In honor of International Overdose Awareness Day (IOAD), August 31, 2023, we take time to pause and reflect on this year’s theme of “recognizing those people who go unseen.” HMA stands with those affected by overdose and promotes an ecological approach to addressing substance use, one that acknowledges the many facets of the crisis that leads to approximately 300 overdose deaths every day in the United States.
We recognize that many Americans experience the repercussions of overdose in ways that are often unseen: friends and family members who act as first responders by reversing an overdose with naloxone; seniors and older adults experiencing addiction; pregnant and parenting people who use drugs and/or medications for opioid use disorder; those who are often unable to access resources due to structural barriers such as homelessness or those living in rural and frontier communities; and, the justice-involved population, who serve as a salient example and often go unseen. Research has confirmed that overdose is the leading cause of death among people leaving carceral settings, as well as the third leading cause of deaths in custody in U.S. jails.
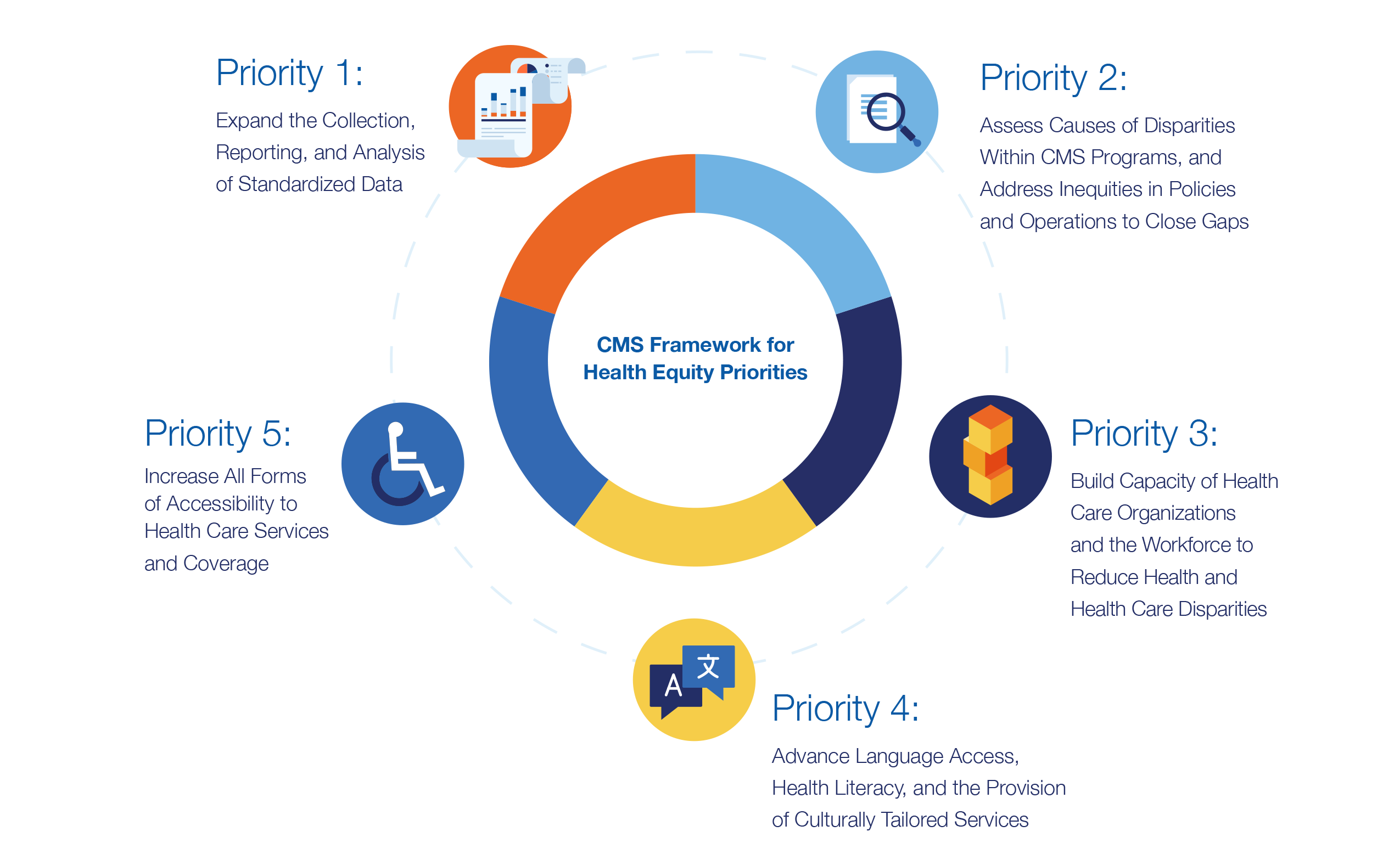
We also recognize that many of the racial disparities in U.S. overdose deaths are unseen and underrepresented in national dialogue about the crisis. At a time when people of color are dying at a higher rate than non-Hispanic White people, the International Overdose Awareness Day theme of recognizing those unseen is timely, and apt. Non-Hispanic American Indian or Alaskan Native people had the highest drug overdose death rates in both 2020 and 2021. Rates of overdose among Black or African American men outpace other groups. Racial disparities extend beyond overdose fatality rates and into the broader substance use disorder continuum of care. People of color are offered medications for opioid use disorder at a rate almost 50% lower than non-Hispanic White people, and the duration of their treatment tends to be shorter; ultimately leading to increased risk of returning to use. These statistics only reinforce the need for an expanded, comprehensive, and equity-centered approach to care.
Finally, we recognize that the overdose landscape is developing unseen changes, as overdose deaths involving psychostimulants such as methamphetamine are increasing with and without synthetic opioid involvement. Polysubstance use is the norm, not the exception. The healthcare sector must broaden and expand services to meet the current needs, including incorporating harm reduction strategies for stimulants, especially in states with high concentrations of deaths such as Nevada, West Virginia, Maine, and among non-Hispanic American Indians or Alaskan Natives.
HMA honors the often-unseen work and expertise of those leading advances in the field including peers, public health professionals, people who use drugs, and friends and family who become first responders. In remembrance of those impacted by overdose, our call to action is to honor unseen populations affected by this crisis, to elevate existing work by and for these communities, and to continuously seek innovative approaches that ensure we carry everyone forward into a responsive system of care.
Someone you know or may have seen may be struggling with addiction. Help is always available. The Substance Abuse and Mental Health Services Administration (SAMHSA) offers free, confidential, and 24/7 support in both English and Spanish at 1-800-662-HELP (4357).
For more information on HMA overdose prevention services, visit HMA’s Behavioral Health page.