
December 13, 2023
The Role of Specialized Managed Care in Addressing the Intersection of Child Welfare Reform and Behavioral Health Transformation
HMA Insights – including our new podcast – puts the vast depth of HMA’s expertise at your fingertips, helping you stay informed about the latest healthcare trends and topics. Below, you can easily search based on your topic of interest to find useful information from our podcast, blogs, webinars, case studies, reports and more.

The Role of Specialized Managed Care in Addressing the Intersection of Child Welfare Reform and Behavioral Health Transformation

HMA is pleased to welcome new experts to our family of companies in October 2023.
Dr. Anika Alvanzo is a distinguished healthcare executive with over 20 years of experience in specialty addiction treatment, behavioral health integration and quality improvement.
Kristine Malana Barrientos brings expertise in the Program of All-inclusive Care for the Elderly (PACE) senior leadership and operational experience from her work in California’s PACE market.
Craig Cartossa, ASA, MAAA, has expertise in Advanced Analytics, Healthcare Economics, Medicare Part D, Value Based Contracting, and Disease Management and Care Management Predictive Modeling and ID/Stratification. Read more about Craig.
Shannon Mayer is an impactful healthcare executive with over 30 years of experience. She is recognized for attaining results in Medicaid and Medicare Advantage’s highly regulated environments.
Cotrina McGue is a highly skilled information technology (IT) professional with over 35 years of experience and over 25 years specializing in healthcare systems.
Patricia Miles is a performance-driven managed care leader with over 25 years of experience in the Medicaid and Medicare markets.
Jason Pettry is a dedicated healthcare executive with over 10 years of experience with the Programs of All-Inclusive Care for the Elderly (PACE).
Corrie Piontak is a skilled healthcare professional with over 15 years of focused experience in management consulting, payer and provider strategy, and partnership strategy.
Aaron Ramthun is a financial professional with more than 20 years of experience working across the healthcare finance field, including Medicare bids, Medicaid rate book reviews, and budgeting. Aaron has a demonstrated track record of improving operational efficiency and implementing innovative forecasting practices.
Matt Smith, ASA, has experience with population health analytics, total cost of care analysis, value-based care contracts, financial modeling, pricing and reserving, and risk adjustment. Read more about Matt.

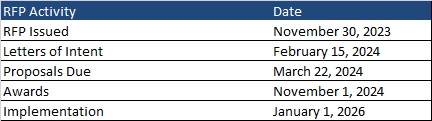
This week, our In Focus section reviews the request for responses (RFR) for the Massachusetts One Care and Senior Care Options (SCO) programs, released by the Massachusetts Executive Office of Health and Human Services (EOHHS) on November 30, 2023. The programs provide physical, behavioral, long-term services and supports (LTSS), and other community services to Medicare and Medicaid dual-eligible beneficiaries. Implementation is set to begin January 1, 2026.
One Care launched in 2013 as a Section 1115 Medicare-Medicaid Plan (MMP) program dual demonstration waiver. It operates under a financial alignment initiative (FAI) capitated model. The program provides integrated care to dual eligible adults ages 21 to 64. Individuals may remain enrolled in One Care when they turn 65 years old as long as they continue to meet all other requirements. Members can also access an independent LTSS coordinator.
As the Centers for Medicare & Medicaid Services (CMS) sunsets the FAI dual demonstrations, One Care will shift to a Fully Integrated Dual Eligible Special Needs Plan (FIDE SNP) beginning in 2026, pending federal approval of the Section 1115 amendment request. Members will have exclusively aligned enrollment with the same plan for both Medicare and Medicaid coverage.
SCO launched in 2004 and is currently a FIDE SNP with exclusively aligned enrollment. Medicaid enrollees ages 65 and older with or without Medicare are eligible. Enrollment in this managed care program is voluntary. Individuals on the Frail Elder Waiver can only join SCO.
Massachusetts will award separate contracts for One Care and SCO but may prefer bids from plans seeking to operate both; however, plans may submit bids to operate one type of plan. The state seeks to offer both One Care and SCO coverage for eligible individuals in as many counties as possible, and ideally statewide. Plans must propose to cover people in at least six counties for each type of plan.
To be selected, plans will need to have a contract with CMS to operate a FIDE SNP in Massachusetts in 2026. Applications must be submitted to CMS by February 2025.
Letters of intent are due February 15, 2024, and the deadline for responses is March 22, 2024. Plans will be selected by November 1, 2024. Implementation is set to begin January 1, 2026. Contracts will run an initial five-year term through December 31, 2030. Contracts may be renewed for up to five years in any increment.
Commonwealth Care Alliance, Tufts, and UnitedHealthcare serve 43,000 One Care members.
SCO incumbents WellSense Senior Care Options (formerly BMC Healthnet), Commonwealth Care Alliance, Fallon Health, Molina/Senior Whole Health, Tufts, and UnitedHealthcare serve 77,000 members.

Previously, Wakely Consulting Group, an HMA company, reviewed aspects of the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) requirements proposed rule published by the Internal Revenue Service (IRS), Employee Benefits Security Administration (EBSA), and Centers for Medicare & Medicaid Services (CMS) on August 3, 2023. The agencies accepted comments on the proposed rule through October 17, 2023. Because the proposed rule, if finalized as put forward, will have a significant impact on the compliance obligations of managed care organizations (MCOs) related to mental health parity requirements for the 2025 plan year in the group market and 2026 plan year in the individual market, MCOs will need to ensure, as they enter 2024, that they are in a position undertake any necessary steps to meet such obligations. This blog post outlines three specific requirements in the proposed the rule related to non-quantitative treatment limitations (NQTL) and their implications for a subset of MCOs: regional and local MCOs.
In the proposed rule, the IRS, EBSA, and CMS restate that MCOs may not apply any NQTL to mental health/substance use disorder (MH/SUD) benefits in any classification that is more restrictive, in policy or practice, than the predominant NQTL that applies to substantially all medical/surgical benefits in the same classification. To ensure compliance with this requirement, the proposed rule specifies exactly how an MCO must determine if the requirement is met.
First, the proposed rule outlines in detail how an MCO must complete a quantitative calculation to determine whether an NQTL applies to substantially all medical/surgical benefits in the classification at issue. If the NQTL does apply to substantially all medical/surgical benefits in the classification, the proposed rule then outlines exactly how the MCO must determine what version of the NQTL counts as the predominant one within the classification as well. Finally, once the predominant variation of the NQTL is established for an NQTL that applies to substantially all medical/surgical benefits in the classification, an MCO would have to use the proposed rule’s definition of “restrictive” (i.e., “imposes conditions, terms, or requirements that limit access to benefits under the terms of the plan,”) to determine if the NQTL applied to the relevant MH/SUD benefit is no more restrictive than the applicable medical/surgical benefit NQTL.
For local and regional MCOs, while the no more restrictive standard is not new, the steps required to ensure compliance likely represent—at the very least—an area where materially more intensive and sophisticated capabilities will need to be brought to bear. Completing the steps outlined above will require a cross-functional approach that leverages such areas as actuarial, behavioral health, clinical, compliance, financial analytics, and legal. The necessary people and processes will need to be deployed not only to accomplish the work effort but to do so in a way that is intelligible to federal and state regulators.
In the proposed rule, the IRS, EBSA, and CMS seek to make explicit a requirement which mandates that MCOs cannot impose an NQTL on MH/SUD benefits in any classification unless the factors used in designing and applying the NQTL to MH/SUD benefits in the classification are comparable to, and are applied no more stringently than, the factors used in designing and applying the NQTL to medical/surgical benefits in the classification. The agencies note that the regulatory revisions offered only seek to codify what has been a longstanding position of the agencies on this issue.
The most notable and innovative provision put forward by the agencies for purposes of determining comparability is one that would prohibit MCOs from relying on any factor in the design or application of an NQTL if the information on which the factor is based discriminates against MH/SUD benefits when compared to medical/surgical benefits. In this context, the proposed rule makes clear that discriminating against MH/SUD benefits means being biased or not objective, in a manner that results in less favorable treatment of MH/SUD benefits, based on all the relevant facts and circumstances.
For local and regional MCOs, it is advisable, given both the prudence of mitigating forthcoming potential compliance risks and likely limitations on the resources that can be devoted to compliance efforts in a discrete time period, to begin to evaluate upon entering 2024, whether NQTLs imposed on MH/SUD benefits have been designed and applied in a way that comports with this proposal by the agencies. For example, an MCO should evaluate whether factors currently employed rely on historical data or other historical information from a time when coverage was not subject to MHPAEA or was in violation of MHPAEA’s requirements where the use of such data results in less favorable treatment of MH/SUD benefits, as this would be prohibited. To this point, the agencies specifically note that MCOs would not be permitted to calculate reimbursement rates based on historical data on total spending for each specialty that is divided between MH/SUD providers and medical/surgical providers, when the total spending was based on a time period when coverage was not subject to MHPAEA or was in violation of MHPAEA, if the data results in less favorable treatment of MH/SUD benefits.
In the proposed rule, the IRS, EBSA, and CMS note that substantially disparate results are often a red flag that an MCO may be imposing an NQTL in a manner that does not comply with MHPAEA and so the agencies have included a proposal to add a requirement that, when designing and applying an NQTL, an MCO must collect and evaluate relevant outcome data in a manner reasonably designed to assess the impact of the NQTL on access to MH/SUD benefits and medical/surgical benefits as well as consider the impact as part of the MCO’s analysis of whether such NQTL complies with MHPAEA.
At minimum, MCOs would have to collect and evaluate data for all NQTLs that includes, but is not limited to, the number and percentage of relevant claims denials, as well as any other data relevant to the NQTLs as required by state law or private accreditation standards. Furthermore, due a specific concern of the agencies about network composition, the proposed rule would mandate that MCOs also collect additional applicable data for NQTLs that relate to network composition such as in-network and out-of-network utilization rates, network adequacy metrics (i.e., time and distance data and data on providers accepting new patients), and provider reimbursement rates. To the extent that data collected and analyzed demonstrates significant differences in access to MH/SUD benefits when compared to medical/surgical benefits, the MCO would be required to take reasonable action to address these differences in access as necessary to ensure compliance with MHPAEA.
For local and regional MCOs, beginning in 2024 to inventory readily available data sources that would be able to be leveraged to comply with this proposal is an important step in order to be prepared to comply during the 2025 plan year in the group market and 2026 plan year in the individual market. Additionally, assessing analytic capabilities to determine the level of readiness to be able to complete the evaluation based on the data collected is also an important component of preparing for this proposed new compliance obligation.
If you have questions about how HMA can support your efforts related to the proposed rule’s implications for local and regional MCOs, please contact our experts below.

HMA was engaged by the Washington, District of Columbia Department of Health Care Finance (DHCF) to lead their Medicaid Business Transformation D.C. Initiative, assessing the technical assistance needs of Medicaid providers and organizations in the areas of legal analysis, budgeting, and business development as they move toward value-based care arrangements. HMA partnered with the D.C. Behavioral Health Association (BHA), Medical Society of the District of Columbia (MSDC), D.C. Primary Care Association (DCPCA), and DHCF to engage, recruit, and collaborate with organizations and stakeholders across the District.
The HMA team implemented a mixed-methods assessment approach that included a literature review of national value-based payment (VBP) best practices, focus groups, interviews, and a technical assistance (TA) survey of District organizations, agencies, and stakeholders. This strategy identified the TA needs of District healthcare providers that informed the design of an intensive 3-month technical assistance program that included a variety of tools, webinars, and trainings. All resources and tools are available on the Integrated Care DC webpage. View the report and other information about the program published this week.
Experts from HMA as well as Wakely Consulting Group and Lovell Communications, both HMA subsidiaries, contributed to this report. We offer our clients a wide range of deep technical, analytical, policy, and communications support to providers, state agencies, and recommendations on ways to improve value-based payment models.
Report authors include Caitlin Thomas-Henkel, Suzanne Daub, Art Jones, Hunter Schouweiler, Amanda White Kanaley, and Vicki Loner. It was peer reviewed by Jean Glossa and Sam DiPaola.

This webinar was held on December 12, 2023.
Beyond the statistics lie the stories of countless children and families needing immediate and critical access to behavioral health services and community-based supports. Addressing these issues requires comprehensive cross-system reforms, including policies that promote integrated financing, enhanced care coordination, increased provider collaboration, and bolster upstream prevention efforts. HMA is working with these national partner organizations to prioritize and focus on cross system integrated and interoperable solutions to address the needs of children, youth, and families with complex behavioral health needs.
HMA hosted a webinar in partnership with the National Association of State Mental Health Program Directors (NASMHPD), National Association of Medicaid Directors (NAMD), Child Welfare League of America (CWLA), American Public Human Services Association (APHSA), and with support from the Annie E. Casey Foundation, Casey Family Programs and other funders. Together, these organizations have developed a multi-state policy lab to be held in February 2024. Applications for state agency participation opened the week of November 11th. State agency decision makers can click here to fill out and submit your state agency’s application. This webinar focused on the overall effort and for states to hear from this partnership on the importance of collaborating to strengthen the children’s behavioral health system.
If the link above to the online form causes problems or does not work for you, please use this fillable PDF application and send it to [email protected] with all relevant attachments. Applicants must submit the full application no later than 5 pm on December 20, 2023.
Key highlights of this webinar include:
Featured Speakers:
Julie Collins, MSW, LCSW, VP, Practice Excellence, CWLA
David Miller, M.P.Aff., Senior Operations & Project Director, NASMHPD
Sheila Poole, Vice President, External Relations, APHSA
Joe Ribsam, JD, Child Welfare and Juvenile Justice Policy Director, AECF

Proposed Changes to Opioid Treatment: What They Will Mean for Providers, Payers, and Regulators

Health Management Associates (HMA) collaborates with state and federal agencies, health service providers, and community-based organizations to enhance access to comprehensive reproductive healthcare and address disparities in birth outcomes, particularly in the context of Medicaid. This involves evaluating and supporting the implementation of perinatal care models, addressing health determinants affecting birth outcomes, and overcoming barriers to reproductive health services. In an effort to inform these initiatives, Diana Rodin, an associate principal at HMA interviewed Swedish experts to understand the country’s universal, publicly funded maternity and reproductive healthcare system. The Swedish model emphasizes universal healthcare, generous socioeconomic supports, and collaborative team-based perinatal care led by midwives. Lessons from Sweden, such as the utilization of “kulturdoulas” for culturally aligned support, a consensus-driven decision-making approach, and a centralized perinatal data system, provide valuable insights for improving birth outcomes for Medicaid recipients in the United States.


As we look back at our 2023 Fall Conference on publicly sponsored healthcare held in October, we wanted to highlight a few key takeaways from the event:
The discourse highlighted pervasive issues such as silos that contribute to a lack of accountability within the system. There was a unanimous recognition of the imperative to eliminate barriers to access, accompanied by a resounding call for a pivotal transformation in payer models. Throughout the session, a prevailing theme underscored the critical need for fostering collaborative efforts across different sectors, emphasizing the creation of opportunities for cross-sector groups to work together.
Participants echoed a shared sentiment regarding the urgency of dismantling the current lacking system and replacing it with a more inclusive, patient-centered approach. The session served as a platform for thought-provoking discussions, inspiring innovative solutions to address the challenges in behavioral health, paving the way for a more effective and accessible system.
The three main conference themes – Equitable Access, Digital Innovation, and Value-based Care – were touched upon in many of the panels and plenary sessions.
HMA is committed to bringing together experts from across the healthcare spectrum, and advancing the conversation about ways to improve access, equity, and innovation in healthcare. In early March 2024, we will be offering an HMA Spring Workshop on value-based care in Chicago. Registration will open soon; to receive the invitation, please be sure you are subscribed to the HMA News and Events list.

Minnesota Department of Human Services partnered with HMA to study Minnesota’s home- and community-based services (HCBS) trends; changes in its demographics, including the experiences of diverse communities; and successful local and national HCBS models to inform future efforts to improve access to supports for older Minnesotans and their informal caregivers. The report outlines recommendations to help address several of the challenges outlined in the brief, and identified several areas for DHS to consider for future innovations.
HMA has extensive expertise in HCBS and long-term services and supports (LTSS). If you would like to learn more about what HMA can do for your organization, you can contact the report authors Susan McGeehan, Barry J. Jacobs, Chris Dickerson, Aaron Tripp, Erica Reaves, and Anya Yermishkin.