending and braiding funding, with a focus on Medicaid and leveraging collective opportunities to develop staff and contractual resources.
- Governance. State teams worked through difficult conversations, including how to measure success, how to manage accountability and monitoring, how to collaboratively design services and case practice, while meaningfully sharing data and creating interoperability within their systems while respecting confidentiality and privacy concerns.
What’s Next
Since the Policy Lab program, most participating states have embarked on next steps identified during the workshop, such as vetting their plans with state leadership, creating an ongoing team for implementation, and identifying community partners. HMA and HMA Companies, including Leavitt Partners, are collaborating with our Policy Lab partners and the state agencies to further develop these plans and prepare for implementations that rethink our approach to services for youth and their families.
For more information about the Policy Lab and follow-on work, please contact Uma Ahluwalia ([email protected]), Christina Altmayer ([email protected]), Jon Rubin ([email protected]), and Sarah Scholle ([email protected]).

March 20, 2024
State Teams Convene to Strengthen Collaboration across Child Welfare, Behavioral Health, and Medicaid

New Leavitt Partners report examines site-neutral payments
A new report by Leavitt Partners, an HMA Company, outlines the concept of site-neutral payment reforms being considered as a potential program improvement, and proposes a compromise approach to implementing site-neutral payments that benefits beneficiaries, hospitals, and the Medicare program. Site-neutral payments, which would equalize payment for the same services across all settings of care, are most commonly considered in connection with outpatient or ambulatory settings. Because out-of-pocket costs for Medicare beneficiaries are based on a percentage of the total reimbursement costs, any policy that reduces reimbursement for some services would result in savings to Medicare beneficiaries.
The approach proposed in the report lowers out-of-pocket costs to Medicare beneficiaries, improves the financing of the Medicare program by addressing a payment distortion, and reinvests in hospitals through new targeted funding and inclusion of policy priorities.

Federal policymakers consider current and future spending measures on simultaneous tracks
This week, our In Focus section covers Congress’s and the Administration’s parallel efforts to finalize fiscal year (FY) 2024 spending bills and begin the budget process for FY 2025.
Congress approved a bipartisan package for some of the FY 2024 spending bills, and on March 9, 2024, President Biden signed the Consolidated Appropriations Act of 2024 into law (PL 118-42). Programs funded through this measure include the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and other federal nutrition supports, rental assistance for safe and affordable housing, and veterans medical care and benefits.
Several mandatory funding extensions of public health programs and health-related policies also found their way into the 2024 consolidated appropriations package, including extending the Community Health Center Fund, delaying reductions in the disproportionate share hospital allotments, defining Certified Community Behavioral Health Centers (CCBHCs) as a Medicaid service, extending incentive payments for certain Medicare providers, and mitigating the impact of cuts to the Medicare physician fee schedule.
These policies, however, addressed a narrower set of issues than the expansive and bipartisan legislation that has been moving through both chambers of Congress. For example, House and Senate members have worked on respective bipartisan policies affecting price transparency, pharmacy benefit managers, and Medicare site-neutral policies, among others.
Meanwhile, President Biden released the FY 2025 Budget proposal March 11, 2024, kicking off the annual budget process. Like the administration’s FY 2024 budget proposal, the FY 2025 plan emphasizes deficit reduction and continues to make equity and Medicare solvency cornerstones of the budget. Health-related priorities include expanding access to affordable healthcare services, lowering drug costs, improving maternal health, addressing the mental health and substance use disorder crises, and enhancing biodefense and preparedness activities.
Check out the FY 2025 budget analysis from Leavitt Partners, a Health Management Associates, Inc. (HMA), company, and a deeper dive into the Consolidated Appropriations Act of 2024.
What We’re Watching
Congress is continuing negotiations on the outstanding spending bills, including the one that funds the Departments of Health and Human Services, Labor, and Education through September 2024. Lawmakers are working to reach an agreement before the next funding deadline of March 22.
The administration’s FY 2025 budget proposals are generally being characterized as a blueprint for President Biden’s re-election campaign and, if successful, a policy agenda for his second term. Though Congress has already begun holding hearings on the budget request, members on both sides of the aisle will likely focus on issues that resonate in an election year.
Regardless of the outcome of the November elections, Congress has an opportunity to address unfinished business during the lame duck session later this year.
HMA and Leavitt Partners collaborate to monitor legislative and regulatory developments in healthcare and adjacent spaces and to assess the impact of policy changes on the healthcare industry.

March 13, 2024
Federal Policymakers Consider Current and Future Spending Measures on Simultaneous Tracks

Medicaid managed care spending in 2023
This week, our In Focus section analyzes preliminary 2023 Medicaid spending data collected in the annual CMS-64 Medicaid expenditure report. After submitting a Freedom of Information Act request to the Centers for Medicare & Medicaid Services (CMS), HMA received a draft version of the CMS-64 report that is based on preliminary estimates of Medicaid spending by state for federal fiscal year (FFY) 2023. Based on the preliminary estimates, Medicaid expenditures on medical services across all 50 states and six territories in FFY 2023 totaled nearly $852.9 billion, with 59.6 percent of that amount now flowing through Medicaid managed care programs. In addition, total Medicaid spending on administrative services was $33.8 billion, bringing total program expenditures to $886.7 billion.
Total Medicaid Managed Care Spending
Total Medicaid managed care spending (including the federal and state share) in FFY 2023 across all 50 states and six territories was $508.1 billion, up from $468.3 billion in FFY 2022. This figure includes spending on comprehensive risk-based managed care programs as well as prepaid inpatient health plans (PIHPs) and prepaid ambulatory health plans (PAHPs). PIHPs and PAHPs refer to prepaid health plans that provide only certain services, such as dental or behavioral health care. Fee-based programs such as primary care case management (PCCM) models are not included in this total. Following are some key observations.
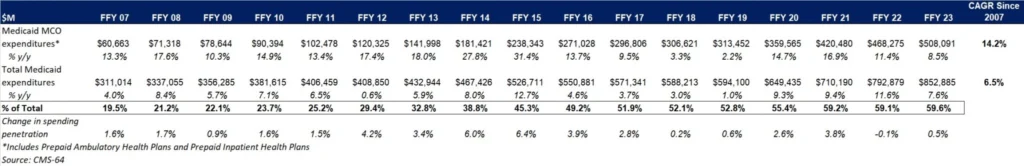
- Total Medicaid managed care spending grew 8.5 percent in FFY 2023.
- Managed care spending growth has decreased in since the end of the COVID-19 pandemic, after peaking in FFY 2021.
- In terms of dollars, the increase in Medicaid managed care spending from FFY 2022 to FFY 2023 was $39.8 billion, compared with $47.8 billion from FFY 2021 to FFY 2022.
- Medicaid managed care spending has increased at a compounded annual growth rate (CAGR) of 14.2 percent since FFY 2007, compared with a 6.5 percent growth in total Medicaid spending.
- Compared with FFY 2022, Medicaid managed care spending as a percent of total Medicaid spending in FFY 2023 increased by 0.5 percentage points to 59.6 percent.
Table 1. Medicaid MCO Expenditures as a Percentage of Total Medicaid Expenditures, FFY 2007−2023 ($M)
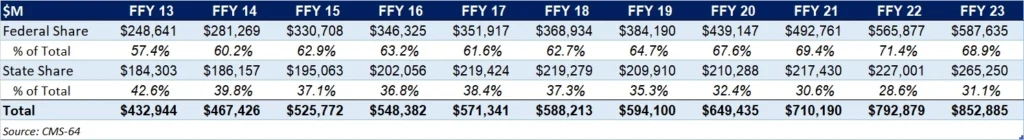
As the table below indicates, 68.9 percent of FFY 2023 spending came from federal sources, which is 11.5 percentage points higher than the pre-Medicaid expansion share in FFY 2013 and 1.3 percentage points higher than FFY 2020.
Table 2. Federal versus State Share of Medicaid Expenditures, FFY 2013−2023 ($M)
State-Specific Growth Trends
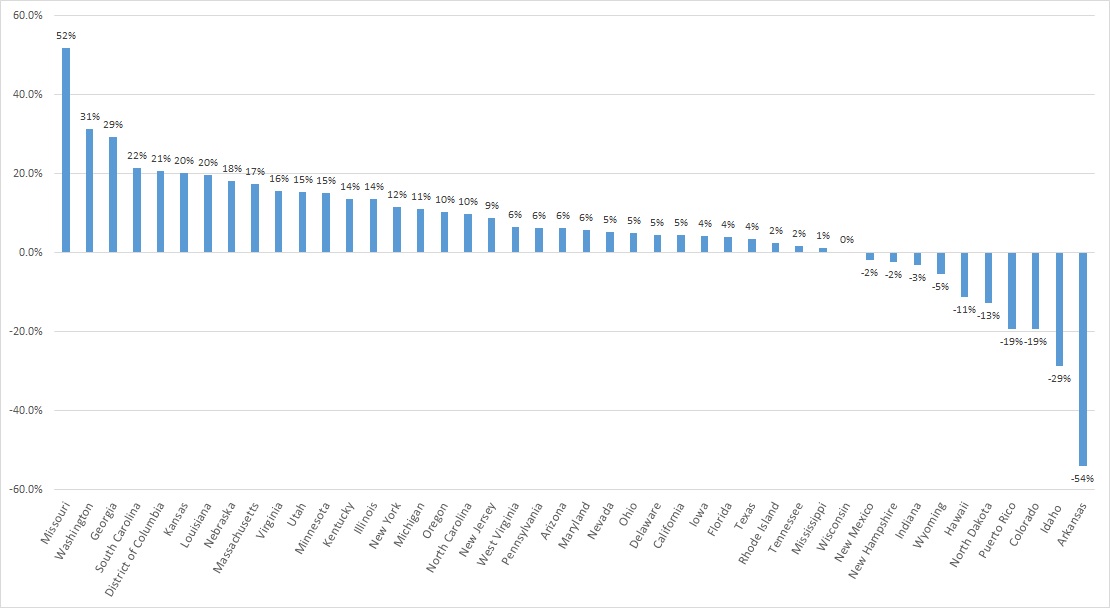
A total of 44 states and territories report managed care organization (MCO) spending in the CMS-64 report. Average MCO spending during FFY 2023 increased 8.5 percent. On a percentage basis, Missouri experienced the highest year-over-year growth in Medicaid managed care spending at 51.7 percent, followed by Washington at 31.4 percent and Georgia at 29.3 percent.
The chart below provides additional detail on Medicaid managed care spending growth in states with risk-based managed care programs in FFY 2023.
Figure 1. Medicaid Managed Care Spending Growth on a Percentage Basis by State, FFY 2022-2023
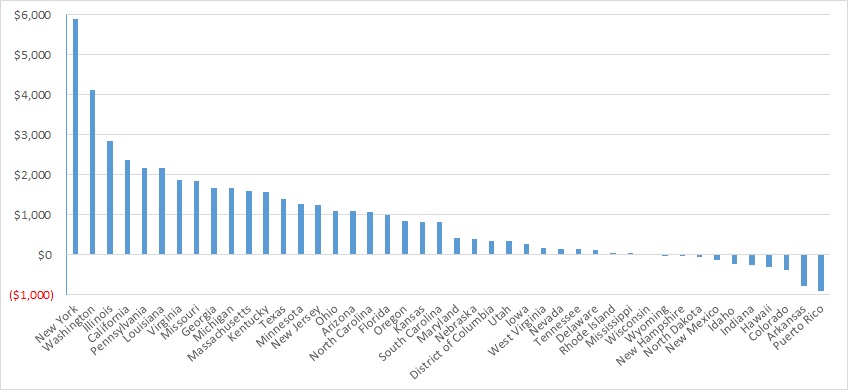
Looking at year-over-year spending growth in terms of dollars, New York experienced the largest increase in Medicaid managed care spending at $5.9 billion. Other states with significant year-over-year spending increases included Washington ($4.1 billion), Illinois ($2.8 billion), and California ($2.4 billion). The chart below illustrates the year-over-year change in spending across the states.
Figure 2. Medicaid Managed Care Spending Growth on a Dollar Basis by State, FFY 2022−2023 ($M)
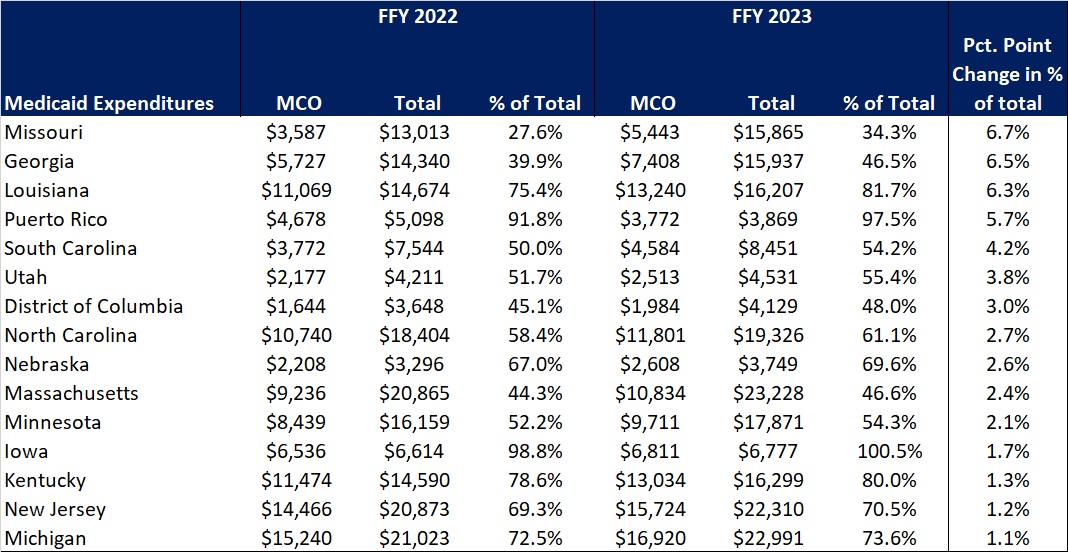
The percentage of Medicaid expenditures directed through risk-based Medicaid MCOs increased by more than one percentage point in 15 states from FFY 2022 to FFY 2023. The managed care spending penetration rate rose 6.7 percentage points in Missouri, 6.5 percentage points in Georgia, 6.3 percentage points in Louisiana, and 5.7 percentage points in Puerto Rico. In all, 22 states saw a decrease in managed care penetration from FFY 2022 to FFY 2023.
Table 3. Medicaid MCO Expenditures as a Percentage of Total Medicaid Expenditures in States with a One percent or Greater Increase from FFY 2022 to FFY 2023 ($M)
The table below ranks the states and territories by the percentage of total Medicaid spending through Medicaid MCOs. Iowa reported the highest percentage at 100 percent, followed by Puerto Rico at 97.5 percent and Kansas at 94.5 percent.
In many states, certain payment mechanisms may never be directed through managed care, such as supplemental funding sources for institutional providers and spending on retroactively eligible beneficiaries. As a result, the maximum achievable penetration rate in each state will vary and may be below the amount achieved in other states. The Medicaid managed care spending penetration rate is greatly influenced by the degree to which states have implemented managed long-term services and supports (MLTSS) programs.
Table 4. Medicaid MCO Expenditures as a Percent of Total Medicaid Expenditures, FFY 2016-2023
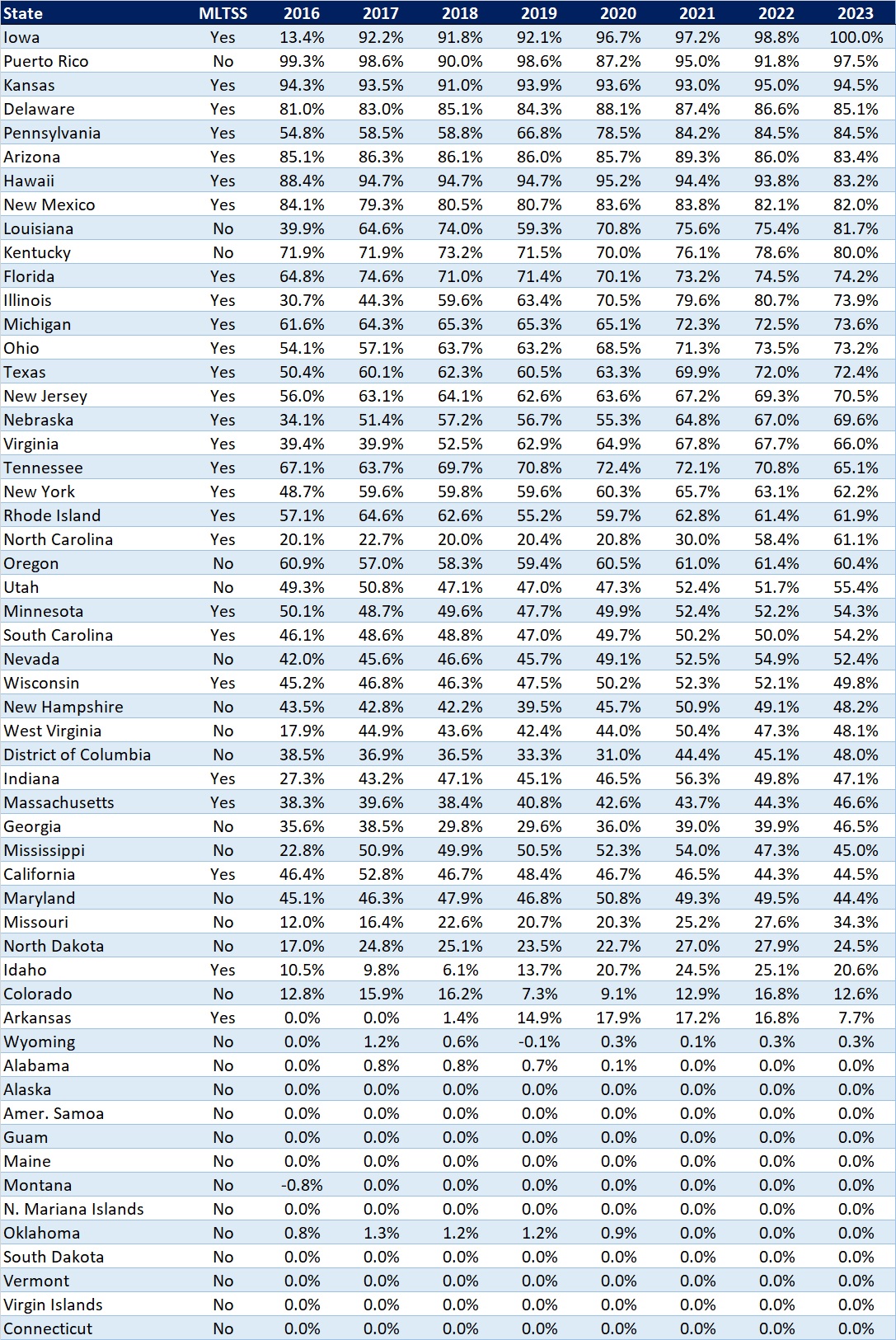
Note: Washington was excluded from the data table.
If you’re interested in becoming an HMAIS subscriber and for access to the CMS-64 data, contact Andrea Maresca at [email protected].

March 6, 2024
Medicaid Managed Care Spending in 2023

Privacy and Security Assessment and Support Services

One of the most important challenges for a health data organization is ensuring that its policies and procedures remain compliant with the dynamic landscape of federal and state privacy and security statutes, regulations, and industry standards.
HMA brings applicable experience and expertise to assist state agencies, non-profit organizations, and other entities that are responsible for all-payer claims databases, hospital discharge databases, and other datasets containing confidential and sensitive health data with:
Reviewing existing policies and procedures to identify gaps and needed updates to ensure compliance with regulations and adherence to best practices and industry standards.
Recommending revisions based on the assessment review and helping prioritize changes based on risk analysis.
Updating policies and procedures based on the approved recommendations.
Developing a training program for staff regarding the updated privacy and security policies and procedures via in person training, virtual training, and/or creating training videos.
HMA’s privacy and security assessment and support services capabilities include the following qualifications and expertise:
Holding leadership roles at state health data organizations and on the National Association of Health Data Organizations Board
Coordinating health information technology (HIT) for state Medicaid agencies
Leading state value-based purchasing agencies
Founding HIT strategic consulting firms
Experience with the National Association of County and City Health Officials
Project management and strategic planning support for multiple state agencies and data organizations
Privacy and security legal expertise
In addition, HMA offers the knowledge and experience of more than 700 consultants to supplement our privacy and security expertise with local healthcare knowledge and support to comprehensively address an organization’s needs.
Contact our experts:

Craig Schneider
Principal

