In this week’s In Focus section, HMA Managing Director Matt Powers and Associate Principal Lora Saunders discuss observations and perspectives as we approach completion of the Medicaid unwinding.
Overview
In response to the COVID-19 pandemic, CMS offered states an enhanced federal match in exchange for states pausing Medicaid disenrollments. As a result, Medicaid enrollment increased from around 71 million at the start of the pandemic to more than 92 million in December 2022, when Congress passed a bill to end the “continuous eligibility” provision. States began to resume normal (pre-pandemic) redetermination activities in early 2023—a massive undertaking of attempting to reach and verify eligibility for the then 94 million Medicaid enrollees known as “unwinding.”
More than 70 percent of the efforts that will precipitate the largest one-year drop in enrollments since the program’s inception in 1965 have been completed. The enrollment reductions to date have been virtually identical to HMA’s aggregate projections, and overall enrollment remains well above pre-pandemic levels. Perhaps most importantly, the Medicaid unwinding has put policymakers in a position to better evaluate how to improve enrollment and redetermination processes going forward.
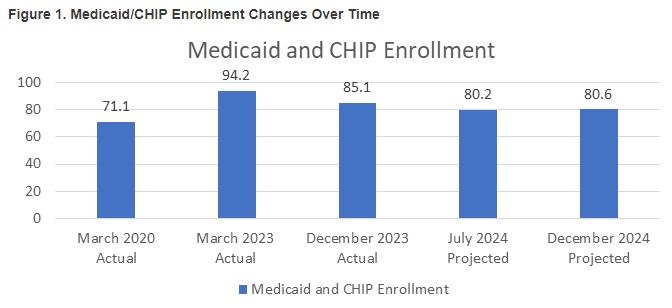
Figure 1 summarizes pre-pandemic enrollments, unwinding enrollments, and the projected end of 2024 enrollment. If the current trend holds, national Medicaid enrollment will be approximately 80 million enrollees—down from the 94 million pre-unwinding enrollment peak and nearly 10 million greater than the 71 million pre-pandemic enrollment.
Our team’s assessment of the status of and data related to the Medicaid unwinding has led us to the following observations:
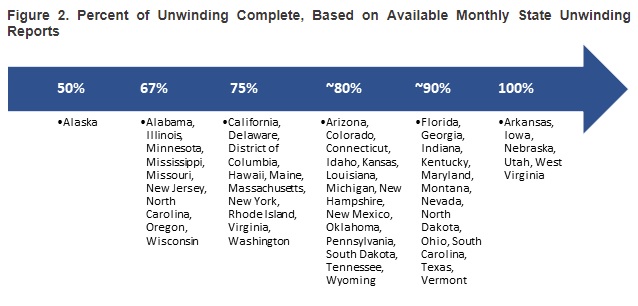
- Arkansas, Iowa, Nebraska, Utah, and West Virginia have completed the redetermination process. More than half of the states are within two months of finishing the process.
- The states that saw Medicaid enrollment grow the most under the continuous coverage policy are generally the same ones that are experiencing the greatest enrollment declines during the Medicaid unwinding.
- Some larger states—including California, New York, and Texas—have sizeable outstanding redeterminations.
- Nationally, more than 70 percent of all Medicaid enrollees have completed the redetermination process. Figure 2 points out how far along states are with the redetermination process as of late April 2024.
Medicaid Unwinding: The Road Ahead
As the Medicaid unwinding process enters its final phase in most states, we are looking back at the experiences and lessons that can be applied to make impactful changes to Medicaid eligibility policies, systems, and procedures.
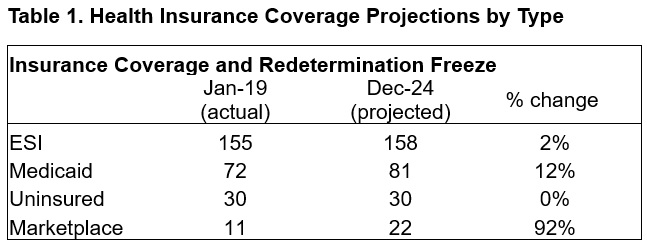
Despite the challenges that the pandemic presented, the safety net was tested and responded well. In early 2020, the number of employed Americans decreased from 158 million to 133 million, and unemployment levels quickly reached 15 percent. Many new healthcare policies targeted direct access issues (e.g., financial supports to providers and telehealth regulatory relaxations), whereas the Medicaid continuous coverage requirement was intended to mitigate the effects of the abrupt spike in unemployment and potential effects on healthcare insurance. Table 1 shows how HMA projects national coverage patterns to change by type of coverage from before the pandemic through the end of the Medicaid unwinding. While the number of people with employer-sponsored insurance (ESI) or uninsured remains essentially flat, Medicaid enrollment grows significantly, and marketplace enrollment nearly doubles. Myriad federal and state policy changes contributed to a remarkably stable uninsurance rate during one of the most volatile economic periods in the past century.
A next question for policymakers is whether, or to what extent, the rate of uninsured people can be sustained or reduced. The broad state adoption of policies to expand postpartum coverage to 12 months from two months and the nationwide January 2024 requirement for states to offer 12 months of continuous Medicaid coverage for children provide a coverage and continuity boost, especially given that nearly 40 million children will benefit from the new law. Other policy levers have the potential to be widely accepted and provide a further incentive to move people who are uninsured toward coverage, more stable insurance products, and more predictable outcomes and costs relative to the inefficiencies and ineffectiveness of non-coverage.
Pivoting to best practices and making policy changes permanent. Just as the relaxation of relatively rigid telehealth policies has become more accepted, post-Medicaid unwinding will provide a natural opportunity to assess best practices and consider permanent policy changes.
- Making Ex Parte Durable Policy. Evidence suggests that ex parte policies effectively reduce churn. Further refinement of longstanding ex parte policies is within reach. Ensuring ex parte appropriately manages both the complexities of household versus individual eligibility issues and addresses the weaknesses of unreliable member contact information can improve the likelihood that ex parte can effectively serve as durable policy.
- Pivoting from Paper to Electronic Communications. The Medicaid unwinding has seen more partnerships and innovation with state and federal workers, providers, managed care organizations, and consumer advocates, and allowed the increased use of mobile devices for outreach and engagement. Making more deliberate strides to simplify eligibility and move the eligibility platform, patient engagement, and member outreach to more reliable communication methods (e.g., email, text, and member portals rather than paper communication) while adhering to privacy and security requirements is a logical next step.
- Continuing to Measure Better. Call abandonment rates, call center wait times, and application processing times—metrics that focused on some of the key challenges to a successful redetermination and timely access to care—received greater attention during the unwinding but were frequently overshadowed by other primary metrics like “disenrollments” and “procedural terminations.” Though disenrollment data and procedural terminations could be used to identify potential areas of concern, their emergence as primary metrics often diverted energy from innovative engagement and redetermination efforts. A focus on contextualized metrics that provide actionable information will support effective oversight and monitoring.
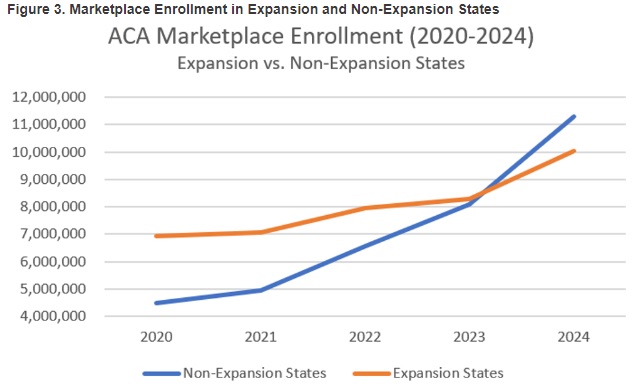
Marketplace growth may be the real story. Throughout the pandemic, marketplace enrollment has steadily increased, jumping nearly 90 percent from 2020 to 2024 and 30 percent from 2023 to 2024, to reach more than 21 million enrollees. Driving the growth in marketplace enrollment are temporarily increased marketplace subsidies and Medicaid unwinding public awareness campaigns.
- The marketplaces are proving to be a reliable source of coverage for consumers without health insurance access through ESI or other public programs, particularly in times of significant change such as the Medicaid unwind. With more marketplace enrollees and, therefore, broader risk pools, more health insurers are considering offering marketplace plans and are assessing competitive advantages like lower costs, broader provider networks, and more robust drug formularies.
- Figure 3 shows that marketplace growth in non-expansion states is far outpacing marketplace growth in Medicaid expansion states, suggesting that the key elements of the Affordable Care Act have developed deep roots.
HMA’s experts continue to monitor Medicaid unwinding developments. We are taking a comprehensive approach to assessing lessons learned and opportunities to improve Medicaid as state and stakeholder experiences and data continue to become available over the next two quarters.
For more information or questions about Medicaid unwinding developments, contact Matt Powers and Lora Saunders.
















































